Introduction
Fractures are well understood to warrant time-sensitive treatment – some of which can be life or limb threatening if not addressed in an expeditious manner.1,2 Some of these fractures, in addition to traumatic soft tissue injuries, are often treated by sports medicine surgeons on an urgent basis.3–5 Many of these injuries have the potential to cause long-term limb dysfunction and disability if not treated in a timely fashion. Therefore, surgical intervention is generally considered non-elective and requires urgent or even emergent initial intervention. In this review, we describe these injuries as “sports medicine trauma” to highlight the severity of these injuries, as well as the importance of timely intervention. The purpose of this review is to highlight commonly encountered upper extremity sports medicine traumatic injuries, provide recommendations for treatment, and the rationale for expedited intervention.
Glenohumeral Joint Dislocations
Epidemiology
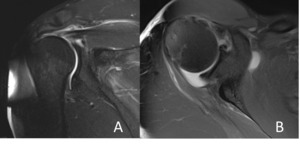
Anterior dislocations are the most common direction of dislocation, comprising up to 97% of shoulder dislocations, and require emergent reduction.6 The most common lesions are of the anterior-inferior labrum (Bankart lesion) and of the posterior superior humeral head (Hill-Sachs lesion) (Figure 1). However, fractures or massive tears of the rotator cuff tendons may also occur.7 Additionally, axillary nerve injury has been noted in about 42% of acute anterior shoulder dislocations.8 Anterior shoulder dislocations occur when the arm is in an abducted and externally rotated position and an anterior force is applied to the shoulder. Patients present with the arm adducted and internally rotated.
Posterior dislocations are less common with a prevalence of 1.1 per 100,000 population per year.9 Posterior shoulder dislocations occur more commonly due to a fall from height or motor vehicle accident with a posterior force directed to the shoulder with the arm in extension. Seizure activity can result in posterior shoulder dislocation while sports injuries are a relatively uncommon mechanism.9
While most shoulder dislocations can be treated with closed reduction, there is a subset requiring acute operative intervention, such as the locked dislocation or the inability to maintain reduction. Locked dislocations tend to be posterior, whereas a reverse Hill-Sachs lesions is engaged on the glenoid rim.10
Treatment
Initial imaging prior to intervention should include antero-posterior, lateral, scapular Y, and axillary or Velpeau view radiographs. Early reduction is critical in the management of shoulder dislocation, both to decrease the risk of unstable reduction and to minimize damage to surrounding soft tissue and neurovascular structures.11 There are a multitude of described reduction techniques, though no optimal maneuver has been established.8 Traction-countertraction is commonly used, as is the Stimson maneuver which involves hanging weight from the affected arm while the patient is in the prone position. Procedural sedation is often required to facilitate reduction and maximize patient comfort.
Regarding anterior shoulder instability, initial treatment for the first time dislocator should be individualized to the goals of the patient, although recurrence rates have been noted to be greater than 75% within at-risk populations without operative treatment.12,13 These decisions can be made on a routine basis without implications for urgency. Factors guiding operative treatment involve patient characteristics, glenoid bone loss, Hill-Sachs lesions, and consideration of on-track versus off-track lesions.14 Irreducible dislocations, on the other hand, should be taken to the operating room for attempted closed versus open reduction. Open reductions, which may be required in cases of tendon entrapment or bony fragments in the joint space, typically proceed through a deltopectoral approach with manual disimpaction of soft tissue or bony components in the joint space.15 In some cases, repair of damaged rotator cuff tendons or capsular repair may be required for soft tissue stabilization of the shoulder joint.16 Reduction of a locked shoulder dislocation should proceed within 48 hours. Studies have shown a higher rate of avascular necrosis of the humeral head in patients with a treatment delay beyond 48 hours.17
Acute Traumatic Rotator Cuff Tears
Epidemiology
Acute traumatic rotator cuff tears (ATRCT) are generally accepted to be injuries to the rotator cuff due to a specific event within the prior 6 months.18 Traumatic tears are caused by an acute trauma upon an already diseased tendon.19 Patients with ATRCTs are typically younger relative to patients with degenerative tears with an average age of 55, and are more commonly male.18 Typical injury mechanisms include forced abduction and external rotation, glenohumeral dislocation, or fall on an outstretched hand.18 Patients aged >40 years who have an anterior dislocation demonstrate rotator cuff tear rates of 35% to 86%.20 Patients in whom an ATRCT is suspected should undergo magnetic resonance imaging (MRI).21
Treatment
Surgical treatment for patients with full thickness ATRCTs >10mm has better long term functional outcomes when compared to conservative management.22–24 Operative management of ATRCTs has shown the best outcomes when done within 3 weeks of injury and has significantly worse outcomes if completed over 4 months after injury.25–27 Patients may have improvement in pain and function with physical therapy, however risk of tear progression and the development of muscle atrophy over time may compromise long term outcomes.28 If proceeding with conservative management, recommendation is for repeat advanced imaging at 12-18 months to evaluate tear progression and muscle atrophy.29
Generally, an initial trial of non-operative management for acute partial thickness rotator cuff tears less than 10mm is recommended.30 A recent randomized controlled trial showed equal results at 1 year with surgical repair and physiotherapy for acute traumatic partial thickness rotator cuff tears with a mean size of 9.7mm, however the authors noted tear progression greater than 5mm in 7 of 24 non-operative patients, and the development of fatty infiltration in 8 of 24.31 Tear progression and fatty degeneration are the chief concerns of non-operative rotator cuff management as these factors influence both patient outcomes and late repair outcomes. Ultimately, the decision to recommend repair or conservative management still must be a patient-centered shared decision for partial thickness tears. There is evidence to suggest, however, that younger, active patients with partial ATRCTs <10mm will likely benefit from repair over conservative management.32
Sternoclavicular Joint Dislocation
Epidemiology
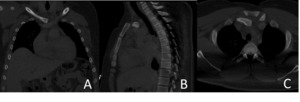
Sternoclavicular (SC) joint dislocations are rare injuries occurring in less than 3% of shoulder girdle injuries. Dislocations occur more than 80% of the time during sports participation through both direct and indirect mechanisms, predominantly in contact athletes, and occur in less than 1% of severely injured trauma patients.33,34 SC dislocations have been associated with severe thoracic injuries and are missed on initial evaluation 9% of the time.33
Posterior dislocations are up to nine times less common than anterior ones, although they can be life threatening and treating physicians should monitor closely for signs of compression of adjacent structures which can occur in up to 30% of posterior cases.35,36 Symptoms to monitor for include dyspnea, dysphonia, dysphagia, odynophagia, neurological dysfunction, or vascular congestion.34,37,38 Imaging should include radiographs with serendipity views to identify the presence of dislocation with a low threshold in equivocal cases to obtain an axial computed tomography (CT) scan, preferably with contrast, to identify potential injury to vascular structures.36
Treatment
Immediate stabilizing procedures depend on presenting symptoms and severity of injury. In low-grade sprains (Allman grade 1-2 injuries), sling immobilization from 1-6 weeks is advised. Failure to reduce SC dislocations, however, has been associated with poor outcomes.38
In both anterior and posterior dislocations (Allman grade 3 injuries), attempts at closed reduction should be performed in all identified cases and are successful in 38%.38 In the setting of hemodynamic instability, respiratory compromise, or asymmetric perfusion, a reduction attempt should be performed emergently. In the absence of these symptoms, reduction should be attempted on an urgent basis. In both cases, reduction should be performed in collaboration with a cardiovascular surgeon under general anesthesia. With regards to timing, closed reduction is more successful in the first 48hrs, but has been successful up to 10 days after dislocation.38
Failure to reduce is an absolute indication for open reduction in posterior dislocations and a relative indication in anterior dislocations.38 Long term sequelae of persistent dislocation include arthritis and recurrent instability, which are indications for surgery if symptomatic following failure of conservative management.36 Following any reduction attempt, serendipity views should be repeated in the procedural room followed by post-reduction CT to confirm stability of the reduction. Patients are typically immobilized postoperatively for a period of 4-6 weeks with sling, with or without swathe, before progressing range of motion. Clearance for sporting activities often occurs at 3-4 months postoperatively.34
Type 4-6 Acromioclavicular Injuries
Epidemiology
Acromioclavicular (AC) joint injuries account for 40-50% of shoulder injuries in athletes.39 These injuries are characterized by the Rockwood classification which correlates increasing soft-tissue disruption with the degree of radiographic displacement. Rockwood types I and II represent low-grade injury patterns with sprains of the AC and coracoclavicular (CC) ligaments resulting in minimal superior clavicular displacement. Type III injuries result in complete disruption of the AC and CC ligaments, but less than 100% displacement of the clavicle superiorly. Rockwood types IV, V, and VI represent high-grade injuries with complete disruption of the adjoining soft-tissue stabilizers and excessive posterior, superior, or inferior clavicular displacement respectively.40
Treatment
Surgical intervention is generally considered for high-grade injuries (IV-VI). Over 100 different surgical techniques have been described to address AC joint pathology, to include hook plate fixation, suspensory devices, and ligamentous reconstructions.41 All techniques intend to diminish the coracoclavicular interval, thereby restoring the normal articulation of the acromioclavicular joint. More current techniques tend to favor the use of a combination suture and hardware in a suspensory fixation format. The addition of either autograft and allograft to reconstruct both the coracoclavicular and acromioclavicular ligaments is commonly performed, although not definitively beneficial. In the end, however, the preferred treatment algorithm to include optimal timing of such procedures for high-grade injuries remains unclear.
A systematic review comparing early versus delayed surgical management of AC joint injuries demonstrated significantly superior functional outcomes associated with early compared to delayed operative intervention.42 The authors also noted a higher rate of loss of reduction associated with delayed (38.1%) compared to early (26.0%) fixation. In contrast, Lädermann et al found equivalent clinical outcomes when comparing early and delayed reconstruction of high-grade AC joint injuries, which the authors suggested was attributable to more modern surgical techniques.43 Similarly, Krul et al reported no significant delay in return to duty amongst active duty military personnel who underwent CC ligament reconstruction in a delayed fashion for high-grade AC joint pathology.44 Interestingly, the authors also indicated that conservative management was successful in most patients, which has been corroborated by other larger scale studies.45,46 Extrapolating these findings to athletes, more aggressive, acute treatment algorithms may be considered for this high-demand population.47 A meta-analysis of 12 studies evaluating 315 athletes reported comparable rates of return to sport associated with acute and chronic operatively treated AC joint injuries ranging from 94-100%, with a return to pre-injury level ranging from 62-100%. Less reliable return to sport has been noted amongst overhead athletes with high-grade AC joint injuries, as well as a longer required course of rehabilitation and a higher likelihood of reducing activity intensity or frequency.48
Pectoralis Major Rupture
Epidemiology
Rupture of the pectoralis major tendon has become increasingly prevalent in the last few decades.49,50 The mechanism of pectoralis major rupture often occurs with forced abduction and external rotation.51,52 Tears can occur at the humeral insertion, musculotendinous junction, or the muscle belly. The tears reported at the humeral insertion site are often complete,53 while myotendinous tears have been reported to be complete in about 20% of cases.54,55
Treatment
The location of the tear, extent of tear (partial or full), and clinical picture of the patient are the guide operative versus nonoperative treatment with young active individuals being more likely to benefit from operative intervention.55–57 Partial tears can be repaired surgically with success for those who wish to maintain full strength and continue high activity levels.58–60 There is an abundance of literature supporting the benefits of surgical repair for complete tears, especially those at the insertion site.49,61,62 These studies demonstrate increased strength, increased return to full participation in sport, and decreased pain in athletes when compared to nonoperative treatment.
Emphasis is placed on early repair for the best chance of excellent results.50,51,63 Generally, better results can be achieved with diagnosis and repair performed within eight weeks of initial injury due to the scarring, fibrosis, and adhesions commonly seen after this period.56,59,64 Additional studies have suggested that in patients with surgery performed before six weeks demonstrate improved outcomes when compared with delayed repair.50 Notably, those treated with delayed repair still showed better outcomes than those treated nonoperatively.50,63
Re-approximation at the tendo-osseous junction is commonly performed through transosseous suture repair (TOS) with the option of bone trough, cortical button fixation, or suture anchors.59,65–67 Overall, all three techniques are proven to be acceptable options with conflicting evidence to support the superiority of one over the other. Acute tears at the myotendinous junction can be successfully repaired with direct suturing to the tendon stump when possible.57,68,69 Alternatively, fixation to the humerus, as in the tendo-osseous rupture approach, can result in successful outcomes through sutures, anchor fixation, buttons, or washers and screws.63,68,70 Increased chronicity (greater than 8 weeks) and tears at the myotendinous junction increase the likelihood of reconstruction using autograft or allograft.50,59
Distal Biceps Rupture
Epidemiology
Distal biceps ruptures occur at a rate of 1.2-9.6 per 100,000 person-years.71–74 This injury predominantly occurs in middle-aged males, and has an increased associated risk among smokers and anabolic steroid users.71,73 Typically an avulsion of the distal biceps tendon occurs when an eccentric load is placed against a flexed elbow.73 Patients may report hearing an audible pop with pain over the anterior elbow and experience decreased strength in supination and flexion.71,74 On physical examination, findings may include ecchymosis about the antecubital fossa, retraction of the biceps muscle proximally known as a reverse Popeye deformity, as well as a positive Hook test. The Hook test is 100% sensitive and specific for the diagnosis of distal biceps rupture, however, MRI with the elbow flexed and forearm supinated may be helpful to further characterize the injury.75
Treatment
For the majority of distal biceps tendon ruptures, surgical treatment is recommended. Non-operative treatment of distal biceps rupture results in loss of 40% supination strength and 30% of flexion strength, and is reserved for patients who are poor surgical candidates or low-demand.76,77 Outcomes after surgical repair of distal biceps rupture demonstrate return to pre-injury levels of flexion and supination strength, 97.5% return to sport amongst athletes,72 and low rate of re-rupture (1.5%).78,79 Primary repair is preferred within the first few weeks after injury to optimize surgical approach by preventing the need for extensive dissection or need for augmentation of the repair.80 Tendon retraction and associated adhesions can present a surgical challenge as early as 4-6 weeks after injury.80 In a systematic review by Bajwa et al., 20% of patients undergoing repair of chronic distal biceps rupture had either a transient or permanent lateral antebrachial cutaneous nerve (LABCN) neuropraxia.81
Triceps Rupture
Epidemiology
Rupture of the distal triceps tendon is rare, estimated at about 1% of all tendon ruptures.82 Most reports have been associated with anabolic steroid use, weightlifting, and laceration, however, chronic systemic illnesses associated with tendon weakening have also been described.83–85 Injury commonly occurs with forceful eccentric contraction such as bench pressing or fall on an outstretched hand.85 Patients often describe a tearing or painful pop and ecchymosis over the posterior elbow. Other exam findings include a lack of passive elbow extension with the triceps squeeze test.86
Radiographs of the elbow may show the flake sign – a small fleck of bone avulsed from the olecranon, which is pathognomonic of the triceps rupture and present in > 60% of patients.86–88 Given the superficial location of the triceps tendon, ultrasound can be used to aid in diagnosis. Magnetic Resonance Imaging (MRI) has long been considered the most accurate modality for diagnosis and preoperative planning.85,88,89
Treatment
Treatment of these injuries should be individualized to the patient’s functional and medical status and injury severity. Partial ruptures with intact extensor mechanisms may be treated non-operatively with splint immobilization for four weeks.90,91 Urgent primary repair is indicated for most active patients or patients with complete tears and extension weakness. Primary repair is ideal within 2-3 weeks from injury.85,87,88 Restoration of the anatomic footprint results in significantly less motion at the repair site with cyclic loading.85,92 Outcomes after triceps tendon repair are generally successful, with 89% return to preinjury activity with rerupture rate estimated at 6%.87 The most common complication is continued pain, numbness, and/or swelling.
Conclusion
While many sports medicine surgeries are considered elective in nature, this review has highlighted several “acute sports trauma” injuries which require more urgent intervention (summarized in Table 1). In many of these injuries, the expedience of treatment directly impacts the subsequent functional performance of an individual, and sub-optimal outcomes in this regard can greatly affect quality of life. A recognition of pathology which requires timely intervention is therefore critical to allow the sports medicine surgeon to deliver optimal care.
Author Contributions
RR manuscript authoring: JF manuscript authoring; RP manuscript authoring; PM manuscript authoring; SF manuscript authoring; NP manuscript authoring; BL manuscript authoring; SR manuscript authoring; DL manuscript authoring; CP manuscript authoring; RS manuscript authoring; RW manuscript authoring; JE manuscript authoring/corresponding author
Study Approval
Not required - Review Article
Study Funding
No funding was obtained for the completion of this study.
Color publication
The figures in this manuscript DO require publication in color.
Results presentation
This review article has not been previously presented or published elsewhere

_axillary_radiograph_showing_posterior__locked_dislocation__b)_axi.tiff)
_and_coronal_(b)_pl.tiff)


_axillary_radiograph_showing_posterior__locked_dislocation__b)_axi.tiff)


_and_coronal_(b)_pl.tiff)

