Introduction
The coronoid process is a key-structure within the ulno-humeral articulation and one of the primary elbow stabilizers. Management of coronoid fractures has traditionally been challenging. The small fragment size, especially in cases of tip fractures or in the presence of comminution, the limited visualization due to the bulky flexor-pronator mass and the proximity of crucial neurovascular structures make coronoid fixation particularly problematic. Moreover, coronoid fractures rarely occur in isolation and are typically part of more complex injuries of the elbow, such as terrible triads, trans-olecranon fracture-dislocations, posteromedial rotatory instability or Monteggia like lesions, which are difficult to treat per se. In this context, failure to address correctly even subtle coronoid fractures may have a major impact on elbow stability and lead to poor clinical outcomes. The objective of this study is to review current evidence, provide a better understanding of traumatic elbow instability, identify the indications for coronoid fixation and guide the appropriate management of coronoid fractures in a holistic way, as part of specific injury patterns.
Anatomy and biomechanics
The ulnohumeral joint is a hinged ginglymoid articulation, between the trochlea and the greater sigmoid notch. It is inherently stable due to its high congruency with nearly 180° of articular contact throughout the full range of motion of the elbow.1–3 The coronoid process, pyramidical in shape, forms the anterior part of the greater sigmoid notch and accounts for about 60% of the anterior surface of the articulation with the humerus.4 It provides a bony buttress to posteriorly directed translation forces to the ulna, while it carries the attachment site for the anterior capsule (at an average of 5.9mm from coronoid tip), the brachialis tendon (volar base of coronoid) and the anterior bundle of the MCL (sublime tubercle).5,6 The coronoid consists of two different facets: (1) the anterolateral one, which articulates with the lateral trochlea and switches laterally to the lesser sigmoid notch and (2) the anteromedial one, which articulates with the medial trochlea. The anteromedial facet is wider and taller, protruding medially as a relatively unsupported by the ulna metaphysis structure.7,8 The anteromedial facet provides significant resistance to varus forces to the elbow.9 However, the lack of support by the ulna metaphysis renders the anteromedial facet prone to fracture.10
Along with the ulnohumeral articulation, the lateral ulnar collateral ligament (LUCL) complex and the anterior bundle of the medial collateral ligament (MCL) complete the triad of the primary stabilizers of the elbow. Secondary stabilizers include the radiocapitellar contact, the anterior capsule and the common flexor and extensor tendons. Muscles crossing the elbow, such as the anconeus, brachialis and biceps act as dynamic constraints.11–13
The relative contribution of coronoid to elbow stability has been extensively investigated. Early biomechanical studies suggested that ulnohumeral posterior displacement does not occur at any flexion position if more than 50% of the coronoid height is maintained.14 Beingessner et al.15 demonstrated increased varus-valgus laxity with increasing coronoid fragment in MCL-deficient specimens. However, laxity significantly decreased after repairing the MCL. Schneeberger16 et al. investigated how radial head (RH) excision and coronoid excision affected elbow stability. They showed that these elbows could be stabilized with RH arthroplasty alone only when<50% of the coronoid was resected. Jeon et al.17 concluded that deficiencies of up to 40% of the coronoid (type II) can be stable in the presence of intact ligaments. However, fractures involving >60% of the coronoid are associated with internal rotation and varus instability regardless of the integrity of the RH. In any case, the actual contribution of the coronoid is very difficult to assess and depends on the integrity of the rest of the stabilizers and the position of the forearm (both flexion-extension and prono-supination). More importantly, in most cadaveric studies, the specimens are subject to one direction forces, usually posteriorly directed, while in vivo instability manifests in a more complex plane.
Classification
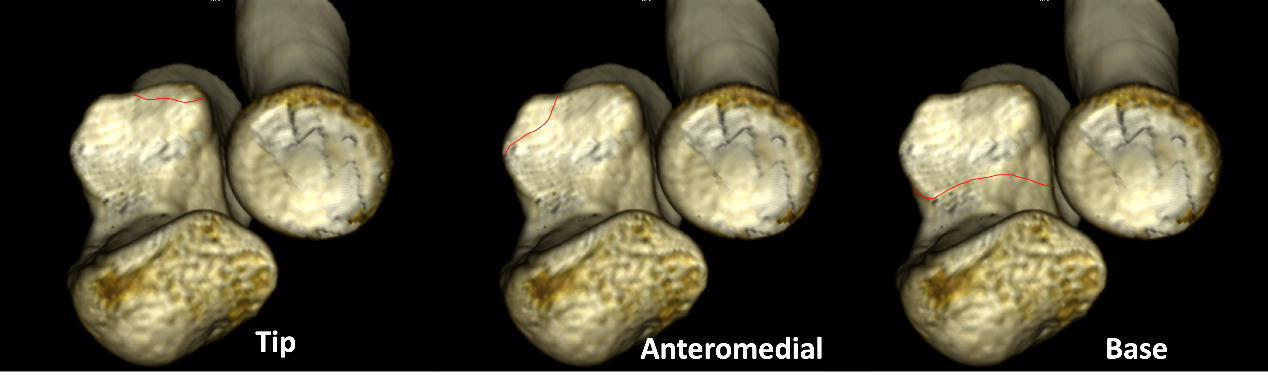
Regan and Morrey18 were the first to classify coronoid fractures, based on the fragment size: type 1 represent avulsion fractures of the tip, type 2 include fragments of less than 50% of coronoid height, while fractures larger >50% are characterized as type 3. Although simple and reproducible, moderate agreement exists regarding the definition of coronoid height. Moreover, O’ Driscoll et al.19 realized that fracture morphology and location should also be incorporated into a new classification system, since the fragment size alone does not have a prognostic value and cannot guide treatment. So, they identified three different types: 1) tip fractures, 2) anteromedial facet, and 3) basal fractures (fig.1). Type 1 are furtherly subcategorized as < 2mm (type 1a) or > 2mm (type 2b). Type 2 are subdivided in those including only the anteromedial rim (type 2a), those with rim plus tip (type 2b) and those with anteromedial rim plus sublime tubercle (type 2c). Finally, type 3 are subcategorized as body and basal (type 3a) and as trans-ulna basal fractures (type 3b). The importance of this classification consists in its association with the most common traumatic instability patterns. Recently, Adam et al. introduced the Wrightigton20 classification of elbow instability based on a three column concept. Although not a pure coronoid fracture classification, the Wrightigton classification provides a new perspective and a simplified algorithm to treat coronoid fractures.21 The osseous structures of elbow joint are divided in three columns: i) the medial column consisting of the anteromedial facet of the coronoid process and the medial part of the trochlea, ii) the middle column consisting of the anterolateral facet and the lateral part of the trochlea and iii) the lateral column consisting of the radiocapitellar joint. The medial column is the only restraint to varus stresses underlying the significancy of even small anteromedial facet fractures in varus-posteromedial types of injuries. The lateral column resists to valgus forces. Therefore, re-establishment of the radiocapitellar joint is the cornerstone of treatment in cases of posterolateral instability patterns, such as terrible triad. The middle column has a secondary contribution to valgus stresses and is less important in the case of a functional lateral column.
Diagnosis
Displaced coronoid fragments of a critical size are typically obvious on a lateral x-ray of the elbow, while small avulsion fractures of the tip or the anteromedial facet can easily be overlooked (fig.2a,b). The presence of an elbow dislocation should alert the surgeon even in the absence of apparent bony lesions. X- rays should be scrutinized for subtle coronoid or RH fractures, which are suggestive of more complex injuries. However, x-rays have only a moderate inter-observer agreement for diagnosing traumatic elbow instability patterns,22 while they are inadequate for pre-operative planning. CT scans are routinely necessary to diagnose and assess coronoid fractures, while the addition of 3D reconstruction significantly improves the inter-observer reliability with respect to the existent classification schemes.23 MRI is not routinely required pre-operatively, since soft tissue injuries are expected to occur in a predictable manner according to the injury pattern. However, MRI can be a significant asset when treating simple elbow dislocations24 to recognize the extent of soft tissue injury and probably identify surgical candidates.
Surgical approach
The coronoid can be approached from the medial side, from the lateral side (after RH osteotomy), directly anteriorly or arthroscopically. In the special case of a posterior fracture-dislocation, the coronoid fragment can be visualized through the fracture after reflecting the proximal olecranon fragment (fig.3) Each approach provides greater visibility to a particular part of the coronoid and should be selected based on fracture pattern, but also in association with other concomitant lesion. The extended medial approach (EMA) provides overall the greatest visualization of coronoid height, followed by the Hotchkiss interval, FCU-split and finally the Taylor-Scham approach.25 However, the Hotchkiss interval provides little or no exposure to structures posterior to the anterior bundle of the MCL, which are preferably approached either through the Taylor-Scham approach or the FCU split. On the other hand, the Taylor-Scham provides no visualization anteriorly to anterior bundle of the MCL. Finally, the FCU split gives access to both anterior and posterior structures of the MCL.25Thus, fractures of the anteromedial facet involving the sublime tubercle are preferably approached through an FCU split interval,26 while fractures of the anterolateral facet, as seen in terrible triads, can be reduced through the lateral approach and fixed indirectly with a PA screw or sutures. Otherwise, an over-the-top approach can give access to the tip. Finally, basilar fragments can be approached using a Taylor-Scham window, where the whole flexor pronator mass is sub-periostally elevated from the ulna. The direct anterior approach can provide visualization to the whole coronoid after splitting the brachialis tendon. However, the proximity of significant neurovascular structures and the difficulty to address simultaneously other soft tissue injuries have limited the use of this approach.
Treatment
Goal of treatment is the restoration of elbow stability, which is interpreted as the maintenance of a concentric reduction throughout a full range of motion. Moreover, stable fixation of the fractures is required to allow for early mobilization and avoidance of post-traumatic stiffness. Conservative treatment should be reserved either for i) unfit for surgery patients or for ii) carefully selected cases, where a concentric reduction of the elbow can be achieved and maintained with a brief period of immobilization. In this section, the management of coronoid fractures will be presented based on the O’ Driscoll classification and in association with the relevant injury patterns.
Type 1
Fractures of the tip of the coronoid typically occur as part of a terrible triad injury. Terrible triads result from a combination of valgus, axial compression and supination of the forearm producing a posterolateral dislocation of the elbow, fracture of the radial head and coronoid, rupture of the LUCL, with or without involvement of the MCL. Terrible triads represent severely destabilizing injuries, since most, if not all, of the elbow stabilizers are disrupted. Re-establishment of the radiocapitellar contact (either RH fixation or replacement depending on the fracture severity) and re-attachment of the LUCL to the lateral epicondyle are the cornerstones of treatment. The coronoid fracture line is typically transverse representing an avulsion fracture of the anterior capsule. The fragment rarely exceeds 50% of the coronoid height in size. Due to the typically small size of the fragment, a “lasso technique” of re-attachment of the anterior capsule with sutures passed through osseous tunnels through the ulna was described. Persistent instability after repairing of these three lesions was managed by addressing the rupture of MCL. However, recent advances in the understanding of elbow biomechanics have changed our treatment algorithm. Small coronoid fragments can be left untreated giving priority to MCL repair if instability persists.27 Indeed, clinical data suggest that that elbow stability and optimal functional scores can be achieved by fixing only fragments > 50% provided the collateral ligaments are repaired.28
Type 2
Anteromedial facet fractures comprise a distinct clinical entity that occurs as a result of varus posteromedial rotational forces. An avulsion of the LUCL is typically present rendering the ulnohumeral joint unstable. The MCL remains usually intact, except for the case of a true elbow disolcation.6 If neglected or not treated properly, the ulnohumeral joint is subject to varus stresses leading to rapidly progressing post-traumatic arthritis.29 Unlike those in terrible triads, anteromedial facets fractures may have a significant variability in size and pattern.30 They may be splits of the rim with articular depression or extend to the tip or the sublime tubercle. In some cases, they consist of a critical-sized single fragment, while in other cases significant comminution into multiple pieces is observed. Anatomic restoration and secure fixation are critical. Single fragments can be fixed either open or arthroscopically, while comminuted fractures are best treated with a low profile pre-shaped buttress plate typically placed through an FCU split approach. LUCL re-attachment to the lateral epicondyle should always be part of the surgery. Conservative treatment can be considered only in the special case of small (<5mm) – minimally displaced fragments provided that concentric ulnohumeral reduction is present on CT scan. Patients should avoid varus stresses, while close radiological monitoring is mandatory.6,29
Type 3
Basilar fractures usually occur along with trans-olecranon fracture dislocations wherein the humerus dislocates through a fracture of the olecranon. The fracture line usually includes the base of the coronoid and may extend to the ulna metaphysis. Despite the complexity and comminution of the proximal ulna, these injuries are characterized by less severe soft tissue injury, with the collateral ligaments kept intact in most cases. The presence of a fragment involving the cresta supinatoris may represent a bony equivalent to LUCL injury and is not uncommon in our experience. The RH typically remains intact as well. The coronoid fracture consists usually of a large basal fragment, which can be secured using either free or through the plate postero-anterior screws. If indirect reduction of the coronoid cannot be achieved, a Taylor Scham approach is indicated where the whole flexor-pronator mass is sub-periostally elevated from the ulna giving better visualization to the coronoid base. Due to the osseous nature of the lesion, these injuries are usually associated with better prognosis compared to terrible triads, in terms of functional scores and re-operation rates. Posterior olecranon fracture dislocations are less common injuries combining fracture of the RH, the coronoid and olecranon and elbow dislocation. They are characterized by a greater diversity in fracture pattern. The coronoid may be a large basilar fragment or separated fragments of the anteromedial facet, the tip and the sigmoid notch may be encountered.10 Proximal reflection of the olecranon fragment provides good visualization of the joint and allows for manipulation of the coronoid fragments. Indirect fixation using a postero-anterior screw is feasible in some cases of a single critical sized fragment. In case of comminution, an anterior buttress plate is usually required, placed preferably through a separate FCU split window (fig. 4a,b). Radial head is typically fragmented as well, requiring either fixation or replacement. As final step, the olecranon fracture is closed and secured with a single or double plating technique and the LUCL is repaired. Finally, posterior Monteggia-like lesions present with atypical fracture of the proximal ulna and RH fracture. Ulnohumeral stability is usually not compromised, and attention should be paid to restore the normal radioulnar relationship. The coronoid, if involved, is usually a large basilar fragment, which can easily be secured with screws through the posterior plate.
Discussion
Our notions about coronoid fracture management have changed a lot over the last decades. Early classifications schemes18 were based exclusively on fragment size, while biomechanical studies identified 50% of the coronoid as a crucial cut-off value for elbow instability.14,16 However, we have been taught that size alone does not predict elbow instability in the clinical setting, mainly for two reasons. The first one is that fracture morphology and topography may be more important than size. Secondly, each fracture occurs in association with a specific injury pattern and is accompanied by different soft-tissue lesions. O’ Driscoll et al. managed to incorporate these factors into their classification, so that the three basic fracture types represent roughly the three basic complex instability injury patterns. It has been shown that terrible triads are associated with a type 1 coronoid fracture (97%), varus posteromedial rotatory injuries with a type 2 (82%), while type 3 occur in conjunction with trans-olecranon fracture dislocations (100%) or posterior fracture dislocations (87%).31 These findings suggest that proper recognition and classification of the coronoid fracture pattern predicts the overall injury pattern and subsequently acquires a prognostic value in the context of a specific treatment algorithm.
The decision to fix or not a coronoid is complex. Even in the setting of a grossly unstable elbow, coronoid fixation does not always add significantly to the restoration of stability. A small avulsion fracture of the tip may be part of a severely unstable injury, as in the case of a terrible triad. However, it seems that RH fixation and repair of LUCL and possibly of anterior band of MCL effectively restores stability, thus obliterating the need for coronoid fixation.27,28 Kim et al.28 achieved excellent results in a case series of 27 patients with terrible triad injuries without addressing the coronoid at all except for basal fractures. Kaneshiro et al.27 concluded that priority should be given to MCL repair rather than fixing small coronoid fragments in terrible triads. Similarly, minimally displaced type 2a anteromedial facet fractures have been effectively managed with LUCL repair alone.32 While addressing every possible source of instability may sound as a reasonable decision, it may have an adverse clinical impact. Post-operative stiffness, surgical time and potential intra- or post-operative complications should always be considered. Therefore, it is crucial to recognize when coronoid fixation is imperative to regain elbow stability and when stability can be achieved indirectly by repairing the rest of the stabilizing components. Probably, the three-column concept classification20 helps to distinguish between those cases. The rationale is that restoration of medial and lateral column is sufficient to restore stability. Fractures limited to the anterolateral facet, as those usually seen in terrible triads injuries, can conditionally be left untreated as long as RH and LUCL have been repaired. On the other hand, bi-facet fractures, as those in Monteggia variants or posterior fracture-dislocations involve both the medial and middle column and require fixation. In any case, pre-operative classification and recognition of the injury pattern are very useful assets to guide treatment, but the decision to fix the coronoid or not should be made intra-operatively.
Fixation method depends on fragment size, topography, comminution, and concomitant soft tissue and bony lesions. As mentioned previously, large basilar fragments in trans-olecranon fractures-dislocations are usually secured with posteroanterior screws, while for very small avulsion fractures, capsular reattachment with sutures, anchors or lasso technique have been utilized. However, the necessity to address those fractures is now considered to be uncertain. More complex fractures especially with medial extension are preferably fixed with a plate. Klug et al. reported excellent MEPS scores using an anatomical buttress plate for the management of coronoid fracture in a cohort of 24 patients. Still, 5 patients had required an arthrolysis due to post-traumatic stiffness. Arthroscopically assisted fixation is an emerging procedure allowing for coronoid repair without the need for extended dissection. Oh et al.33 achieved similar clinical outcomes with arthroscopy vs open technique, but a lower complication rate was observed in the arthroscopy group. Still, the role of arthroscopy and its limitations in complex elbow instability require further research.
Chronic post-traumatic coronoid deficiency, secondary to significant comminution and/or poor initial treatment, can be complicated by persistent instability and early post-traumatic arthrosis.34 In this situation, a reconstruction procedure with a structural osteochondral graft is typically indicated. Most commonly, the graft is harvested from remnants of the radial head (if to be replaced) or the olecranon tip. Other potential graft sources include tri-cortical iliac crest, navicular bone, costochondral joint ends or distal clavicle.34 The goal is to restore a near normal coronoid height (normal values: 13-19.6mm) and olecranon-coronoid angle (normal values: 18o-28o), which are crucial for a congruent and stable joint.35 Bone graft size plays an important role to prevent resorption and ensure optimal load distribution. A graft height of 15mm seems to be sufficient in most cases to ensure joint stability and function, while greater heights may adversely affect elbow flexion.36 Lastly, coronoid replacement with specially designed prostheses, either cemented or press-fit, has also been described with very few clinical data on the literature.34,37 Still, potential risks of aseptic loosening, degenerative changes of the trochlea or catastrophic failure of the construct must be furtherly investigated.
Future directions. A small portion of patients will develop late onset post-traumatic arthrosis despite an initial concentric reduction and clinically stable elbow.38 It has been hypothesized that infra-clinical valgus instability may be responsible for this late onset arthritis in selected cases. Should we probably expand our indications to include routine MCL repair or small coronoid tip fractures in terrible triad injuries, especially in selected populations, such as young athletes? Could there be a role for post-operative 4d CT to recognize patients with subtle instability? Another area of future research is to clarify the indications of coronoid reconstruction in acute setting. Is there a place for acute coronoid reconstruction in severely comminuted fractures or should it be reserved for chronic cases? All these questions require further investigations with well-designed clinical and/or biomechanical studies.
Conclusion
Coronoid fractures are typically part of more complex injury patterns, each of them being associated with different soft tissue lesions and different prognosis. Proper recognition and classification of the coronoid fracture is a key step in order to identify the specific injury pattern correctly and treat both osseous and soft tissue injuries accordingly. In any case, the goal of treatment remains the achievement of a concentric reduction of the ulnohumeral joint and restoration of elbow stability, rather than coronoid repair itself.
Declarations
The authors have no relevant financial or non-financial interests to disclose.


_subtle_coronoid_fragments_can_easily_be_overlooked_on_initial_x_-rays_(yellow_arrow)_b).png)
_coronoid_as_seen_from_the_lateral_side_after_rh_osteotomy_in_case_of_a_terrible_triad_i.png)
_3d_image_of_a_posterior_ulna_fracture_dislocation_with_a_comminuted_coronoid_fracture_b.png)
_subtle_coronoid_fragments_can_easily_be_overlooked_on_initial_x_-rays_(yellow_arrow)_b).png)
_coronoid_as_seen_from_the_lateral_side_after_rh_osteotomy_in_case_of_a_terrible_triad_i.png)
_3d_image_of_a_posterior_ulna_fracture_dislocation_with_a_comminuted_coronoid_fracture_b.png)