Introduction
Knee osteoarthritis (OA) stands as a formidable global health challenge, characterized by the relentless degeneration of articular cartilage within the knee joint. This progressive condition, marked by synovial inflammation and subsequent functional limitations, reigns as the most prevalent form of arthritis.1 The associated pain, stiffness, and a relentless loss of motion significantly compromise patients’ quality of life, limiting their ability to perform even the most basic activities of daily living (ADLs). From the inability to climb stairs with ease to the struggle with participating in work or social activities, knee OA casts a long shadow of limitations.2
Total knee arthroplasty (TKA) is a highly successful surgical intervention for end-stage knee OA. By effectively alleviating pain and restoring joint function, TKA has transformed lives. Over the past few decades, it has become one of the most frequently performed procedures in orthopedic surgery, with over one million procedures bolstering mobility annually in the United States alone.3 Despite the remarkable advancements in TKA techniques and implant designs, a significant portion of patients continue to experience a lingering sense of incompleteness following surgery. Studies report that up to 20% of patients may express dissatisfaction after TKA, citing issues that cast a shadow on their perceived success. Residual pain, persistent stiffness, abnormal gait mechanics that disrupt natural movement patterns and a disquieting sense of joint instability can mar the experience.4 These limitations are often attributed to the inherent challenges of replicating the native knee’s intricate kinematics and the delicate balance of the soft tissues during conventional TKA procedures.
Traditionally, TKA has focused on achieving a standardized mechanical alignment based on idealized anatomical landmarks. This approach, while seemingly straightforward, may not fully account for the intricate variations in individual anatomy and the pre-existing kinematic patterns of the diseased knee joint. This mismatch between the implant and the patient’s unique biomechanics can lead to abnormal stress distribution across the prosthetic components. This, in turn, has the potential to accelerate implant wear and tear, potentially compromising long-term functionality and ultimately, patient satisfaction.5 Thus in recent years, a wave of innovation has swept through the field of TKA, driven by the pursuit of addressing these limitations and optimizing long-term outcomes. Two key advancements have emerged at the forefront of this exciting journey: kinematic alignment (KA) and personalized knee arthroplasty.6
Kinematic Alignment: Kinematic alignment (KA) represents a paradigm shift in surgical philosophy, a move away from a one-size-fits-all approach. Instead, it focuses on meticulously recreating the patient’s individual pre-arthritic joint kinematics. This innovative approach utilizes sophisticated intraoperative navigation techniques.7 These techniques act as a conductor’s baton, guiding the surgeon with high-fidelity data to precisely replicate the patient’s natural joint line orientation and the tension of the ligamentous structures during implant positioning. Proponents of KA argue that this strategy fosters a more natural feeling knee joint. This, in turn, has the potential to lead to improved implant longevity, a more natural gait pattern that closely resembles pre-arthritic movement, and ultimately, a higher level of patient satisfaction.8
Personalized Knee Arthroplasty: Personalized knee arthroplasty takes the concept of patient-specific optimization a step further, venturing into the realm of bespoke solutions. This approach leverages advanced imaging techniques such as CT scans and magnetic resonance imaging (MRI).9 These detailed scans, coupled with computer modeling, pave the way for the creation of customized implant components. These components are meticulously designed to precisely match the patient’s unique anatomical geometry, encompassing both the femoral and tibial bone surfaces. This potentially allows for a more congruent articulation between the implant and the remaining native bone. This improved fit has the potential to reduce stress concentrations and enhance implant stability, potentially leading to superior long-term outcomes.10
The growing adoption of KA and personalized TKA techniques necessitates a critical appraisal of the current evidence regarding their long-term outcomes compared to conventional TKA.11 A comprehensive systematic review and meta-analysis can serve as a powerful tool to illuminate the path forward. By systematically evaluating the existing literature, this study aims to shed light on the comparative effectiveness and safety of these emerging surgical strategies and provide a robust and objective assessment of the current evidences, which will provide valuable evidence-based guidance for orthopaedic surgeons to make informed decisions regarding the optimal surgical approach for individual patients undergoing TKA. Ultimately, the aim is to refine surgical techniques, improve patient outcomes, and enhance long-term mobility and quality of life for those suffering from knee OA.
Methods
The study was conducted according to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines and checklist.12 Following the rules of the Cochrane Handbook for Systematic Reviews of Interventions.13
Literature search
We searched PubMed, Web Science, Cochrane Library and Scopus on June 2, 2024 for published randomized controlled trials using the following search strategy: also we manually screened the reference lists of the included studies for any eligible articles.
Eligibility criteria and study selection
We included randomized controlled trials that compared Kinematic alignment with Mechanical alignment in patients undergoing total knee arthroplasty. We excluded animal studies, cohort or case control reports, in vitro studies, overlapped datasets, conference abstracts, reviews, book chapters, theses, editorial letters and abstract only papers. After duplicate removal using Endnote two authors independently performed the title and abstract screening then the full text screening. Conflicts were solved by consulting a third author.
Data extraction
We extracted baseline demographic characteristics of the patients, summary of the main results of the included studies, along with the following outcomes: combined knee society score (KSS) at 6 and 12 months, KSS Patient satisfaction at 1 year, KSS function score at 2 years, Oxford score at 6 months and 2 years, KOOS score, mMPTA, Range of motion at 1 and 2 years, length of stay, Duration of surgery, and Incision length.
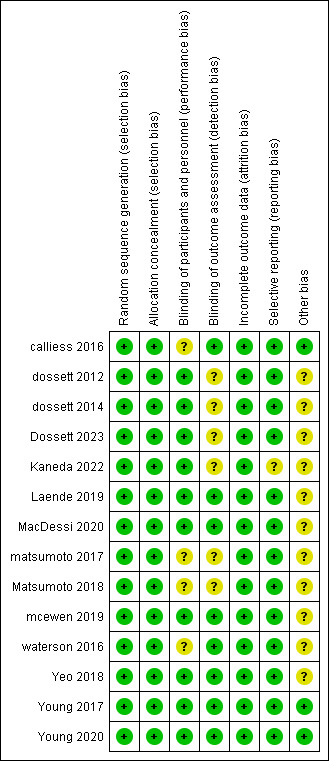
Risk of bias assessment
Two authors independently assessed the quality of the included studies using Cochrane risk of bias tool as described in Cochrane handbook.14 The main assessed bias domains include: selection bias, performance bias, detection bias, attrition bias, reporting bias, and other potential sources of bias.
Data synthesis
We used Review Manager software version 5.4 for the meta-analysis, continuous outcomes were pooled using main difference (MD), dichotomous outcomes were pooled using odds ratio (OR), all with 95% confidence intervals (CIs). Heterogeneity was assessed using chi-square and I-square tests. The studies were considered heterogeneous at chi-square p-value < 0.1 and I2 > 50%. Fixed effect model was used for the analysis unless heterogeneity was detected in which case random effect model was used.
Results
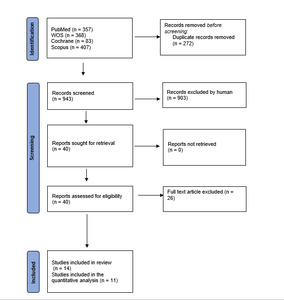
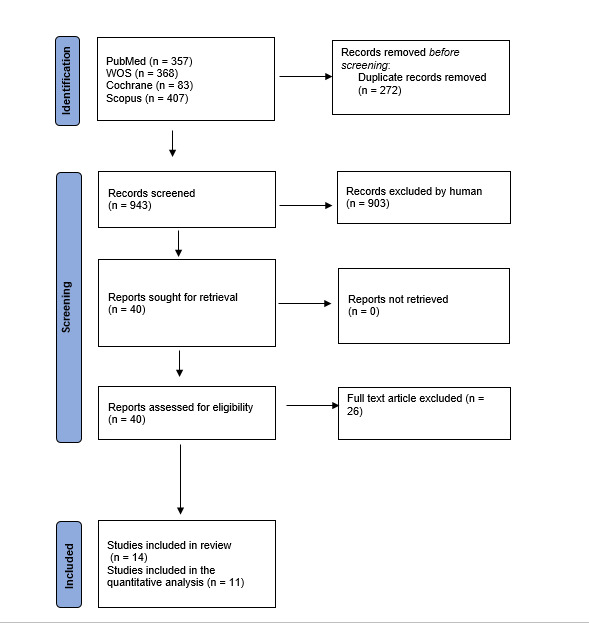
We found 1215 article through literature search. After duplicate removal, title and abstract screening and full text screening we finally included 14 articles.15–28 (See PRISMA flow diagram; Fig. 1).
Baseline characteristics of the included studies are shown in table 1. And table 2 show the summery and main results. The included studies mainly demonstrated a low risk of bias throughout the assessed domains; the details are presented in fig. 2.
Meta-analysis results
Knee society score
Combined KSS at 6 months
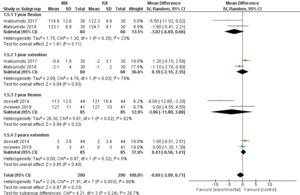
Two studies reported the outcome with153 total participants. The pooled results showed no statistically significant difference between mechanical and kinematic alignment in KSS at 6 months postoperatively (MD = -13.21, 95% CI [-34.93, 8.50], P = 0.23), however the pooled data were heterogeneous (P = 0.01, I² = 843. %). fig.3.
Combined KSS at 12 months
Two studies reported the outcome with 271 total participants. The pooled results showed no statistically significant difference between mechanical and kinematic alignment in KSS at 12 months postoperatively (MD = -4.27, 95% CI [-20.23, 11.68], P = 0.60), the pooled data were heterogeneous (P = 0.001, I² = 90%). fig.3.
KSS Patient satisfaction at 1 years
Three studies reported the outcome with 130 total participants. The results showed no statistically significant difference between mechanical and kinematic alignment in KSS Patient satisfaction at 1 years postoperatively (MD = -1.67, 95% CI [-5.04, 1.71], P = 0.33), the pooled data were homogenous (P = 0.19, I² = 40%). fig. 3.
KSS function score at 2 years
Two studies reported the outcome with 187 total participants. The pooled results showed no statistically significant difference between mechanical and kinematic alignment in KSS function score at 2 years postoperatively (MD = -7.73, 95% CI [-16.06, 0.60], P = 0.07), the pooled data were homogenous (P = 0.16, I² = 49%). fig. 3.
Oxford score
Oxford score at 6 months
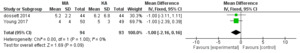
Two studies reported the outcome with 129 total participants. The pooled results showed no statistically significant difference between mechanical and kinematic alignment in Oxford score at 6 months postoperatively (MD = 3.02, 95% CI [-4.82, 10.86], P = 0.45), the pooled data were heterogeneous (P = 0.005, I² = 87%). fig. 4.
Oxford score at 2 years
Four studies reported the outcome with 316 patients. The pooled results showed no statistically significant difference between mechanical and kinematic alignment in Oxford score at 2 years postoperatively (MD = -1.79, 95% CI [-4.17, 0.58], P = 0.41), the pooled data were heterogeneous (P = 0.06, I² = 60%). The heterogeneity was solved by removing Dossett 2014 (P = 0.89, I² = 0%). and the effect estimate remained not significant (MD = -0.60, 95% CI [-1.98, 0.78], P = 0.39) fig. 4.
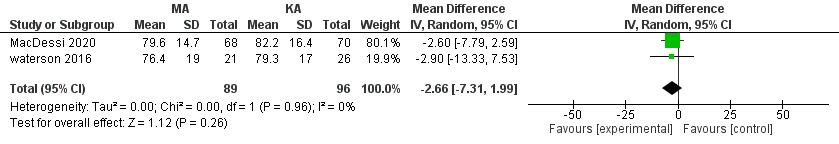
KOOS score at 1 year
Two studies reported the outcome with 185 patients. The pooled results showed no statistically significant difference between mechanical and kinematic alignment in KOOS score at 1 year postoperatively (MD = -2.66, 95% CI [-7.31, 1.99], P = 0.26), the pooled data were homogeneous (P = 0.96, I² = 0%). fig. 5.
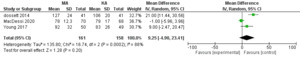
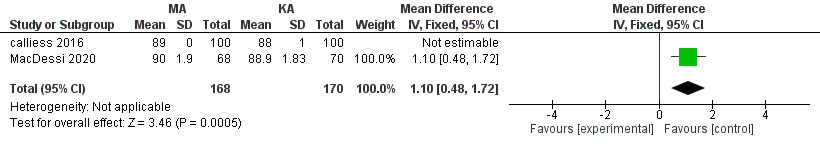
mMPTA at 12 months
Two studies reported the outcome with 338 patients. The pooled results showed significantly greater mMPTA with mechanical alignment at 1 year postoperatively (MD =1.10, 95% CI [0.48, 1.72], P = 0.0005). fig. 6.
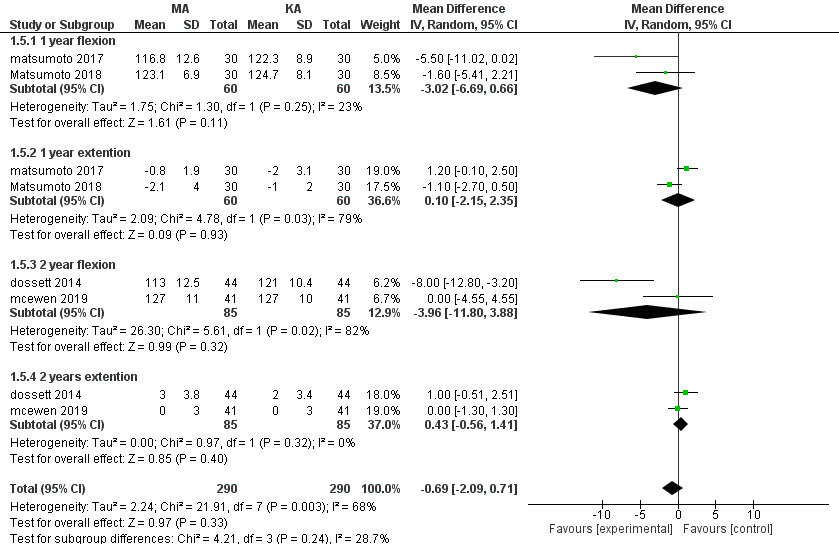
Range of motion
At one year
Two studies reported the outcome with 120 patients. The pooled results showed no statistically significant difference between mechanical and kinematic alignment in flexion (MD = -3.02, 95% CI [-6.69, 0.66], P = 0.11) with homogenous data (P = 0.25, I² = 23%), and extension (MD = 0.10, 95% CI [-2.15, 2,35, P = 0.58) with heterogeneous data (P = 0.03, I² = 79%). fig. 7.
At two years
Two studies reported the outcome with 170 patients. The pooled results showed no statistically significant difference between mechanical and kinematic alignment in flexion (MD = -3.96, 95% CI [-11.80, 3.88], P = 0.32) with heterogeneous data (P = 0.02, I² = 82%), and extension (MD = 0.43, 95% CI [-0.56, 1.41], P = 0.40) with homogenous data (P = 0.32, I² = 0%). fig. 7.
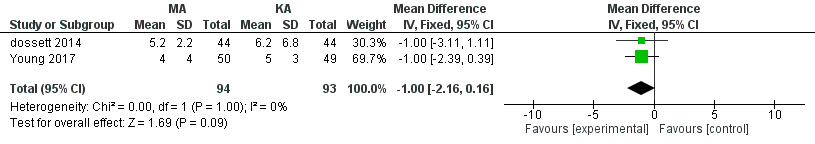
Length of stay
Two studies reported the outcome with 187 patients. The pooled results showed no statistically significant difference between mechanical and kinematic alignment in Length of stay (MD = -1.00, 95% CI [-2.16, 0.16], P = 0.09), the pooled data were homogeneous (P = 1.00, I² = 0%). fig. 8.
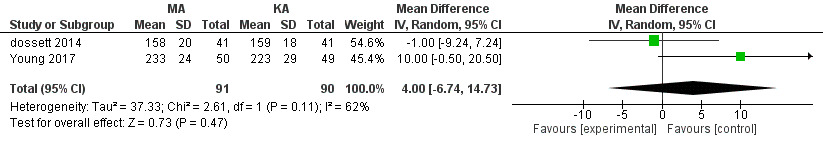
Incision length
Two studies reported the outcome with 187 patients. The pooled results showed no statistically significant difference between mechanical and kinematic alignment in Incision length (MD = 4.00, 95% CI [-6.74, 14.73], P = 0.47), the pooled data were heterogeneous (P = 0.11, I² = 62%). fig. 9.
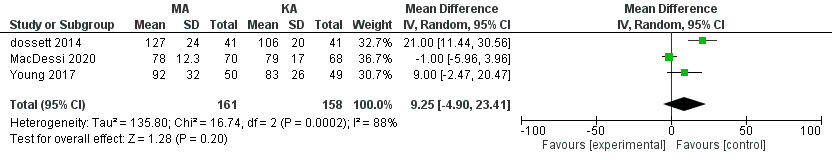
Duration of surgery
Three studies reported the outcome with 319 patients. The results showed no statistically significant difference between mechanical and kinematic alignment in the duration of surgery (MD = 9.25, 95% CI [-4.90, 23.41], P = 0.20), the pooled data were heterogeneous (P = 0.0002, I² = 88%). fig. 10.
Results of the qualitative analysis
Three randomized controlled trials reported long term follow up results of kinematic alignment versus mechanical alignment in total knee arthroplasty. Yeo 2018 reported 8 to 9 years results as follow: HSS (MA = 94.8±5.5, KA = 93.2±8.0), WOMAC score (MA = 20.4±1.8, KA = 19.3±1.9), ROM (MA = 129.0±11.5, KA = 125.0±11.5), KS pain (MA = 47.2±7.5, KA = 47.5±5.6), KS function (MA = 93.0±9.1, KA = 90.1±10.5). the difference was not statistically significant between the two groups in all reported scores. Moreover, the radiological and gait analysis results showed no statistically significant difference except for the Coronal femoral and tibial inclination. Young 2020 reported 5 years follow up results that showed no statistically significant difference in any patient reported outcome measure between mechanical and kinematic alignment. Dossett 2023 reported outcomes at 13 years follow up that also showed no statistically significant difference in any patient reported outcomes, and no difference between the 2 alignment methods for major and minor reoperations, with kinematically aligned total knees self-reporting a non-statistically significant (P ¼ .16) improved satisfaction (96% versus 82%).
Discussion
MA TKA relies on restoring the hip–knee–ankle angle of the limb to neutral under static weight-bearing conditions.29 However, only 0.1% of patients have a neutral mechanical axis therefore MA change most patient’s native anatomy.30 KA is an alternative technique that produces anatomic rather than arbitrary component positions.16,27 Thus in this systematic review and meta-analysis we assessed self-reported clinical and radiological outcomes of MA compared to KA in patients undergoing TKA.
Our results showed no significant difference between MA and KA in KSS score at six months, one and two years for combined, patient satisfaction and function scores. The outcome was reported in eight studies with most studies showing no statistically significant difference between the two groups. However, Calliess et al stated a significantly better KSS with KA measured one year postoperatively.15 Dosset et al reported KSS at different time points showing significantly better KSS with KA at six months16 and two years17 postoperatively. But on long term follow up at 13 years they reported no significant difference between MA and KA in terms of pain, function, or satisfaction.18 Our results are different from what was previously reported by Essen et al showing better KSS with KA, however the later meta-analysis included RCTs and cohort studies at different follow up period.31
Oxford and KOOS scores were not significantly different between the two groups. All pooled studies reported the same findings except Dosset et al that showed significantly better Oxford and KOOS scores with KA at six months16 and 2 years17 postoperatively. Our results are similar to the previous meta-analysis by Liu et al showing no significant difference between KA and MA in Oxford and KOOS score across different domains.32
The mean mMPTA is 87.5° varus with a range of 85°–90° in normal knees.33 Two studies reported mMPTA values, at six months postoperatively the reported values lied within the normal range. MacDessi et al. showed that KA group had a significantly greater mean varus angulation.21 On the other hand, Calliess et al reported that KA group demonstrated an average post-operative alignment of 1° ± 3° valgus.15 The previous meta-analysis also reported a significant difference between the two groups showing greater mLDFA with MA.32
The most important outcome to assess the functional ability of the patients after total knee arthroplasty is the range of motion. A minimum of 90° range of knee flexion is essential to maintain the daily activities.34 the range of motion is primary affected by the patient’s age, BMI and baseline KSS alongside the implant design, surgical techniques and postoperative rehabilitation.35 According to our results the difference in the range of motion was not significantly different between the two groups, showing non significantly more flexion range with KA and slightly more extension range with MA.36 This is similar to the previous study by Luo et al that showed no significant difference in ROM. However, another study by Gao et al reported significantly greater flexion ROM with KA.37
Surgical duration has a significant impact on patient’s outcome. Prolonged TKA was reported to carry a high risk of infection.38,39 Moreover, incision length and the length of hospital stay plays a significant role in patient’s satisfaction. We found no statistically significant difference between MA and KA in duration of surgery, incision length, and the length of hospital stay. Our results are similar to the findings reported by the previous meta-analysis.32
Strength: firstly, we included only Randomized controlled trials. Secondly, we assessed the reported outcomes at different time points separately and qualitatively reported the results of studies not matched for meta-analysis group. And finally, most of our included studies demonstrated a good quality.
Limitations: The significant heterogeneity encountered during assessment of most reported outcomes. Moreover, due to the small number of included studies we could not perform a sensitivity analysis. thus more RCTs with large sample size are needed to further validate our findings.
Conclusion: there is no significant difference between KA and MA in different clinical outcome scores, range of motion, length of stay, incision length or the duration of surgery.