Introduction
Genu valgum, colloquially known as “knocked knees,” is a coronal plane deformity of the lower extremity characterized by a medial displacement of the Q angle exceeding 20 degrees. While bilateral genu valgum may be physiologic in pediatric populations, unilateral and bilateral presentations can result from underlying pathology.1 These may range from metabolic conditions such as Rickets, to local disorders such as infection, tumor growth, or trauma.2 Depending on the cause and severity of presentation, genu valgum may be treated conservatively through the use of exercise programs, NSAIDs, orthotic insertions, or surgically through osteotomy or guided growth surgery.3
A physeal bar results from injury or infection to the growth plate (physis) before fusion, leading to a bony interruption that disrupts normal bone growth. In the case of the distal lateral femur, a physeal bar can cause interruption of lateral femoral condyle growth, potentially resulting in a valgus deformity.1,4 Multiple studies evaluating the operative management of physeal bars and concomitant genu valgum emphasize that physeal bar resection and hemiepiphysiodesis can correct both deformities while preserving remaining growth potential.1,2,4,5
Case Presentation
A 13-year-old-male presented to urgent care with a six-day history of left leg pain. He reported that the pain occurred daily and was exacerbated with ambulation and weight-bearing activities. He had an episode of this pain one month prior which lasted for one week and resolved without intervention. X-Rays of the tibia and fibula taken during that visit showed no soft tissue abnormalities, fractures, or dislocation. Given his atraumatic appearance and medical history, he was counseled to continue conservative treatment with over-the-counter pain medication, activity modification, and heating pads.
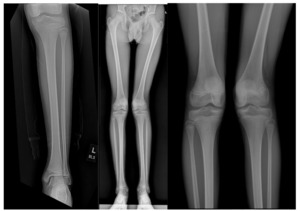
As the pain persisted, a follow-up appointment with orthopedic surgery was scheduled. By this time, the pain had been continuous for seven weeks. A review of imaging as well as further radiographs of the lower extremity revealed a left genu valgum, a minor limb length discrepancy, and a potential distal lateral femur physis bar [Figures 1a, 1b, 1c].
The patient’s mother reported that he had a left knee infection at 1.5 years old which was managed operatively. She was however unsure if this infection was septic arthritis or osteomyelitis. As his genu valgum may have been related to bony changes following the infection, further imaging was ordered. A left knee CT scan and MRI showed a distal lateral femur physis bar measuring 1.1 x 0.8 cm in the transverse and antero-posterior dimensions respectively.
Management and Outcomes
Given his history of operatively-managed infection and findings on imaging, he underwent operative management with a left medial distal femur hemiepiphysiodesis and lateral distal femur bar excision. An intraoperative O-arm was utilized to ensure proper reaming of the physis bar. [Figures 2a, 2b, and 2c].
The patient returned for a follow-up two weeks after his procedure for repeat radiographs showing the medial distal femur hemiepiphysiodesis plate in good position, as well as the remaining area of the lateral distal femur physis [Figures 3a and 3b]. He was advised to begin at-home exercises to increase strength in his left quadriceps. However, at six weeks post-surgery he experienced difficulty ambulating without his crutches. Consequently, he was instructed to begin physical therapy and to gradually resume weight-bearing activities as tolerated.
Three months after the procedure, the patient was ambulating without the use of crutches, experiencing no difficulty or knee instability. Given his progress, he was able to resume all athletic activities except physical contact sports. Repeat standing radiographs showed improvements in genu valgum. Six months post-surgery he returned for a follow-up and reported no further aggravation of his left knee, with full ability to ambulate unassisted.
Nine months after surgery, the patient experienced left knee medial patella pain for two weeks and pain with ambulation, without any inciting trauma. He did not exhibit a limp in his left lower extremity and his genu valgum was improving without any swelling. On examination, there was mild tenderness to palpation of the medial retinaculum but no gross instability of the patellofemoral joint. A standing Scanogram was done to evaluate postoperative changes as well as to assess correction of genu valgum. The new onset medial patellofemoral pain was likely related to inadequate quadriceps strength which was evaluated during the exam, as may be explained with changes in force vectors on the patella following operative correction. He was instructed to continue physical therapy to improve quadriceps strengthening.
Conclusion
This case highlights the careful management of a physis bar with concurrent genu valgum. Recent literature focused on post-infectious physeal bar development found that distal femur bar formation manifested an average of 23 months post sepsis. Bar development can result in Q-angle deformities and limb length discrepancies, both of which were seen in our patient.6 While his remote history of knee infection happened in early childhood, the operative management of his pathology may have contributed to knee joint trauma which manifested following long bone growth. Regardless of the etiology of his physis bar and following genu valgum, operative management was indicated through the use of bar resection and hemiepiphysiodesis.
One possible complication of hemiepiphysiodesis is the reformation of the pathology due to long-term damage to the physis. These complications are more commonly seen in patients who undergo operative correction after the age of 10 years, potentially due to partial closure of the physis.7
Our patient presented with medial knee pain nine months after surgery, which can be attributed to minimal participation in physical therapy, leading to weakness in his left quadriceps muscle. This weakness may originate from both pre-operative weakness and post-operative muscle wasting due to a lack of physical therapy. As he is now 14 years old, strength training and therapy are imperative to attenuate strength loss and prevent further complications, such as changes in static and active balance, coordination problems, and falls. Although correction of genu valgum to an improved mechanical alignment may lead to rebound growth correction of the cartilage, the implantation of corrective plates in this region may improve pain levels as strength develops in his quadriceps.8–10
This case highlights the management of a pediatric patient presenting with complex knee pathology following a history of early childhood knee infection. Surgical intervention involving medial distal femur hemiepiphysiodesis and lateral distal femur bar excision effectively addressed the anatomical abnormalities identified on imaging, leading to significant improvement in ambulatory function and pain resolution. The occurrence of medial patellofemoral pain underscored the importance of tailored rehabilitation programs focusing on quadriceps strength. Through comprehensive assessment and multidisciplinary management, including surgical intervention and structured rehabilitation, favorable outcomes were achieved, emphasizing the significance of individualized care in pediatric orthopedics.
Author Contributions
M.Z. and E.S. conceived of the presented idea. M.Z. and S.N. developed the theory and performed the computations. M.Z., P.Z. and S.N. verified the analytical methods and analyzed the presented results of the data. E.S. encouraged M.Z., P.Z., and S.N. to investigate the outcomes and long-term impacts and differences of both variables in addition to supervising the findings of this work. All authors discussed the results and contributed to the final manuscript.
Author Disclosures
In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: N/A declare(s) Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Ethical considerations
Verbal consent to publish and provide educational materials on the current case was obtained from the guardian’s of the patient.