Introduction
Lumbar radicular pain is a prevalent and often debilitating condition that can significantly impact patients’ quality of life. Epidural steroid injections (ESIs) are commonly used to manage this condition by delivering corticosteroids and local anesthetics into the epidural space, aiming to reduce inflammation and alleviate pain.1,2 Among the various ESI approaches, the caudal technique is frequently utilized due to its favorable safety profile and accessibility in patients with challenging anatomical considerations, such as those with a history of lumbar surgery, scoliosis, or significant degenerative stenosis.3,4 However, despite its advantages, the effectiveness of caudal ESIs can be inconsistent, with some patients experiencing only partial or short-lived relief. Alternative ESI approaches include the transforaminal and interlaminar techniques.5–7
One possible limitation of performing caudal ESIs using a spinal needle is suboptimal drug distribution. Medications may not fully reach the site of pathology due to inadequate volume being injected or anatomical barriers such as epidural adhesions or scarring limiting medication dispersion. In such situations, catheter-guided techniques can offer a more targeted medication delivery, allowing precise placement of the injectate toward the symptomatic side and affected nerve roots.8–10 This targeted approach could enhance clinical outcomes in patients who do not achieve satisfactory pain relief with standard caudal ESIs.
In this case series, we describe three patients with unilateral lumbar radicular pain who experienced suboptimal pain relief following initial caudal ESIs performed with a 22-gauge spinal needle. Each patient subsequently underwent a repeat caudal ESI utilizing an epidural catheter, allowing for more precise medication delivery to the area of interest. We present their clinical responses and discuss the potential advantages of catheter-guided caudal ESIs as an alternative strategy for improving pain relief in select patients with lumbar radicular pain.
Case Series
Patient 1
A female in her mid-60s with unilateral lumbar radicular pain underwent a caudal ESI using a 22-gauge spinal needle. The injectate consisted of 3 mL of 0.25% bupivacaine, 3 mL of preservative-free normal saline (PFNS), and 2 mL of 40 mg/mL of triamcinolone. At the 2-week follow-up, the patient reported only a 30% improvement in pain symptoms. Due to the suboptimal response, a repeat caudal ESI was performed using an epidural catheter, which was advanced toward the symptomatic side and area of interest for more targeted medication delivery. The injectate for the repeat procedure included 2 mL of 0.25% bupivacaine, 1 mL of PFNS, and 1.5 mL of 40mg/mL of triamcinolone. At the 2-week follow-up after the repeat injection, the patient experienced 70% pain relief.
Patient 2
A male in his mid-60s with unilateral lumbar radicular pain underwent an initial caudal ESI using a 22-gauge spinal needle. The injectate consisted of 3 mL of 0.25% bupivacaine, 5 mL of preservative-free normal saline, and 2 mL of 40 mg/mL of triamcinolone. The patient initially reported an 80% reduction in pain, but this relief lasted only 3 days, with symptoms returning to baseline by the 2-week follow-up. Given the short duration of relief, a repeat caudal ESI with an epidural catheter was performed to allow for more precise medication delivery to the symptomatic region. The injectate for the repeat procedure included 2 mL of 0.25% bupivacaine, 1 mL of PFNS, and 1 mL of 40 mg/mL of triamcinolone. At the 2-week follow-up after the repeat injection, the patient reported 60% pain relief, indicating improved and sustained symptom control compared to the initial procedure.
Patient 3
A male in his early 70s with unilateral lumbar radicular pain underwent a caudal ESI using a 22-gauge spinal needle. The injectate consisted of 2 mL of 0.25% bupivacaine, 4 mL of preservative-free normal saline, and 2 mL of 40 mg/mL of triamcinolone. This resulted in 40% pain relief at the 2-week follow-up. Due to the moderate response, a repeat caudal ESI with catheter-guided delivery was performed, allowing the medication to be deposited directly at the affected site. The injectate for the repeat procedure included 2 mL of 0.25% bupivacaine, 1 mL of PFNS, and 1.5 mL of 40 mg/mL of triamcinolone. At the 2-week follow-up after the repeat injection, the patient reported 100% pain relief, with complete resolution of symptoms.
Outcomes are shown in Table 1.
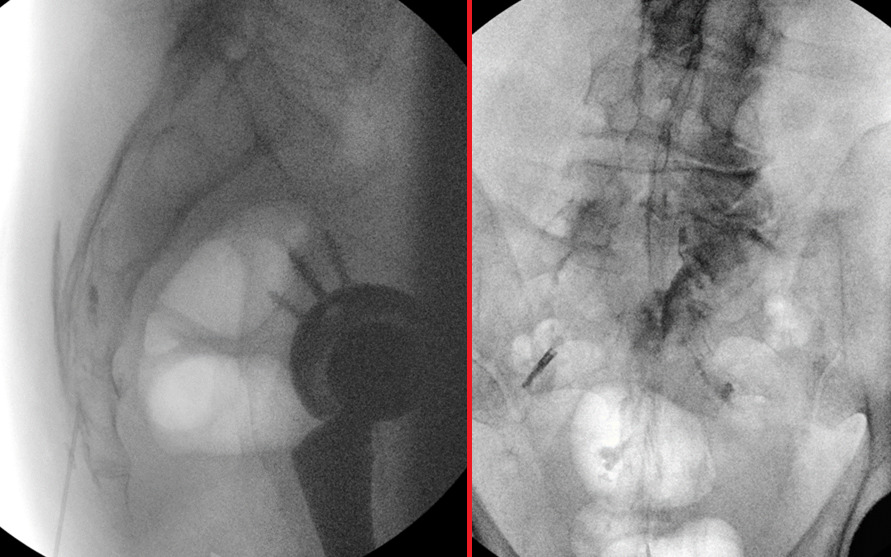
An example of the procedure, including fluoroscopic images demonstrating needle placement through the sacral hiatus and contrast spread following catheter advancement to the right L5/S1 region, is shown below in Figure 1.
The left image presents a lateral fluoroscopic view, demonstrating the advancement of an 18-gauge Tuohy needle through the sacral hiatus for caudal epidural access. The right image displays a post-contrast anteroposterior (AP) fluoroscopic view, showing the contrast spread after a 21-gauge epidural catheter was directed toward the right L5/S1 region, confirming targeted medication delivery.
Discussion
Caudal ESIs are widely used for managing lumbar radicular pain, particularly in patients with prior lumbar surgery, scoliosis, or degenerative stenosis where transforaminal or interlaminar approaches may be less feasible. However, the effectiveness of caudal ESIs can be variable, with some patients experiencing limited or short-lived relief. In cases where standard caudal ESIs using a spinal needle do not provide sufficient symptom improvement, alternative strategies such as catheter-guided injections may enhance pain relief by allowing more targeted medication delivery.
In this case series, three patients with unilateral lumbar radicular pain experienced suboptimal pain relief following initial caudal ESIs performed with a 22-gauge spinal needle. While one patient (Patient 2) initially reported 80% improvement, the relief was short-lived, lasting only three days before symptoms returned to baseline. The other two patients experienced only 30% and 40% relief at the 2-week follow-up. Given the incomplete responses, a repeat caudal ESI was performed in each patient using an epidural catheter, allowing for directed medication administration toward the affected side and region of pathology. This adjustment led to notable improvements in pain relief, with patients reporting 70%, 60%, and 100% symptom reduction at their respective 2-week follow-ups.
The improved outcomes following catheter-guided caudal ESIs may be attributed to several factors. First, directing the catheter toward the symptomatic nerve root or affected region allows for higher local drug concentration, potentially enhancing anti-inflammatory effects and reducing pain transmission more effectively. Additionally, traditional caudal ESIs rely on the diffusion of injectate within the epidural space, which may result in uneven or inadequate drug distribution, particularly in cases of unilateral radicular pain.7,8 The catheter technique overcomes this limitation by positioning the tip closer to the affected area, thereby improving medication deposition and optimizing therapeutic effects.8
While this case series highlights the potential benefits of catheter-guided caudal ESIs for patients with unilateral lumbar radicular pain, several limitations should be considered.
First, this study includes only three patients, limiting the findings’ generalizability. More extensive studies with more participants are needed to determine whether the observed benefits are consistent across a broader population. Additionally, the follow-up period was limited to two weeks post-injection. Although patients demonstrated improved pain relief after the catheter-guided approach, the long-term durability of these effects remains unknown. Further research with extended follow-up is necessary to evaluate whether symptom relief is sustained or if patients eventually require additional interventions.
Discussing the potential downsides of utilizing catheters when performing caudal ESIs is also essential. While catheter-guided caudal ESIs offer targeted medication delivery and possible improvements in pain relief, they also present several procedural challenges and risks. One obvious concern is the need for a larger-gauge Tuohy needle to accommodate catheter advancement, which may contribute to increased procedural discomfort for the patient. Additionally, advancing a catheter through the sacral hiatus and directing it toward the target region can prolong procedure time and increase radiation exposure. Using a catheter-based approach also necessitates additional equipment, including the catheter itself, which may increase procedural costs and serve as a barrier. Technical challenges associated with catheter advancement can further complicate the procedure. Forceful or aggressive catheter manipulation may lead to patient discomfort or, in rare cases, dural puncture or tear, increasing the risk of post-procedural headaches or other complications. Moreover, suppose the catheter needs to be withdrawn or repositioned after it has exited the Tuohy needle. In that case, there is a potential risk of catheter shearing, which could result in fragment retention within the epidural space. Given these risks, careful technique, adequate procedural training, and proper patient selection are essential to minimizing complications and optimizing outcomes when performing catheter-guided caudal ESIs.
Conclusion
This case series demonstrates the potential benefits of catheter-guided caudal ESIs in patients with unilateral lumbar radicular pain who experience suboptimal relief from standard caudal ESIs. The ability to target medication delivery to the symptomatic side may enhance pain relief and improve outcomes in select cases. Further studies are warranted to evaluate this approach’s long-term efficacy and patient selection criteria in clinical practice.