1. Introduction
The emergence of patient-specific alignment techniques in Total Knee Arthroplasty (TKA) has renewed the longstanding interest of the orthopedic community on knee coronal alignment1–3 and has emphasized the importance of understanding and classifying its variations.4–6
Despite various methods for assessing coronal knee alignment, the gold standard remains the measurement of the mechanical axis using the hip-knee-ankle angle (HKA) from a weight-bearing full limb radiograph (FLR).7,8 Unlike standard short knee radiographs (SKRs), which capture approximately 10 cm of the distal femur and proximal tibia, FLRs provide a comprehensive view of the entire lower limb, aiding in the assessment of anatomical variations in the proximal femur and distal tibia. However, FLRs have drawbacks such as increased radiation exposure, specialized equipment requirements, and higher costs.
Consequently, many clinical studies have used the femorotibial angle (FTA) measured on SKRs to evaluate alignment, delineate “safety” boundaries and risk factors for failure in knee arthroplasty9 and still today many surgeons rely on SKR in their clinical practice, even for the analysis of post-operative outcomes.
The FTA definition varies greatly among different research papers, leading to various methods proposed for its measurement, both on fully-extended antero-posterior (AP) and semi-flexed postero-anterior (PA) SKRs. As a result, the FTA-HKA correlation is still a subject of ongoing debate, with a broad spectrum of values reported in the literature.10–13 To our knowledge, a systematic review on the subject has never been performed.
This study aimed to conduct a thorough review of existing literature to provide a comprehensive understanding of the relationship between FTA and HKA. Additionally, it aimed to perform a meta-analysis to quantify the FTA-HKA correlation comparing 1) the most commonly used methods for measuring FTA, 2) the method used to determine the knee’s center, and 3) AP vs PA SKRs. The hypothesis was that, irrespective of its definition and type of SKRs, FTA would not allow to predict the HKA in a substantial subset of patients.
2. Methods
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines have been utilized to carry out this systematic review.14
2.1. Eligibility Criteria
Only studies written in English and employing prospective or retrospective comparative designs were considered. All included studies examined the correlation between HKA measured on FLR and FTA measured on standard SKR. Exclusion criteria were applied to studies utilizing knee radiographs capturing more than 10 cm of the tibia and femur to assess the FTA.
2.2. Information Sources and Search
An electronic systematic search of PubMed (MEDLINE), Scopus and Cochrane databases was carried out by 2 reviewers, G.P and G.G., to identify eligible studies. The search was executed on November 12, 2023. The following search string was adopted: “hip-knee-ankle”[All Fields] AND (“angle”[All Fields] OR “angled”[All Fields] OR “angles”[All Fields]) AND (“diagnostic imaging”[MeSH Subheading] OR (“diagnostic”[All Fields] AND “imaging”[All Fields]) OR “diagnostic imaging”[All Fields] OR “x ray”[All Fields] OR “x rays”[MeSH Terms] OR “x rays”[All Fields]).
Then, a manual search of the bibliography of each published study was performed, to find relevant articles that could potentially have been missed. The remaining articles were analyzed by 2 reviewers, to exclude studies not fulfilling the eligibility criteria. Studies included were categorized by study type, according to the Oxford Centre for Evidence-Based Medicine.
2.3. Selection Process
For each study, the following data were extracted: epidemiological characteristics of participants (age, sex, type of knee, grade of OA, lower limb alignment), type of SKR (standing AP, semiflexed PA, FLR cropped to the dimension of SKR), FTA measurement method and FTA-HKA correlation.
The statistical analysis was conducted using R software, version 4.3.2. Meta-analyses were performed to pool the correlations between the most common FTA measurements and HKA and to establish potential differences depending on the method used to determine the knee’s center and the type of SKR used (AP vs PA). The results were reported as correlation coefficients and 95% confidence intervals (95% Cl). A random-effects model was used for I2 > 70%. Correlation coefficients were categorized as follows15,16: perfect (r = 1), excellent (0.9 ≤ r ≤ 0.99), very good/very strong (0.8 ≤ r ≤ 0.89), good (0.6 ≤ r ≤ 0.79), fair/moderate (0.4 ≤ r ≤ 0.59), weak (0.20 ≤ r ≤ 0.39), and neglegible (r <0.20).
2.4. Quality of the Studies
The quality of included studies was assessed using the MINORS (Methodological Index for Nonrandomized Studies) score.17
3. Results
3.2. Study selection and characteristics
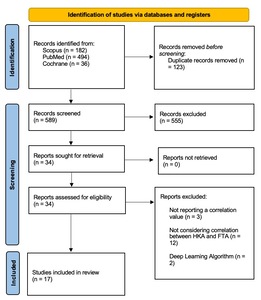
The literature search initially identified 712 papers, which were reduced to 589 after removing duplicates. Following the screening of titles and abstracts, 555 studies were excluded. Subsequently, the full text of 34 manuscripts was read, resulting in 17 studies that met the eligibility criteria for the systematic review. The PRISMA 2020 flow diagram outlining this process is depicted in Figure 1.
Details of the included studies are summarized in Table 1, encompassing a total of 2597 patients and 3234 knees. Of the 17 studies, 3 were prospective while the remaining 14 were retrospective. The mean age of participants was 60.4 years (range: 14 to 81 years). Additionally, the average MINORS score across studies was 10.2/16 (Table 1).
Demographic characteristics, FTA measurement methods and types of knee radiographs examined are reported in Table 2. The FTA-HKA correlation was analyzed on AP SKRs in 8 studies, on PA semi-flexed SKRs in 4 studies and on both in 1 study. Finally, 4 studies analyzed the correlation on AP FLRs cropped to the dimensions of a SKR. The alignment category was reported in 9/17 studies, comprising a total of of 816 varus, 350 valgus and 400 neutral knees.
3.2. META-analysis
In the 17 studies examined, 11 distinct methods of measuring the FTA were identified, as outlined in Table 2. For the purpose of result analysis, all methods that differed in the proximal point of the tibia (center of the base of the spines, center of the tip of the spines, and center of the tibial plateau) were grouped together, considering the differences negligible, thus resulting in a total of 8 methods (Table 2 and 3). Only preoperative data were included in the meta-analysis for studies that provided both preoperative and postoperative data.
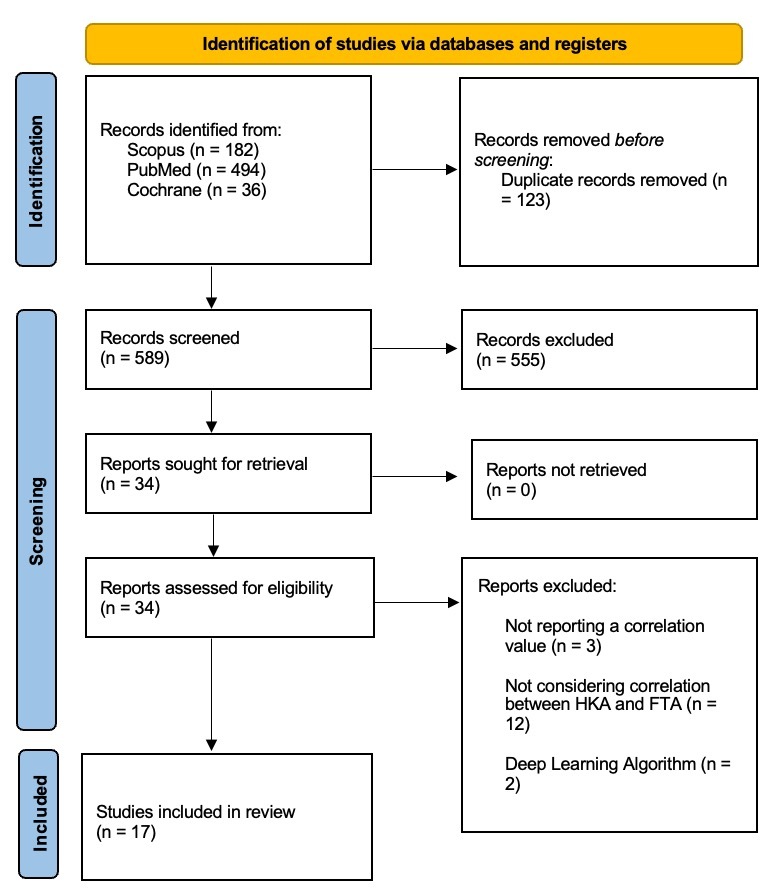
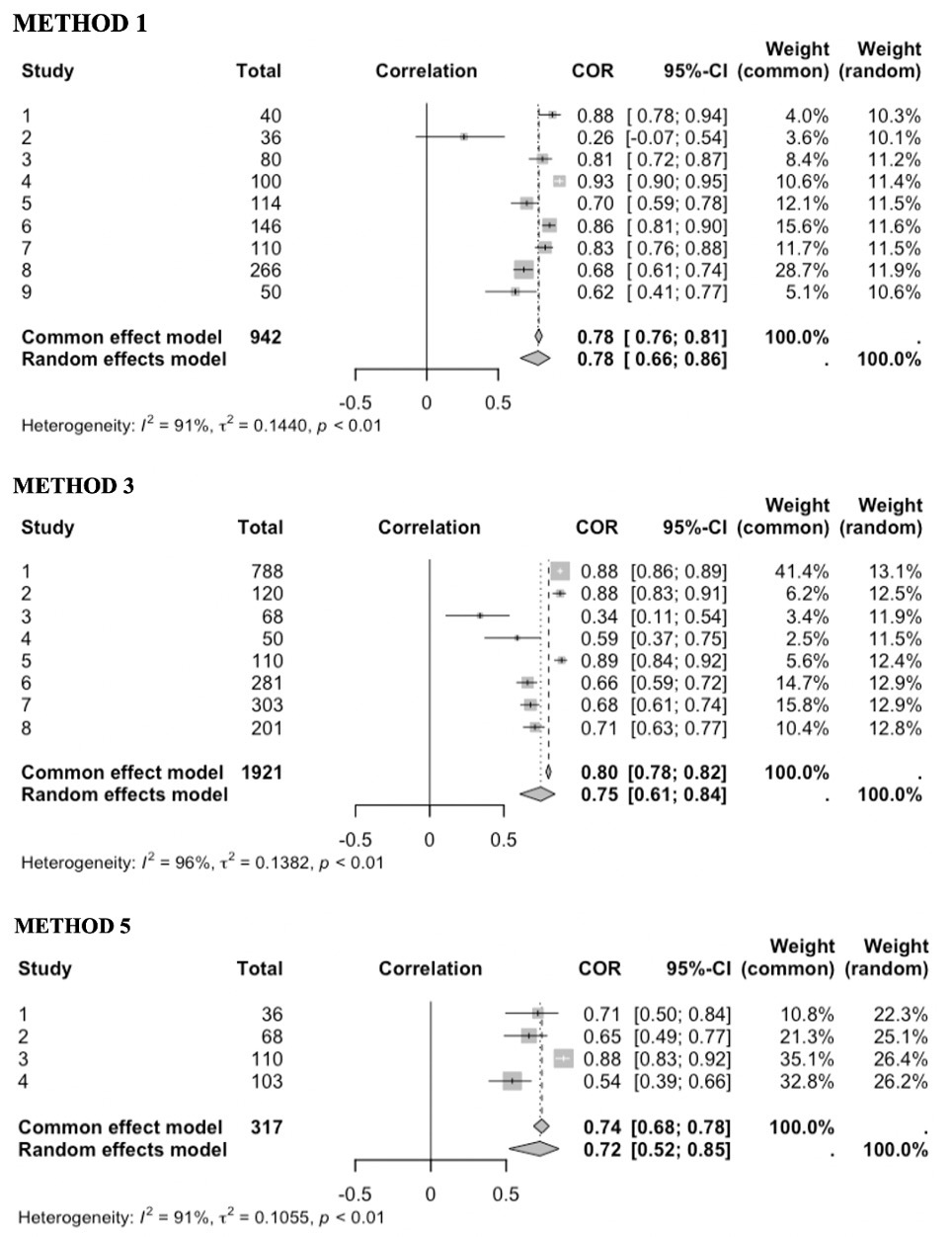
The 3 most commonly used FTA methods were Method 1, Method 3 and Method 5, evaluated in 9, 8 and 4 studies, respectively (Figure 2).
In Method 1 the FTA was defined as the angle formed by the intersection of a femoral axis drawn between (a) the femoral mid-shaft 10 cm proximal to the center of the tibial spines and (b) the center of the tibial spines, and a tibial axis drawn between (a’) the center of the tibial spines and (b’) the tibial mid-shaft 10 cm distal to the center of the tibial spines.
In Method 3 the FTA was defined as the angle formed by the intersection of a femoral axis drawn between (a) the femoral mid-shaft 10 cm proximal to the center of the femoral notch and (b) the center of the femoral notch, and a tibial axis drawn between (a’) the center of the tibial spines and (b’) the tibial mid-shaft 10 cm distal to the center of the tibial spines
In Method 5 the FTA was defined as the angle formed by the intersection of a femoral axis drawn between (a) the femoral mid-shaft 10 cm proximal to the center of the femoral notch and (b) the junction of the femoral meta-epiphysis, and a tibial axis drawn between (a’) the junction of the tibial meta-epiphysis and (b’) the tibial mid-shaft 10 cm distal to the center of the tibial spines
The FTA-HKA correlation coefficients were: 0.78 (95% CI: 0.66 to 0.86; I2 = 91%) for Method 1, 0.75 (95% CI: 0.61 to 0.84; I2 = 96%) for Method 3, and 0.72 (95% CI: 0.52 to 0.85; I2 = 91%) for Method 5.
The various methods were further classified into two groups based on their approach: those relying on a single reference point (Group I) and those utilizing two reference points—one for the tibia and one for the femur (Group II)—to establish the center of the knee (Figure 3). Group I, evaluated in 9 studies, showed a correlation coefficient of 0.78 (95% CI: 0.66 to 0.86; I2 = 91%), while, Group II, evaluated in 13 studies, showed a correlation coefficient of 0.77 (95% CI: 0.68 to 0.83; I2 = 95%).
Finally, a trend towards stronger FTA-HKA correlation was found when using AP vs PA SKRs in both Method 1 and Method 3 (Figure 4). In Method 1, 6 studies used AP SKRs with a correlation coefficient of 0.79 (95% CI: 0.60 to 0.90; I2 = 93%), and 4 studies used PA SKRs with a correlation coefficient of 0.75 (95% CI: 0.62 to 0.84; I2 = 87%). Similarly, in Method 3, 5 studies used AP SKRs with a correlation coefficient of 0.80 (95% CI: 0.60 to 0.90; I2 = 96%), and 3 studies used PA SKRs with a correlation coefficient of 0.66 (95% CI: 0.62 to 0.71; I2 = 0%).
4. Discussion
The main finding of the current study, gathereing results from 17 articles involving a total of 2597 patients and 3234 knees, was that, irrespective of its definition and type of short knee radiographs, the femorotibial angle fails to predict the hip-knee-ankle angle in a significant subset of patients. To the best of our knowledge, this represents the first systematic review and meta-analysis on this topic.
Although the FTA11,12,18–23 is commonly defined as the angle formed by the intersection of two lines drawn from the midpoint of the tibial spines to a point situated 10 cm above and below the joint line and midway between the cortical bone surfaces (Method 1), alternative definitions have been explored in the literature.13,21–30 Notably, the chosen FTA definition seems to significantly impact its ability to predict the HKA, as observed by Gielis et al.21 In their study, they compared the FTA-HKA correlations with 6 of the 8 methods considered in the current systematic review and found the best correlation (r = 0.93) for Method 4, which defines FTA as the angle formed by the intersection of a femoral axis drawn between (a) the femoral mid-shaft 10 cm proximal to the femoral notch and (b) the center of the femoral notch, and a tibial axis drawn between (a’) the junction of the tibial meta-epiphysis and (b’) the tibial mid-shaft 10 cm distal to the center of the tibial spines.
Therefore, a meta-analysis was conducted on the three most commonly referenced methods to measure the FTA. Our results revealed Method 1 as the most valid, exhibiting a correlation coefficient of 0.78. Additionally, similar correlation coefficients were found for Methods 3 and 5, with values of 0.75 and 0.72, respectively. Notably, even within a specific FTA method, the FTA-HKA correlation can vary greatly, with values spanning from 0.2618 to as high as 0.93.19
An essential aspect in understanding the FTA-HKA correlation among various FTA measurement methods is the choice of reference point used to define the knee’s center. In advanced knee osteoarthritis, some degree of femur subluxation on the tibia is often observed. Therefore, it might seem logical to anticipate that methods utilizing a single reference point would be less reliable compared to those employing two separate reference points—one for the tibia and one for the femur. However, our meta-analysis did not support this assumption, as it revealed very similar results between Group I and Group II.
Several studies have investigated the FTA-HKA correlation using semi-flexed PA SKRs,10,20,22,23,30 which reflect the knee’s loading position, instead of fully-extended AP SKRs. The only study directly comparing the FTA-HKA correlation using both types of SKRs was conducted by Kraus et al,20 revealing correlation coefficients of 0.65 and 0.75 when employing AP and PA SKRs, respectively. In contrast, our meta-analysis yielded a stronger mean correlation coefficient for AP SKRs compared to PA SKRs, with values of 0.79 vs 0.75 and 0.80 vs 0.66 for Method I and III, respectively. These results suggest that AP SKRs may be a preferable option for assessing the FTA-HKA correlation.
It’s crucial to acknowledge substantial discrepancies across the included studies of the current systematic review. The reported differences between FTA and the HKA vary widely, ranging from less than 111,12 to more than 7°.10,13,24,25 The heterogeneity of these results may stem from factors other than variations in FTA measurement methods and type of SKR used, such as presence, direction and degree of femoral/tibial bowing or other extra-articular deformities,31 direction and degree of lower limb malalignment,25 sex,10,13,20 pre- vs post-operative state,18,28 and sample size across different studies.
Significant femoral and/or tibial bowing, present in a varying percentage of the population,32,33 can significantly impact the predictive accuracy of FTA for HKA, as highlighted by Oh et al.31 Their study revealed a twofold increase in the rate of misalignment categorization in knees with bowing compared to those without (26.2 vs. 13.1%). Incorporating a longer shaft length in the SKR could potentially capture the presence of extra-articular deformity, offering an explanation for the heightened FTA-HKA correlation observed by Chang et al13 when utilizing 15 cm shaft length, compared to the standard 10 cm. Similar results were also reported by Park et al28 and Sheehy et al.25
Additionally, research suggests that the FTA-HKA correlation may vary depending on the type of alignment and the severity of deformity, as demonstrated by Sheehy et al25 In their study, they found that using a shorter shaft length for assessing the FTA resulted in an increase in the FTA-HKA offset in varus limbs and a decrease in valgus limbs. Furthermore, inconsistent findings regarding offsets between HKA and FTA have also been reported between males and females in previous studies.10,13,20 While some authors10,20 reported a smaller offset in the female population, ranging from 3 to 3.5°, Chang et al13 reported opposite trends.
Various efforts have been undertaken to derive the HKA from the FTA through predictive equations.11,13,20 However, their reliability and external validity appear to be limited, likely as a consequence of the small sample sizes, as pointed out by Stickley et al.26 Indeed, their findings indicate that, when applying the gender-specific equation from Chang et al13 and the generalized equation from Kraus et al20 to 788 consecutive cases, they accurately predicted HKA within ±3° in only 61% of males and 63% of females, and 36% of males and 44% of females, respectively.
Finally, the predictive ability of the FTA for determining the HKA also appears significantly influenced by whether pre-operative or post-operative images are analyzed. In the TKA population, Park et al28 observed a more than twofold increase in the misclassification rate of patient alignment when using post-operative compared to pre-operative images (33.0 vs 13.9%), coupled with a lower FTA-HKA correlation (0.69 vs 0.90). Conversely, in a high tibial osteotomy population, Zampogna et al18 found that the FTA-HKA correlation was higher for post-operative compared to pre-operative images for both methods considered (FTa1: 0.53 vs. 0.26; FTa2: 0.79 vs. 0.71).
Our findings support the hypothesis that FTA lacks reliable accuracy in predicting the HKA in most knees. Moreover, inconsistent boundaries have been reported in the literature for categorizing alignment as neutral, varus or valgus based on the FTA values,9,34,35 thus limiting its utility also for broader analytical purposes, as shown by Shang et al.29 Therefore, we advocate for the use of FLRs whenever precise estimation of the patient’s alignment is necessary. Additionally, caution is advised in interpreting studies investigating knee alignment or outcomes after knee arthroplasty procedures based on FTA.
The findings of the present study need to be considered in light of its potential limitations. The considerable heterogeneity of the populations among the studies in terms of age, sex, type of alignment and presence vs absence of knee osteoarthritis, underscores the need for a cautious interpretation of the results. Additionally, a high level of heterogeneity was observed within the results of the meta-analysis, with the I2 exceeding 85% in nearly all reported correlations. Finally, the limited number and low evidence level of included studies, mostly categorized as level IV, as well as variations in FTA-HKA offsets, predictive equations, and FTA definitions, pose challenges in comparing results and may introduce bias in the absence of subgroup analysis.
5. Conclusions
Irrespective of the its definition or type of SKR used, FTA lacks reliable accuracy in predicting the HKA in most knees. The variability in offset between HKA and FTA is unpredictable and highly influenced by inter-individual factors. Full-length radiographs should be used whenever precise estimation of the patient’s alignment is necessary. Additionally, caution is advised in interpreting studies investigating knee alignment or outcomes after knee arthroplasty based on FTA.
Corresponding author
-
Name: Pietro Gregori
-
Institutional address: Research Unit of Orthopaedic and Trauma Surgery, Department of Medicine and Surgery, Università Campus Bio-Medico di Roma, Roma, Italy
-
Phone: +393400951122
-
Email: Pietro.gregori@unicampus.it
Authors’ contribution
RP had the idea for the article. GG was responsible for data acquisition, data analysis, and the writing of the manuscript. GP was responsible for data acquisition. GFP was responsible for data analysis. UGC and BZ were responsible for grouping the FTA methods with uniform definitions. EF, SC, and PG were responsible for reviewing and critically revise the manuscript. All authors have given final approval of the version to be published.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare that they have not conflict of interest.