Introduction
Developmental dysplasia of the hip (DDH) is a common orthopedic disorder.1 If it is not treated properly, it may lead to subluxation, dislocation and eventually degenerative joint disease.2,3 Early diagnosis offers the chance of a more effective management. However, this is not always the case specially in the developing countries where the screening programs are not well-established. Consequently, the diagnosis is frequently delayed and a more complex intervention with a variable degree of success is required. Open reduction is preferred over closed reduction after the age of 16-20 months as the latter was found to be associated with an unaccepted rate of avascular necrosis after this age.4–6 The acetabular remodeling capacity in response to a successful reduction declines with age.7,8 Based on that, a pelvic osteotomy as an adjunct to open reduction, becomes more essential the older the child.9–11 In cases of dysplasia without subluxation or dislocation, a pelvic osteotomy can be undertaken without an open reduction. Another adjunct procedure is a proximal femoral osteotomy which could involve shortening, varus and/or derotation. Pelvic osteotomies include several types. They can be divided into 2 groups, complete and incomplete transiliac osteotomies. Complete transiliac osteotomies include those introduced by Salter,12 Steel13 and Sutherland.14 The first account on incomplete transiliac osteotomy was written by Albee15 in 1915 who described a semicircular cut of the acetabular rim directed from the lateral to the medial cortex in an oblique way. The best known incomplete transiliac osteotomy is Pemberton’s.16 It starts 10 to 15mm above the anterior inferior iliac spine and curves posteriorly to end at the level of the ilioischial limb of the triradiate cartilage. It hinges at the triradiate cartilage but it may also hinge at the symphysis pubis. The Pembersal osteotomy was described by Perlik17 and is similar to Pemberton’s osteotomy except that it crosses the ilioischial limb of the triradiate cartilage and extends to the body of the ischium. It is assumed that it provides a better acetabular redirection and reshaping; however it carries a potential of growth arrest of the triradiate cartilage.
Dega osteotomy18,19 was introduced in 1969. It is an incomplete transiliac osteotomy that involves cutting the outer as well as the anterior and middle portions of the inner cortices of the ilium leaving a hinge that is formed by the intact posteromedial cortex. The original account and the subsequent reports from the Dega’s institution did not provide an elaborate description of the surgical technique.
The aim behind this paper includes several folds. We would like to provide a clear description of the procedure as there was some debate on what constitutes a Dega osteotomy. We also aimed at exploring how many pelvic osteotomies were planned as a Dega osteotomy but were implemented as different osteotomies due to limited intraoperative exposure. We also wanted to examine how effective Dega’s osteotomy is in improving a dysplastic acetabulum in DDH in quantitatively. Lastly, we tested the effect of certain technical steps on the final change in the acetabular coverage including the starting point of the bony cut, the inclination and the relation to the arcuate line of the pelvis and the ilioischial limb of the triradiate cartilage.
Methods and Materials
This is a retrospective radiographic and case note review study. We reviewed the records, plain radiographs and CT images of patients with DDH who were treated operatively by Dega osteotomy.
The spectrum of the cases included acetabular dysplasia, hip subluxation and dislocation depending on the Shenton’s line, the acetabular roof index and the loss of articulation.
The Dega osteotomy was either performed as a primary procedure (simultaneously with an open reduction) or as a secondary procedure (some time period after an open reduction being effected). In cases of acetabular dysplasia without subluxation or dislocation, a Dega osteotomy was performed without an open reduction.
Open reduction was undertaken for all cases of subluxation or dislocation. Femoral osteotomy was used for all cases where shortening was needed or there was an excessive neck shaft angle and/or anteversion.
The period of the study started from October, 2018 onward. The inclusion criteria included patients at walking age, the availability of the pre and postoperative clinical and radiographic data including a postoperative CT scan with 3D reconstruction and a minimal period of a postoperative follow up of 2 years.
The study population consisted of 48 hips (44 patients, 4 bilateral cases) including 31 females and 13 males. The average age at the time of the operation was 2 years and 7 months, with a range of one year and 9 months to 4 years and 6 months. The average follow up period was 41 months with a range of 29 to 63 months.
The clinical findings were documented for each patient as obtained from the preoperative assessment and the follow up records. These included the presence of pain and any functional limitations, the range of motion, any leg length discrepancy and gait characteristics. Plain radiographs were used to determine the pre and postoperative acetabular roof index, the Shenton line, the center-edge angle (CEA) and the change in the appearance of the obturator foramen. The latter index is thought to indirectly reflect hinging at the symphysis pubis and is assessed by looking at the change in the ratio of the width to the height of the obturator foramen between the pre and the postoperative radiographs.
Postoperative CT with 3D reconstruction was checked for all cases. The extent of the osteotomy in relation to the triradiate cartilage was assessed to help define the bone cut as a Dega osteotomy as planned or as another variant. The anatomic characteristics of the osteotomy where also studied such as the starting point, the inclination of the cut and the thickness of the acetabular component and the relation of all these to the amount of coverage achieved. Similarly, the relation of the osteotomy to the adjacent landmarks including the arcuate line and the ilioischial limb of the triradiate cartilage and effect of this relation on the final correction obtained were also evaluated.
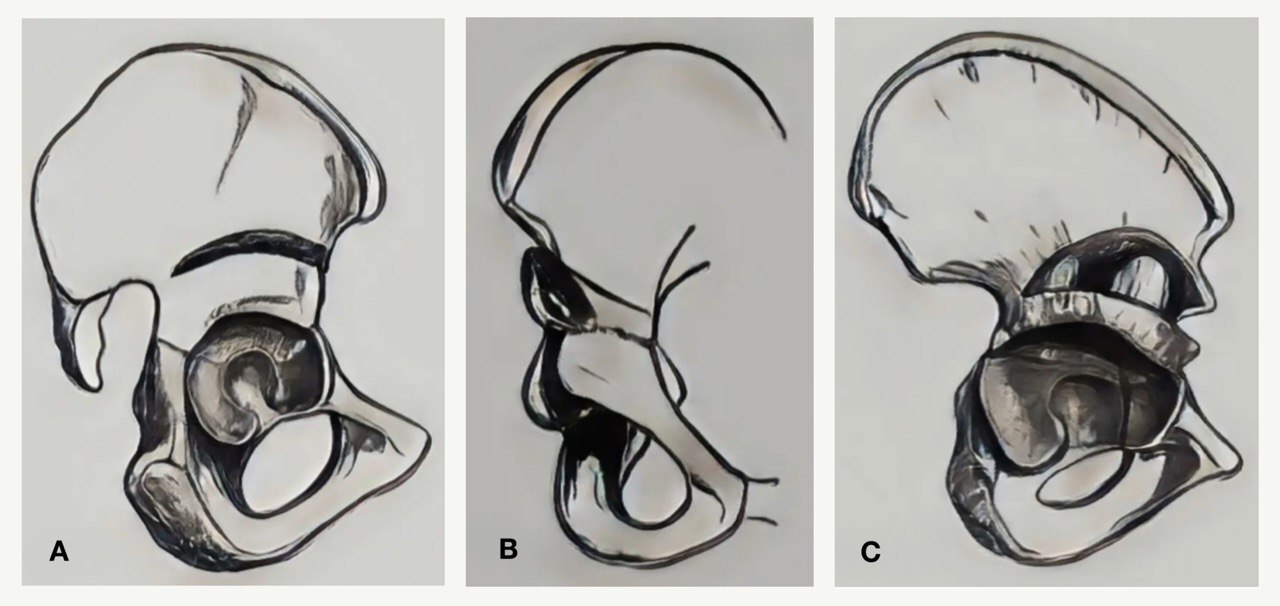
Surgical Technique, Dega osteotomy: The bony cut is marked on the outer cortex. The starting point is just above the anterior inferior iliac spine. The bony cut runs posteriorly in a curvilinear fashion to end at a point approximately 1 to 1.5cm from the greater sciatic notch (figure 1, A). The highest point of the osteotomy corresponds to the midpoint of the roof of the acetabulum. Next, a guide wire is introduced under fluoroscopic control from the highest point of the cut in the outer cortex and is directed obliquely medially to ensure that the cut in the inner cortex exits above the ilioischial and iliopubic limbs of the triradiate cartilage. The osteotome is directed in an oblique way medially and inferiorly parallel to the guide wire. The inner cortex is cut in its anterior and middle portions leaving the posterior one third to one quarter intact to act as a hinge to open the osteotomy (figure 1, B). With more experience, it is possible to avoid the fluoroscopic assistance in guiding the bony cut.
To lever open the osteotomy, an osteotome or a laminar spreader is used. It is important to notice that while doing this maneuver, the outer cortical cut may propagate into the greater sciatic notch creating a greenstick fracture. The latter rarely compromises the stability of the osteotomy since the posterior portion of the inner cortex is maintained intact.
The osteotomy site is kept open using one or two chunks of a bicortical bone graft that is harvested from the iliac crest or from the femoral shortening osteotomy (figure 1, C). Since the acetabular deficiency is predominantly anterior, the larger part of the bone graft needs to be placed anteriorly while the smaller portion is wedged posteriorly in front of the sciatic notch.
Results
The study population consisted of 48 hips (44 patients). Dega osteotomy without an additional procedure was needed for 5 hips. These included 3 hips with dysplasia without subluxation or dislocation and 2 more hips with a previous successful open reduction but with a residual dysplasia. We also had 19 hips with subluxation and 24 hips with dislocation; out of the total number of these, 27 needed open reduction and Dega osteotomy only while 16 needed an additional femoral osteotomy. Combined operations were performed on the same session in 43 hips (primary Dega osteotomy) while Dega osteotomy was performed some time-period after an open reduction was effected in 2 hips (secondary Dega osteotomy). Seventeen hips had a prior attempt of closed reduction and 4 had undergone a various combination of open reduction and femoral and/or pelvic osteotomy.
The male to female ratio was 13: 31. The average age at the time of the operation was 2 years and 7 months, with a range of 1 year and 8 months to 4 years and 7 months. The average follow up period was 41 months with a range of 29 to 63 months.
Postoperatively, clinical evaluation was undertaken on the follow up visits and was correlated with the radiologic evaluation. The clinical and radiographic assessments were undertaken at immediate postoperative encounter, at cast removal, every 3 months for the first year and then every 6 months. Modified McKay’s criteria were used in the final clinical evaluation. Using these criteria, the results were defined as:
Excellent: painless, stable, full range of motion and normal gait.
Good: painless, stable, mild restriction of motion and normal gait.
Fair: painless, stable, moderate restriction of motion and positive Trendelenburg’s sign.
Poor: painful, unstable and required further surgical interference.
Table 1 shows the distribution of the final outcomes.
The radiographic evaluation included several indices. The acetabular roof index improved in all hips except in one case were we had immediate postoperative displacement due to dislodgement of the graft. The center-edge angle (CEA) improved in 40 out of 43 hips with subluxation/ dislocation included in the study. It failed to improve initially in 3 hips which included 2 cases of postoperative re-dislocation and one case of valgus overgrowth which necessitated secondary procedures. The improvement in the value of the CEA was observed immediately postoperatively and continued to improve on the follow-up visits. Table 2 shows the changes in the values of these radiographic signs and the p-value.
The change in the appearance of the obturator foramen was evaluated. Such a change is thought to reflect the re-orientation of the acetabular component due to motion at the symphysis pubis. The ratio of the width to the height of the foramen was assessed and its preoperative and postoperative radiographs were compared. It was found to be significantly changed in 11 patients (22.9%). Most of the patients (9 out of 11) in whom such a change was encountered were older than 3.5 years.
We used CT with 3D reconstruction to evaluate all the cases postoperatively. It was performed within one week postoperatively. Out of the 48 Dega osteotomies which were assumed to be undertaken, we found that 6 (12.5%) were actually Pemberton’s and 4 (8.3%) were actually Pembersal’s). Despite this discrepancy between the planned procedure and the end result in these cases, we found no significant difference in the amount of correction effected between the 3 variants (p-value 0.0055).
We also used the CT evaluation to assess the amount of correction induced by the osteotomy and its relation to the arcuate line. We found that the arcuate line was crossed in 44 hips (91.6%). The site of crossing varied. Despite that this site is difficult to describe in exact anatomic terms, we could divide the cases into two groups depending on whether the crossing point of the arcuate line occurred above or at/ below the level of the midpoint of the greater sciatic notch. The midpoint of the notch was labelled on the 3D CT scan in reference to the SI joint, the roof of the notch and the iliopubic limb of the triradiate cartilage. We found that “low crossing” occurred in 33 hips (75%). However, we found no significant difference in the average amount of correction induced between the 2 groups (p-value 0.0053). Figure 2 shows an example of the CT scan 3D reconstruction to evaluate the mentioned parameters.
The relation of the Dega osteotomy to the ilioischial limb of the triradiate cartilage was also evaluated on the CT scan. By definition, the Dega osteotomy does not cross the triradiate cartilage. We found that the osteotomy cut could pass at a variable distance from the ilioischial limb depending on variable factors including the starting point and the inclination of the cut. We found that the amount of correction of the acetabular dysplasia was in an inverse relation to the distance from the ilioischial limb of the triradiate cartilage as the closer the cut to this structure, the more the correction imparted as reflected on the indices of the acetabulum. We admit that it was difficult to put this relation in quantitative terms.
The starting point of the osteotomy was also evaluated. We compared the amount of correction in cases where the starting point was one cm or less from the anterior inferior iliac spine (13 clearly defined such cases) to those where it was 1.5cm or more (19 clearly defined such cases). We neglected the cases where the measure of the distance was not clearly defined (16 cases). We found that there was a slight difference (p-value 0.00479) in favor of a high starting point in offering lateral coverage of the head. Moreover, we found that the closer the osteotomy cut to the acetabulum, the thinner the acetabular fragment and the better the re-shaping of the acetabulum. However, this variable is again difficult to quantify. Figure 3 (A and B) demonstrates one of the cases treated by open reduction, Dega osteotomy and femoral osteotomy.
Complications: Out of the 48 hips, we had 6 cases (12.5%) that needed secondary procedures . We had one hip with dislodgement of the graft immediately postoperatively with inadequate displacement of the osteotomy. It occurred in a female who was 4 years and 2 months old who also underwent open reduction and femoral osteotomy at the same session. She needed revision of the Dega osteotomy using the same graft material fortified by an iliac crest graft along with revision of open reduction. Postoperative re-dislocation occurred in 2 cases (one immediately postoperatively, one on early follow up) both were treated by revision of open reduction and Dega osteotomy. We had one case of a valgus overgrowth that was diagnosed 3 years after the index procedure with recurrence of the hip dysplasia and it was addressed by a varus femoral osteotomy. We also had one case of excessive varus proximal femur that was observed 1.5 year postoperatively and was treated by a valgus osteotomy. Lastly, we had one case of excessive external rotation following femoral osteotomy that was seen 1 year after the index procedure and was treated by an internal rotational osteotomy. Table 3 summarizes the complications encountered during this study.
Discussion
Over the last a few decades, Dega osteotomy has been widely used for the treatment of DDH. Several advantages are thought to make it as an appealing option. Since the sciatic notch is maintained intact, the osteotomy is noticeably stable with no added means of fixation.20 Also, for the same reason, this osteotomy does not cause an iatrogenic lengthening of the limb. The osteotomy does not violate the triadiate cartilage in comparison to other osteotomies like those attributed to Pemberton,16 Trevor et al21 and Perlik et al.17 This would minimize the theoretical risk of damage to the triradiate cartilage. Moreover, the Dega osteotomy is thought to both re-shape and re-orient the acetabular fragment.22–25 However, there is no consensus on what represents a Dega osteotomy from the technical point of view.22,24–26 This is attributed in part to the reports of Dega himself and his coworkers. Dega wrote 2 accounts on incomplete semicircular transiliac osteotomy in 1969 and 1974. In these, he described 2 slightly different osteotomy designs. A need has arisen to put this procedure in a standard form in terms of the starting point, the extent and the orientation. In this account, we tried to emphasize these details as described above. We found that a starting point that is 1.5cm or more from the anterior superior iliac spine would ensure a better coverage. However, the statistical difference in the amount of coverage from those cases with a relatively low starting point (one cm or less from the anterior inferior iliac spine) was not that large (p-value 0.00479). On the other hand, a thinner roof acetabular fragment offers a better re-shaping. This is attributable to two factors, namely, a better pliability and a closer cut to the triradiate cartilage and the lower part of the sciatic notch. It should be noticed though that, a lower starting point carries a risk of penetrating into the joint cavity.
We found that it is crucial to spare the cortex of the sciatic notch and the adjacent medial 1 to 1.5cm extent of the inner iliac cortex. This would offer an adequate hinging of the acetabular fragment in the direction that compensates for the acetabular dysplasia. Since the acetabular deficiency in DDH is mainly lateral and anterior, it is possible to spatially manipulate the acetabular fragment by changing the amount of the cut in the inner cortex. As more of the medial extent of this cortex is cut, more posterior hinging is offered and hence more anterior coverage. On the other hand, if more medial cortex is spared, a posteromedial hinging and a more lateral coverage is provided.
We think that Dega osteotomy can both re-shape and re-orient the acetabulum. Re-orientation can be easily checked on the anteroposterior radiograph of the pelvis as it is reflected by the change in the appearance of the obturator foramen (width to height ratio), the acetabular roof index and the center-edge angle. The re-shaping of the acetabulum, on the other hand, is difficult to put in quantifying terms as stated above.
The change in the appearance of the obturator foramen, as was evident by the change in its width to height ratio, was found in 22.9% of patients and that was mostly observed in patients whose age being older than 3.5 years. This can be explained on the base of the hinging mechanism in Dega osteotomy. Most of the hinging is believed to occur at the triradiate cartilage and the sciatic notch. However some of the hinging occurs at the symphysis pubis and this occurs more in older children. Since the change in the appearance of the obturator foramen reflects hinging at the symphysis pubis, it is more evident the older the child. These facts give support for using the Dega osteotomy for both before and after fusion of the triradiate cartilage.
The postoperative CT scan with 3D reconstruction was reviewed in all cases. It demonstrated that, 20.5% of the osteotomies crossed the ilioischial limb of the triradiate cartilage turning what was planned as a Dega osteotomy into a Pemberton or a Pembersal osteotomy. This is mostly attributed to the limited intraoperative exposure. It is interesting that the amount of correction imparted in such cases did not differ significantly from those cases treated by a Dega osteotomy.
The CT scan also demonstrated the relation of the osteotomy to the arcuate line which represents the iliac part of the iliopectineal line and marks the pelvic brim. It was found to be crossed in most cases (91.6%). The CT revealed that this structure could have been crossed at its upper or lower extent. However, The level of such crossing was not a significant determinant of the amount of the correction achieved by the osteotomy. On the other hand, the relation of the osteotomy to the ilioischial limb of the triradiate cartilage significantly affected the amount of correction. The closer the osteotomy to this structure, the more the displacement of the osteotomy and hence the more the correction. This can be explained by hinging of the osteotomy at a more flexible region when the osteotomy is closer to the cartilage.
In this study, we report our experience with Dega osteotomy with excellent to good clinical outcome being obtained in 83.3% using the modified McKay’s criteria. >Concentric reduction was achieved and maintained in 45 hips (93.7%) with only 3 cases needed to repeat the Dega osteotomy. Out of these, one case had failure that was directly attributable to the Dega osteotomy due to dislodgement of the graft and inadequate displacement of the osteotomy while the other 2 cases had re-dislocation. All 3 cases where treated successfully by re-open reduction and revision of the Dega osteotomy. These results are comparable to those obtained from several other studies including those of Reichel and Hein,27 Al-Ghamdi et al.,25 El-Sayed et al.,28 Grudziak and Ward,22 and Karlen et al.24 The 2 last studies delt with Dega osteotomy performed for DDH and neuromuscular disorders.
Our overall reoperation rate was 12.5%. This was attributable to multiple causes as emphasized in table 5. One hip (2.08%) only had its failure was directly related of the Dega osteotomy itself. Our reoperation rate was higher than observed in some studies as in the reports by Labaziewicz29 who reported 4.1% reoperation rate, Pucher30 and Senger31 who reported 2.9% reoperation rate. On the other hand, a higher reoperation rate were reported by Grudziak et al.22 which was 16.6 (24 hips) and El-Sayed et al.23 which was 18.9% (58 hips). Such a variation of the reoperation rates between different studies can be explained based on several reasons. These include the different DDH populations involved in the study, the variable lengths of the follow-up period, the threshold set for a revision procedure and the experience of the surgeons who performed the index procedure. Pucher et al.,30 reported 2 serious complications namely, extension of the osteotomy to the hip and septic arthritis but no re-dislocation.
Conclusion
Our study demonstrates the significance of performing the Dega osteotomy in a technically accurate manner as an integral part of the surgical treatment of DDH. A special focus was directed toward the stability and the preservation of the elastic recoil of the sciatic notch as well as the spatial orientation of the bone cut. We believe that the results of the Dega osteotomy in the treatment of the DDH children are satisfactory and reliably reproducible with a concentric reduction rate of 93.7% and a re-operation rate of 12.5%. Referring to postoperative CT scan, we found that in some cases (20.7%) the osteotomy turned to be performed as Pemberton or a Pembersal. However, this did not compromise to the final result. The limitations of this study included certain aspects. A longer follow-up period, preferably to skeletal maturity, would have been more effective in evaluating the outcome. Another limitation was the age of the patients which were relatively young. We are interested in investigating the effect of the Dega osteotomy in DDH in older children and specially for revision cases. Finally, some of the variables in the study were difficult to put in clear measurable terms including the distance of the osteotomy from the anterior inferior iliac spine and the amount of the re-shaping of the acetabulum induced by the osteotomy.
Acknowlegement
Acknowledgement to the Iraqi Ministry of Higher Education and Scientific Research for funding this study and to Dundee University, UK for collaboration.
Conflict of interest
We declare no conflict of interest.
Ethical standards
Approval of the Ethical Committees of the Al Hussein Teaching Hospital, College of Medicine, University of Thi Qar was obtained before any data were collected. Written consent was obtained from all patients and/ or their parents/guardians.
Funding
The research is funded by the Iraqi Ministry of Higher Education and Scientific Research.