Introduction
Cervical radiculopathy is a condition characterized by pain, numbness, or weakness radiating from the neck into the upper extremities. This typically results from compression or irritation of the cervical nerve roots.1 Common etiologies include herniated intervertebral discs and degenerative changes in the cervical spine.2 Conservative treatment modalities for cervical radiculopathy often include physical therapy and a variety of oral analgesics. However, when these interventions fail to provide adequate relief, interventional procedures may be considered. Among these, cervical epidural steroid injections (CESIs) are a popular approach for reducing inflammation and alleviating nerve root compression.2,3 Interlaminar epidural steroid injections are a specific type of CESI that involves the delivery of corticosteroids into the epidural space via the interlaminar approach, targeting the area around the inflamed nerve roots. This approach allows for the potential spread of medication over multiple affected levels, making it particularly useful in cases where radicular symptoms are diffuse or multi-level.
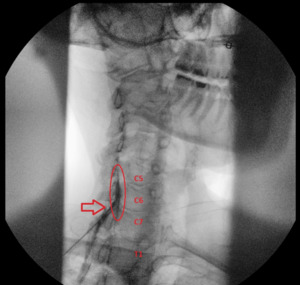
This case report details the application of an interlaminar CESI in treating a patient with cervical radiculopathy. Initially, the procedure revealed inadequate contrast flow, which could have led to suboptimal treatment if the needle had not been repositioned. This case emphasizes the critical importance of achieving proper contrast flow patterns to ensure optimal patient outcomes.
Case Presentation
The patient is a female in her early 60’s who presented with complaints of radiating pain and discomfort in her left upper extremity for six months consistent with C5/6 and C6/7 radiculopathy. Her pain was constant and interfered with her ability to work. She had tried physical therapy for 6 weeks without relief. She also tried oral analgesics including acetaminophen 1,000 mg three times a day, ibuprofen 400 mg three times a day, and gabapentin 300 mg three times a day without improvement. She underwent a cervical spine MRI which demonstrated a central disc bulge at C5/6 and a left paracentral disc protrusion at C6/7. Given failure of conservative management, she opted to proceed with an interlaminar CESI.
The patient was placed in a prone position, and the target area was cleaned with chlorhexidine. Under fluoroscopic guidance, the needle was advanced into the epidural space at the C7/T1 level. However, upon injection of contrast, the flow was noted to be inadequate with minimal cephalic spread, indicating suboptimal coverage of the targeted levels (Figure 1).
Given that the pathology was at C5/6 and C6/7, the needle was carefully withdrawn and repositioned at the C6/C7 interspace. A second injection of contrast demonstrated improved flow, with adequate spread to cover both the C5/6 and C6/7 levels (Figure 2).
Once optimal contrast distribution was confirmed, 80 mg of triamcinolone acetonide, 1 mL of 0.25% bupivacaine, and 1 mL of saline were injected into the epidural space. The patient tolerated the procedure well without any immediate complications. At the follow-up visit three weeks later, she reported a 90% reduction in her radicular symptoms, indicating a significant improvement in both pain and functional status. In addition, the patient was able to reduce her use of oral analgesics, minimizing her dependence on medication for pain control. This allowed her to resume her ongoing physical therapy exercises, further enhancing her recovery and functional mobility.
Discussion
Interlaminar CESIs are most commonly performed at the C7/T1 due to its favorable anatomical characteristics. The C7/T1 interspace is typically the widest and most easily accessible interlaminar space in the cervical spine.4 A critical aspect of performing CESIs safely and effectively is the observation and interpretation of contrast flow patterns during the procedure. The flow pattern of the contrast agent is crucial because it provides information about the anatomy of the epidural space, the presence of any anatomical abnormalities, the correct placement of the needle, and the site and spread of medication delivery.
This case underscores the importance of careful needle placement and contrast flow assessment during cervical epidural steroid injections. The initial inadequate contrast flow at the C7/T1 level could have resulted in suboptimal treatment had the needle not been repositioned. By adjusting the needle placement to the C6/C7 level, effective coverage of the C5/6 and C6/7 levels was achieved, leading to significant symptom relief for the patient. It is worth noting that the patient had disc protrusions at C5/6 and C6/7, likely contributing to canal stenosis, which may have impeded the flow of contrast and steroid medication. An alternative approach would have been to introduce a catheter through the epidural needle, advancing it to the targeted spinal level to ensure accurate drug delivery.5,6 However, in this particular case, we did not have the necessary equipment at the time of the procedure. The decision to proceed without a catheter was made after considering the situation, and needle repositioning was chosen to ensure adequate drug delivery.
Ensuring optimal contrast flow is critical in CESI procedures to ensure that the medication reaches the intended nerve roots. This case also illustrates the efficacy of CESI in managing cervical radiculopathy, particularly when performed with careful attention to technique and contrast flow patterns.
Conclusion
Cervical epidural steroid injections can be a highly effective treatment for cervical radiculopathy when performed with precision. This case demonstrates the importance of adequate contrast flow assessment and needle repositioning to ensure optimal drug delivery and achieve significant symptom relief. The patient’s positive outcome emphasizes the value of this approach in the management of radicular pain.