1. Introduction
Proximal femoral fractures (PFF) pose a formidable health challenge, representing one of the most common types of fracture in the elderly population1: they have gained increasing attention due to their association with age-related bone fragility and the growing aging population. As explored by Dhanwal et al. the epidemiology of hip fractures reflects a global diversity: genetic and environmental factors play a role in the etiology of hip fracture.2 Understanding the etiology and finding predictable factors of different types of hip fracture (femoral neck and trochanteric) can help with prevention and management.3
There have been ongoing discussions concerning optimal treatment of lateral proximal femoral fractures (LPFF): which one leads to the least amount of failures, quickest rehabilitation and, most importantly, lowest mortality. Intramedullary nailing is considered the most appropriate treatment option in LPFF.4 Literature considers different parameters in order to define which factors most influence the outcome of the surgery: on top of patient age and correct reduction of the fracture, but also failure of fixation due to cephalic screw cut-out is one of the most relevant factors.5 The correct positioning of the cephalic screw depends on 2 factors: the region of the femoral head where it is positioned in the antero-posterior (AP) and lateral view and the distance between the apex of the lag and the cortical of the femoral head. This latter parameter has been evaluated by Baumgartner et al, which defines it as the “tip apex distance” (TAD index) that represents the result of the sum of the distances between the apex of the nail and the external cortical in the AP and lateral view.6
TAD is the strongest predictor of a cut-out after intramedullary nailing in PLFF and the critical threshold is 25 mm.7 So, the ADAPT (ADAptive Positioning System) Stryker system (Stryker Leibinger GmbH & Co. KG, Freiburg, Germany) has been developed; it can intra-operatively calculate the TAD as well as the tip-surface distance, which is the 3D distance between the lag screw’s tip and subchondral bone surface of the femoral head.
The ADAPT system is composed of a set of points of reference that are applied to the brilliance amplification device and to the external maniple of the Gamma nail (Stryker); this signal is then sent to an external device which uses an ad hoc software in order to determine the TAD index and the distance between the apex of the cephalic screw in the two view. It then suggests necessary adjustments to obtain a positioning within the optimal range.
The aim of this study was to compare the results obtained with the use of the ADAPT system with the results achieved in the patients where this system wasn’t used.
2. Materials and Methods
Our first approach to the surgical navigation platform goes back to the end of 2020 but we consider the period between January '22 and December '22 to mitigate bias related to the inability of the surgical team to fully use this system. A total of 97 patients with diagnosis of intertrochanteric fractures in 2022 were evaluated. A retrospective analysis was performed. We divided patients in two groups according to the osteosynthesis procedure: with (group I) or without (group II, control group) the Stryker ADAPT®system. Among the sample analysed, 34 patients were categorised under group I, 63 patients under group II. Orthopaedic Trauma Association (AO/OTA) fracture classification was used to evaluate fracture type: the fractures were grouped into classes 31A1, 31A2 and 31A38 We included basicervical fractures (31B3) treated with cephalomedullary nail. The treatment of basicervical femoral neck fractures remains a topic of interest and controversy. It is widely agreed that intramedullary fixation is more effective in preventing complications such as fixation failure.9 However, only few studies have focused on the outcomes of intramedullary nailing in treating basicervical fractures.10,11
Two authors (G.G.M and S.C) independently collected data. Any discordance was resolved through consensus with a third author (L.C.). The study was conducted in a level -1 trauma centre and the surgery was performed by expert trauma surgeons (M.N., M.D.G., E.L.). All cases were operated on a fracture surgery traction table. In all patients the Gamma 3 (Stryker®) nail (170 length, 125° neck angle) was implanted, locked with a distal static screw. All the patients had antibiotic prophylaxis12; an urinary catheter was preoperatively placed; postoperatively, anti-thrombotic stockings and low molecular weight heparin prophylaxis were used in order to avoid deep vein thrombosis; we collected pre and post-operative radiographies (AP pelvic view, AP and LL view of the affected hip) of all the patients.
We examined the operative time, the cephalic screw angle, the post operative cases of nail cut out and the use of the U-blade (Stryker®). It’s a device occasionally applied to strengthen the lag screw and to avoid rotation of the femoral head over the femoral neck. As a main control criteria, we evaluated the tip apex distance (TAD) obtained. This value was calculated using the Baumgaertner’s equation. When ADAPT was used, the system itself verified the TAD value.
We followed the patients for at least 1 year of follow-up. We performed postoperative x-rays, an x-rays at 1 month, 3 months, 6 months and a x-rays at 1 year after surgery.
Statistics were conducted using chi-square test to compare data between the two groups and t-student test for the continuous data. Data was processed by SPSS IBM software. Values of P < 0.05 were considered to be statistically significant.
3. Results
3.1. Demographic characteristics
We evaluated 97 patients, 18 (18.5%) were male and 79 (81.5%) were female. The mean age at diagnosis was 82.9 (standard deviation, σ 8.9) years. Concerning the type of fracture, 39 (40,2%) were classified as 31A1, 29 (29.9%) as 31A2, 12 (12.4%) as 31A3 and 17 (17.5%) were grouped into class 31B3. There were no significant differences in terms of type of fracture between two groups (p=0.389). Demographic and clinical data are presented in Table 1.
3.2. Treatment
Among the enrolled patients, 34 (35.1%) were treated with ADAPT System, 63 (64.9%) without it (control group). The mean age was 83.71 years (σ 8.062) in the ADAPT group and 82 years in the control group (σ 9.401), p=0.373.
The operative time was 48.88 min (σ 18.110) in the ADAPT group and 46.35 (σ 15.650) min in the control group (p=0.09)
The mean cephalic screw angle in the ADAPT group was 125.15° (σ 1.941), compared with 125.24° (σ 1.663) in the reference group treated without the ADAPT device, p=0.809.
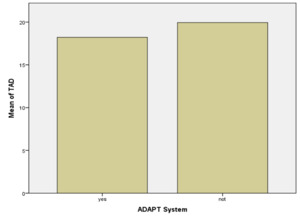
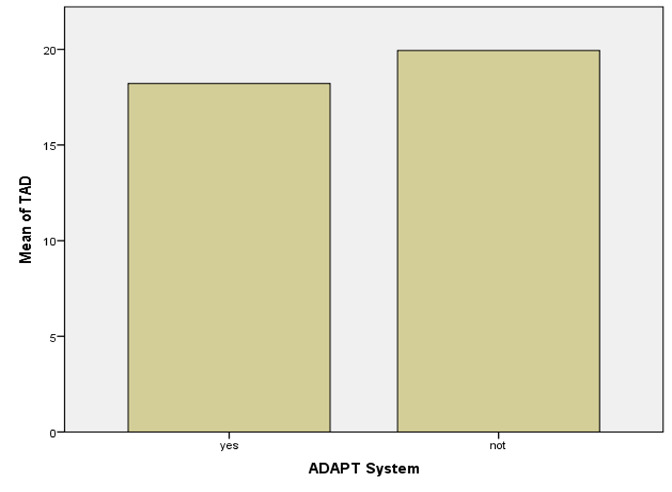
Regarding the TAD, it seems expected to be lower with the ADAPT system. TAD was 18.21mm (σ 5.407) in the ADAPT group and 19.94mm (σ 5.570) in the control group (p=0.149) as resumed in Table 2.
Thus, the ADAPT group didn’t benefit from a statistically significant reduction of the TAD compared to the control group: T-student test proved it (Figure 1).
In a second phase of our analysis, we reported that 5 patients (5.15%) suffered from cut-out of lag screw, only one of them treated with ADAPT system (p=0.47).
16 patients (16.49%) underwent internal fixation using the U-Blade lag screw: we observed cut out in only one of them (6.25%). There were no significant differences with a p-value = 0.32 (Table 3).
The mean TAD was 18.9mm in the group of 92 patients (94.85%) without any mobilisation of lag screw (standard deviation, σ 5.190) and 27.40mm (standard deviation, σ 6.269) in the group of 5 patients who suffered from cut-out of lag screw. As shown in Table 4, a statistically significant difference was found between these groups (p=0.037).
4. Discussion
In recent years computer-assisted orthopaedics surgery has increased. The better efficiency and accuracy in device positioning leads to less failures of the implants and consequently second revision surgeries.13
Computer-assisted surgery has also been employed in femur traumatology as well. Our study aimed to show the impact of the ADAPT system in the surgical treatment of proximal femoral fractures. ADAPT system aims to help the surgeon to reduce the risk of misplacement of the lag screw.
The safety margin established by Baumgaertner et al.6 is correlated to the biomechanics of the hip and the transmission of forces from the load-bearing zone along the force lines of Ward, avoiding overloading of peripheral cephalic regions. Right at the base of the femoral neck, where Ward’s triangle is situated, there are particularly intense forces of flexing strain, the degree of which is related to the length of the neck.14
Pervez H et al reported that the ideal measurement is 5mm < TAD < 20mm,15 Herman A et al and Hsueh KK et al reported that inferior-centre placement of lag screw is best although TAD is greater than 25mm.16,17 As Takai et al noticed in their study, TAD in the case of inferior-centre positioning is larger than that centre-centre positioning because the distance from the tip of the lag screw to the axis of the femoral neck is obviously longer in inferior-centre positioning.18 Baumgaertner MR et al and Galanakis IA et al claim that the centre-centre position of the lag screw is better.7,19
The critical nature of TAD underscores the broader importance of precision in cephalomedullary nailing. Our data correlates with the literature, indicating that the placement of the lag screw must be as accurate as possible within the quadrants defined by Park et al.,20 and its length carefully selected to prevent varus displacement of the femoral neck and migration of the screw itself.
In the literature It’s still controversial if a higher TAD is a major risk of lag screw cut-out.
Andruszkow H et al and Geller JA et al support that increased TAD is one of the strongest predictors of failure of the osteosynthesis due to cut-out.21,22
Our analysis reveals a strong correlation between the TAD and the incidence of cut-out. We found 5 patients who suffered from lag screw cut out (5.15%) with a mean TAD of 27.40mm; on the other side we reported a mean TAD of 18.9mm in the group of 92 patients (94.85%) without any mobilisation of lag screw.
As Kang et al reported in their study, mechanical instability of the lag screw could contribute to screw migration and consequent fixation failure.23 The U-blade gamma nail has a screw-blade hybrid type device. Kwak et al. reported that the rotational stability of the proximal fragment was greater with the hip screw type than with the blade type and hybrid type in a biomechanical study.24 We reported that 16 patients (16.49%) underwent internal fixation using the U-Blade lag screw: we observed cut out in only one of them (6.25%) although there were no significant differences.
In our series, the majority of patients were treated with nails with a cervicodiaphyseal angle of 125°, achieving often an optimal TAD. The mean cephalic screw angle in the ADAPT group was 125.15°, compared with 125.24° in the reference group treated without the ADAPT device.
The ADAPT system doesn’t demonstrate a concrete advantage in our study regarding TAD and lag screw cut-out. TAD was 18.21mm (σ 5.407) in the ADAPT group and 19.94mm (σ 5.570) in the control group. Even if only one patient treated with ADAPT system suffered from lag-screw cut out, it’s not statistically significant (p=0.47)
In our study, in terms of intraoperative time, ADAPT System doesn’t modify surgical time. Atesok K et al sustain that the disadvantages of computer-assisted trauma include a time-consuming to set up and an increased operating time.13 In our analysis the operative time was 48.88 (σ 18.110) min in the ADAPT group and 46.35 (σ 15.650) min in the control group (p=0.09).
The limitations of our study are represented by its retrospective nature and bias in patients recruitment. Unfortunately we also have lack of data on patients’ bone quality. Moreover, our study doesn’t consider radiation dose time. The literature argues that the ADAPT system reduces radiation exposure.25,26
5. Conclusion
While the ADAPT system didn’t exhibit advantages in our comparative analysis, the highlighted correlation underscores the fundamental importance of achieving optimal TAD in cephalomedullary nailing that the ADAPT System ensures. As orthopaedic surgery continues to evolve, these insights pave the way for refined techniques and further exploration of computer-assisted systems to enhance precision and improve patient outcomes.
Our study reveals a strong correlation between the Tip Apex Distance (TAD) and the incidence of cut-out if LPFF.
It must be shown in further studies if it will lead to a decrease in postoperative complications and reduction of cut-out rate, but our results are promising and indicative of potentially improved surgical outcomes.
Conflicts of interest
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.