1. Introduction
Lumbar spinal stenosis is a degenerative spinal condition involving the narrowing of the central canal, lateral recess, or neural foramina, which can compress nerve structures, leading to significant pain, impaired mobility, and reduced quality of life.1 Standard management approaches for lumbar spinal stenosis include both conservative treatments, such as physical therapy and medication, and surgical interventions, with decompression surgery often pursued in cases where conservative treatment does not provide adequate relief.2,3 Decompression techniques can be divided into three main groups: open surgery without fusion, fusion-related open surgery, and minimally invasive decompression. Numerous studies, both in Vietnam and internationally, have affirmed the efficacy of open surgery with and without fusion for treating spinal stenosis. However, recent advancements in surgical techniques have catalyzed a shift toward minimally invasive options due to their clinical advantages, including reduced postoperative pain, shorter hospital stays, and faster recovery compared to traditional open surgery.
The emergence of full-endoscopic decompression techniques marks a significant advancement in minimally invasive spine surgery. Unlike open approaches, full-endoscopic decompression involves smaller incisions, less muscle disruption, and a reduction in postoperative scarring, while maintaining effective clinical outcomes.4–7 As a result, this approach is increasingly considered a standard alternative to conventional open surgery. However, publications from Vietnam assessing the efficacy of full endoscopic decompression for lumbar spinal stenosis, particularly using the outside in technique via the interlaminar approach, are scarce in the medical literature. Moreover, global evidence often focuses on specific patient populations and healthcare settings, with scarce data from developing countries, where resource constraints and demographic differences may influence treatment outcomes.
Given the potential for minimally invasive endoscopic techniques to optimize patient recovery, reduce hospital stays, and lessen the burden on healthcare systems, there is a pressing need for research assessing their effectiveness within diverse clinical settings, including Vietnam. This study aims to bridge this gap by evaluating the early outcomes of full-endoscopic decompression for lumbar spinal stenosis in a Vietnamese hospital setting. By documenting clinical outcomes and complications associated with this technique, we aim to provide insight into its applicability and potential benefits in a developing country context, offering a valuable contribution to both local and international discussions on minimally invasive spinal surgery.
2. Materials and Methods
2.1. Patients & Study Setting
From January to December 2024, a retrospective review was conducted on 25 consecutive patients with lumbar spinal stenosis who underwent full-endoscopic decompression at Viet Duc Hospital in Hanoi, Vietnam. Patients were eligible for inclusion if they were diagnosed with degenerative lumbar spinal stenosis, presenting with neurogenic claudication symptoms, accompanied by back pain and leg numbnes, and had failed at least 3 months of conservative treatment. MRI findings confirmed canal stenosis at the site corresponding to clinical symptoms, with a spinal canal cross-sectional area of less than 76 mm2. Patients with controlled comorbidities (e.g., diabetes, hypertension) were included if medically optimized, while those with severe osteoporosis (T-score < -3.0), spondylolisthesis (Meyerding grade ≥2), prior lumbar surgery, active infection, or spinal malignancy were excluded. Endoscopic decompression surgery was recommended for patients meeting one of the following criteria: (i) lumbar spinal stenosis with progressive neurological impairment, or (ii) lumbar spinal stenosis with persistent nerve root pain that had not responded to three months of medical treatment.
2.2. Demographic, Clinical & Radiographic Data
An analysis of demographic, clinical, and radiographic data included factors such as age, body mass index (BMI), lumbar syndrome, radicular pain, clinical localization of nerve root injury, movement disorders, nerve root palsy, muscle atrophy, dystonia, central and lateral spinal stenosis, the degree of canal stenosis, location of spinal stenosis, cross-sectional area, surgical approach, operative time, and length of hospital stay.
Clinical outcomes were evaluated using the Visual Analog Scale (VAS; ranging from 0 to 10) to assess pain, as well as the Oswestry Disability Index (ODI; ranging from 0% to 100%, with higher scores indicating more severe disability). Assessments of back and leg pain using the VAS, as well as evaluations of functional disability using the ODI, were conducted preoperatively, immediately postoperatively, and during follow-ups at three months and six months. The final outcome was evaluated using the Mac-Nab criteria at both the three-month and six-month follow-ups.
2.3. Surgical Technique
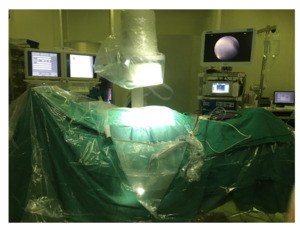
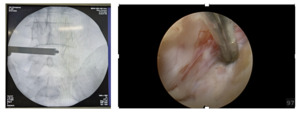
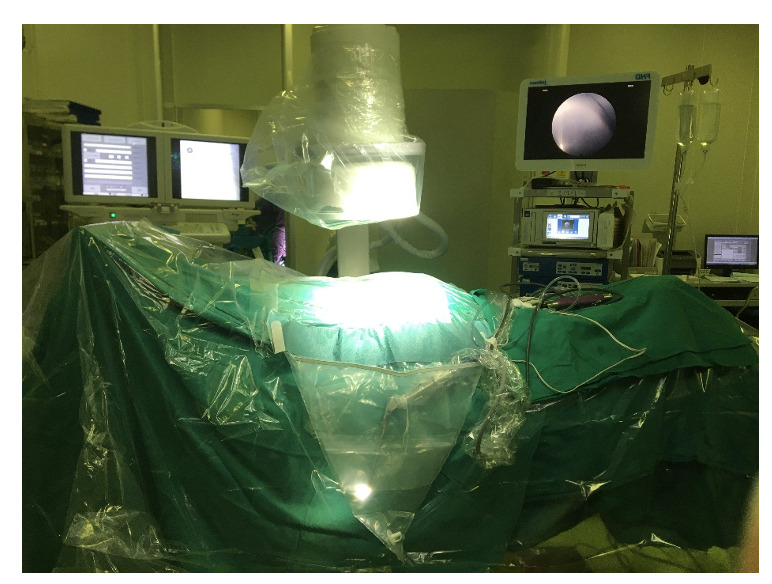
Patients were positioned prone under general anesthesia without muscle relaxation (Image 1). A SIEMENS Mobile C-arm (Model: Pb r8 N40 f090) operating in pulsed fluoroscopy mode (6 frames/sec) was used for real-time guidance, with last-image-hold function to minimize radiation exposure. The interlaminar entry point corresponding to the site of spinal stenosis was accurately located in two planes under fluoroscopy. Under fluoroscopic guidance, guidewires were inserted through the posterior lumbar musculature, with their tips directed toward the targeted operative space to facilitate the insertion of the working channel (Image 2).
The surgical approach (unilateral or bilateral decompression) was determined preoperatively based on: Unilateral approach: For patients with MRI-confirmed unilateral stenosis (lateral recess/foraminal compression) and contralateral neuroforaminal width >5mm; Bilateral approach: For central canal stenosis with bilateral symptoms or radiographic evidence of contralateral root compression (cross-over sign).
A diamond burr was utilized to resect the lower edge of the cranial lamina and the upper segment of the caudal lamina until the margins of the ligamentum flavum were exposed. The ligamentum flavum was then carefully removed. Facet joints and any anterior herniated disc fragments causing compression were resected to achieve effective decompression. In cases requiring additional stabilization, CP-ESP artificial discs were implanted following decompression.
Bilateral decompression was confirmed by verifying the absence of nerve root compression on both sides. Following confirmation of complete decompression of the lateral recess and foramen, as well as achieving adequate hemostasis, the endoscope and working cannula were removed. The skin was then sutured in layers. Postoperatively, patients were monitored for any complications, and standard care protocols were implemented to ensure optimal recovery.
2.4. Postoperative Management
Immediate Postoperative Care: All patients received standardized postoperative care immediately following surgery. Vital signs and neurological status were monitored every 2 hours for the first 24 hours. Intravenous fluids were maintained until oral intake was tolerated, typically within 6-8 hours postoperatively.
Pain Management Protocol: A multimodal analgesic regimen was implemented, consisting of intravenous paracetamol (1g every 8 hours) for the first 24 hours, followed by oral celecoxib (200mg twice daily) for 3 days. Rescue analgesia with tramadol 50mg was available as needed, though only required in 12% of cases. No patients required opioid medications beyond the third postoperative day.
Mobilization and Activity Restrictions: Patients were encouraged to ambulate with assistance within 6 hours after surgery. No spinal braces were prescribed. Activity restrictions included avoidance of heavy lifting (>5kg), twisting motions, and prolonged sitting for the first 6 weeks. Most patients achieved independent ambulation by postoperative day 1.
Rehabilitation Program: A phased rehabilitation protocol was initiated: Phase 1 (0-2 weeks) focused on isometric core stabilization and gentle range-of-motion exercises. Phase 2 (2-6 weeks) incorporated progressive strengthening under physiotherapist supervision. The mean time to return to light work was 4 weeks, with full activities resumed by 6-8 weeks (mean 6.05±0.82 weeks).
Follow-up Protocol: Structured follow-up included clinical evaluations at 1 week, 1 month, 3 months, and 6 months postoperatively. Each visit included VAS and ODI assessments. MRI was repeated at 3 months only for patients with persistent symptoms (none in this series). Final outcomes were evaluated using MacNab criteria at 3 and 6 months. No cases of surgical site infection, dural tears, or neurological complications were observed during follow-up.
2.5. Data Collection
Demographic, clinical, and radiological data were gathered during hospitalization. Preoperative clinical outcomes were assessed using the Visual Analog Scale (VAS; range 0 to 10) for pain evaluation8 and the Oswestry Disability Index (ODI; range 0% to 100%, with higher scores indicating more severe disability).9 Clinical data included age, body mass index (BMI), radicular pain, clinical localization of nerve root injury, movement disorders, nerve root palsy, muscle atrophy, and dystonia. Assessments were conducted preoperatively, immediately postoperatively, and at follow-ups at three months and six months.
Radiographic evaluations included measurements of disc height, segmental lordosis angle, overall lumbar lordosis, and the degree and location of spinal stenosis, all assessed using standing X-rays. Additionally, computed tomography (CT) scans were employed to measure facet joint line length and bilateral cross-sectional area at the mid-disc level. Canal cross-sectional areas were measured at the affected and adjacent levels, and any degree of listhesis was thoroughly examined. Dynamic X-rays were utilized to rule out spinal instability.
2.6. Statistical analysis
All statistical analyses were performed with the statistical package Stata. Data are expressed as the mean ± standard deviation for continuous variables. The quantitative variables were presented with frequency and percentage.
3. Results
Table 1 presents the demographic and preoperative characteristics of the study patients. A total of 25 patients were included in this analysis, with a mean age of 65.80 ± 8.41 years. The majority of the patients were male, comprising 16 individuals (64%), while 9 patients (36%) were female. Preoperative clinical symptoms included lumbar syndrome in 24 patients (96%), radicular pain in 25 patients (100%), and limited mobility (less than 500 meters) in 2 patients (8%). Muscle atrophy was observed in 1 patient (4%). The most common site of spinal stenosis was at the L4-L5 level, affecting 17 patients (68%), while 8 patients (32%) had stenosis at the L5-S1 level. Central canal stenosis was observed in 10 patients (40%), and the predominant causes of spinal stenosis were a combination of hypertrophy of the facet joints and ligamentum flavum thickening, identified in 9 patients (36%), along with combined disc herniation in 11 patients (44%).
Table 2 presents the intraoperative and postoperative characteristics of the study patients. The most common operated level was L4-L5, with 14 patients (56.00%), followed by L5-S1 with 9 patients (36.00%), and L3-L4 with 2 patients (8.00%). Unilateral decompression was performed in 20 patients (80.00%), while bilateral decompression was conducted in 5 patients (20.00%). The mean operative time was 50.96 ± 16.20 minutes, and the average length of hospital stay was 2.13 ± 0.52 days. The mean time to return to work was 6.05 ± 0.82 weeks. Importantly, there were no complications reported among the patients.
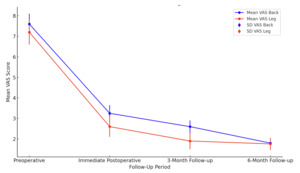
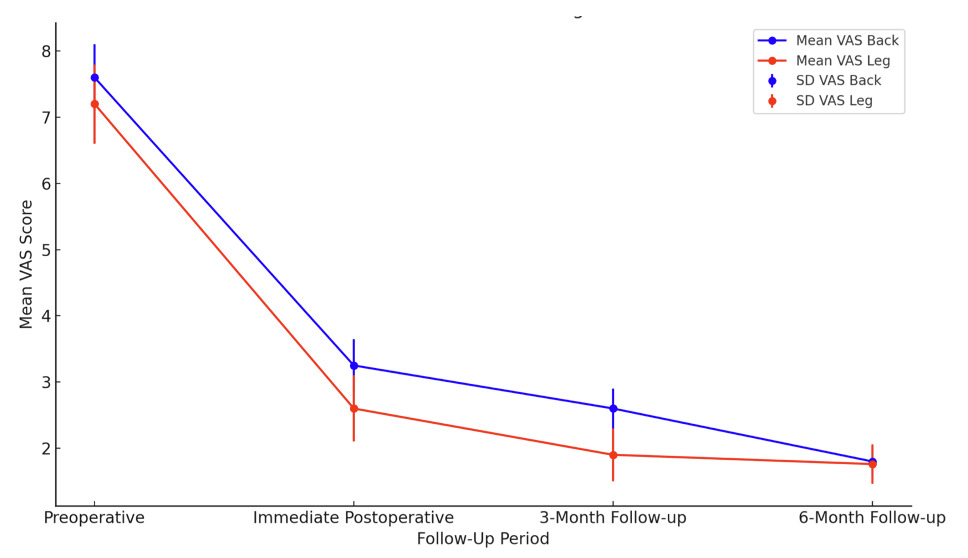
As was shown in Figure 1, the analysis of VAS scores for back and leg pain revealed significant reductions at each postoperative assessment following full-endoscopic decompression for lumbar spinal stenosis. The mean VAS score for back pain decreased from 7.60 preoperatively to 3.25 immediately postoperative, further reducing to 2.60 at 3 months, and finally reaching 1.80 at 6 months. Similarly, leg pain scores dropped from 7.20 preoperatively to 2.60 postoperatively, then to 1.90 at 3 months, and stabilized at 1.76 at 6 months.
The ODI scores demonstrated significant changes over time with a preoperative mean ODI of 76.35 that decreased to 18.15 immediately postoperative and further reduced to 13.98 at the 3-month follow-up before reaching 10.34 at the 6-month follow-up (Figure 2).
The Mac-Nab criteria at the 3-month follow-up indicated excellent outcomes in 17 patients representing 68 percent good outcomes in 6 patients representing 24 percent and fair outcomes in 2 patients representing 8 percent At the 6-month follow-up the criteria improved further with excellent outcomes in 20 patients representing 80 percent good outcomes in 4 patients representing 16 percent and fair outcomes in 1 patient representing 4 percent (Figure 3).
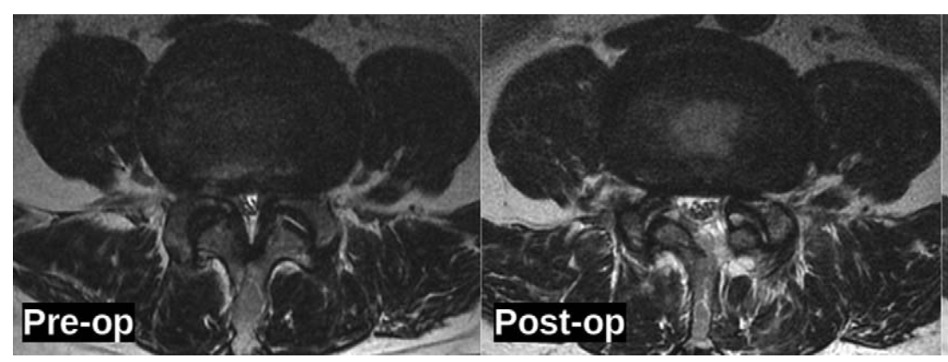
Table 3 presents the radiologic outcomes observed in patients undergoing full-endoscopic decompression for lumbar spinal stenosis. A significant increase in the canal cross-sectional area was noted postoperatively, with a mean area of 155.2 ± 32.2 mm² compared to the preoperative measurement of 75.78 ± 28.45 mm² (p <0.01). In terms of the intervertebral height index (IHI), preoperative values were recorded at 30.87 ± 5.49%, which slightly decreased to 30.28 ± 5.21% postoperatively; however, this change was not statistically significant (p >0.05). Regarding segmental angulation, measurements were obtained for both extension and flexion angles, with extension averaging 7.01° ± 1.74° and flexion measuring 6.51° ± 1.56°. Range of motion (ROM) was assessed, demonstrating a mean extension of 2.87 ± 0.53 mm and a flexion of 2.78 ± 0.54 mm. Facet joint dimensions were evaluated bilaterally, revealing a slight reduction in ipsilateral facet length from 14.8 ± 0.9 mm preoperatively to 14.4 ± 0.7 mm postoperatively, and minimal change in contralateral facet length from 14.9 ± 0.6 mm to 14.8 ± 0.6 mm. Neither change reached statistical significance (p >0.05), indicating that the surgical technique preserved facet joint integrity. Lastly, the Pfirrmann classification system indicated no change in disc degeneration status.
4. Discussion
The study presents compelling evidence of the effectiveness of full-endoscopic decompression for lumbar spinal stenosis, demonstrating significant improvements in both clinical and radiologic outcomes. The mean VAS score for back pain decreased dramatically from 7.60 preoperatively to 1.80 at the 6-month follow-up, while the VAS score for leg pain showed a similar reduction from 7.20 to 1.76 over the same period. These findings align with previous literature indicating that minimally invasive surgical techniques can effectively alleviate pain in patients suffering from lumbar spinal stenosis.10–13
The ODI reflected a marked improvement, with scores decreasing from 76.35 preoperatively to 10.34 at the 6-month follow-up. This substantial reduction underscores the impact of surgical intervention on functional status and quality of life for patients. In agreement with these findings, Kim et al. (2021)12 reported a significant improvement in ODI scores from 58.9 to 28 at their one-year follow-up, reinforcing the notion that endoscopic decompression contributes positively to patient functionality. Additionally, Xue et al. (2021)13 noted a comparable improvement in ODI scores, which decreased from 72.35 to 16.15, further supporting the findings of our study.
Moreover, the Mac-Nab criteria indicated excellent outcomes in 20 patients (80%), good outcomes in 4 patients (16%), and fair outcomes in 1 patient (4%) at the 6-month follow-up. This level of success mirrors the findings of other studies,14 which reported similar Mac-Nab criteria outcomes, demonstrating that a significant proportion of patients achieved either good or excellent results following endoscopic decompression.
Radiologically, our study observed a significant increase in the canal cross-sectional area, which improved from 75.78 mm² preoperatively to 155.2 mm² postoperatively. This is consistent with findings from previous studies,10,15 which also reported substantial increases in canal cross-sectional area following decompression surgeries, emphasizing the efficacy of the surgical intervention in alleviating spinal canal obstruction.
The >100% expansion in canal dimensions directly correlates with our clinical outcomes, as the achieved 155.2 mm² far exceeds the 100-130 mm² threshold considered necessary for symptomatic relief in lumbar stenosis. Importantly, the preserved facet joint dimensions (pre-op: 14.8±0.9mm vs post-op: 14.4±0.7mm, p>0.05) demonstrate our technique’s ability to maintain spinal stability while achieving adequate decompression, a distinct advantage over conventional laminectomy where facet integrity is often compromised.
Overall, these results corroborate the existing literature, including systematic reviews and meta-analyses, that advocate for the safety and effectiveness of minimally invasive techniques in managing lumbar spinal stenosis. The consistency of our findings with previous studies reinforces the validity of our results and highlights the potential benefits of full-endoscopic decompression for improving both pain relief and functional outcomes in patients with lumbar spinal stenosis.
The findings from our study carry significant implications for clinical practice concerning the surgical management of lumbar spinal stenosis. The marked improvements in VAS and ODI scores post-surgery demonstrate that full-endoscopic decompression can effectively alleviate pain and enhance functional abilities in patients suffering from this condition. As healthcare providers increasingly adopt minimally invasive techniques, the evidence supporting their effectiveness can guide surgical decision-making, leading to more informed choices regarding patient treatment options. Notably, the substantial reduction in VAS scores for back and leg pain indicates the potential of this technique to provide rapid pain relief, aligning with similar outcomes documented in the literature. Furthermore, the improvement in ODI scores from 76.35 to 10.34 at the six-month follow-up suggests that patients not only experience less pain but also achieve a notable enhancement in their functional status, corroborating previous findings that emphasize effective surgical intervention translating into better patient-reported outcomes.
Moreover, the high rate of favorable outcomes, as indicated by the Mac-Nab criteria, further emphasizes the reliability of this surgical technique, with 80% of patients reporting excellent outcomes. This evidence can influence clinical practice by promoting minimally invasive surgery as a first-line option for managing lumbar spinal stenosis, offering a safer alternative to more invasive procedures that may carry higher risks. The significant increase in canal cross-sectional area observed in our study correlates with improved clinical outcomes, reaffirming the necessity of addressing the anatomical issues underlying lumbar spinal stenosis. As noted by Xue et al. (2021),13 effective decompression alleviates symptoms while addressing the root cause of spinal canal obstruction. Ultimately, the results of our study provide strong evidence for the clinical effectiveness of full-endoscopic decompression, underscoring its role as a safe and effective treatment option that enhances patient quality of life and recovery outcomes while informing surgical decision-making in clinical practice.
Our study’s findings on the significant improvement in VAS scores, ODI scores, and Mac-Nab criteria align with the results from Kim et al. (2021),12 which reported substantial reductions in VAS scores for back and leg pain following endoscopic decompression, with VAS back scores improving from 5.4 preoperatively to 1.6 at one-year follow-up. Similarly, Xue et al. (2021) demonstrated notable improvements in both VAS and ODI scores, with a mean ODI reduction from 72.35 preoperatively to 16.15 at the last follow-up. These results underscore the efficacy of endoscopic techniques in alleviating pain and enhancing function for patients suffering from lumbar spinal stenosis. However, our findings also reveal unique aspects. For instance, while both Kim et al. and Xue et al. reported improvements in the cross-sectional area of the spinal canal, our study demonstrated a more pronounced increase postoperatively, indicating potential differences in surgical techniques or patient populations.12,13 Furthermore, the higher proportion of patients achieving excellent outcomes according to the Mac-Nab criteria in our cohort suggests that the full-endoscopic approach may yield superior functional results compared to other methods. Discrepancies in reported complication rates, including our zero complication incidence versus minor complications noted in other studies, may reflect differences in surgical expertise, patient selection criteria, or postoperative care protocols.
The observed improvements in pain and disability scores following full-endoscopic decompression for lumbar spinal stenosis can be attributed to several mechanisms associated with the endoscopic approach. One significant factor is the minimally invasive nature of the technique, which typically results in reduced soft tissue disruption compared to traditional open surgery. This preservation of surrounding tissues, including muscle and ligament structures, likely contributes to quicker recovery times and less postoperative pain. Available evidence supports this, indicating that minimally invasive surgical techniques lead to decreased inflammatory responses and quicker healing due to less tissue trauma. Additionally, the endoscopic approach allows for precise decompression of affected nerve roots and the spinal canal while maintaining the integrity of adjacent anatomical structures. The direct visualization provided by endoscopic techniques enhances the surgeon’s ability to accurately identify and address pathological changes, such as hypertrophied ligaments or herniated discs, without extensive manipulation of surrounding tissues. This specificity in targeting the source of compression may explain the significant improvements in VAS and ODI scores observed in our study.
Another mechanism to consider is the role of neural decompression in pain relief. By relieving pressure on the affected nerves, the endoscopic technique may reduce neurogenic pain, often exacerbated by chronic compression. As previously highlighted,16 effective decompression not only alleviates symptoms but also promotes neuroplastic changes that contribute to long-term pain relief and functional recovery. Furthermore, the rapid return to daily activities following endoscopic decompression, as observed in our study with an average time to return to work of 6.05 weeks, emphasizes how this technique enhances patient quality of life by facilitating quicker engagement in rehabilitation and normal activities, thereby fostering overall recovery. In summary, the mechanisms underlying the improvements in pain and disability scores following endoscopic decompression are multifactorial, involving minimized tissue trauma, targeted decompression, and potential neuroplasticity enhancements that collectively contribute to superior clinical outcomes.
This study has several limitations that must be acknowledged, which may impact the interpretation of our findings. First, the retrospective design of our research, coupled with the fact that it was conducted at a single center, restricts the generalizability of the results. This design can introduce selection bias, limiting the applicability of our conclusions to the wider population of patients with lumbar spinal stenosis. Second, the relatively small sample size restricts the statistical power of the analysis. As a result, certain clinical parameters and outcomes may not have been adequately assessed, potentially skewing the understanding of the efficacy of full-endoscopic decompression in this patient population. These limitations suggest that caution should be exercised when interpreting the data and drawing conclusions about the broader applicability of our findings. Future studies should consider multi-center designs with larger sample sizes to enhance the robustness of the data and facilitate more comprehensive analyses of long-term outcomes. Furthermore, a prospective approach could better control for confounding variables and provide a clearer understanding of the relationship between surgical interventions and patient outcomes.
5. Conclusions
The results of our study indicate that full-endoscopic decompression for lumbar canal stenosis can yield excellent outcomes. The advancements in endoscopic surgical instruments and techniques enable these procedures to be performed with comparable, if not superior, effectiveness to traditional open decompression surgery. Given the associated benefits, such as reduced tissue trauma, shorter recovery times, and decreased hospitalization, full-endoscopic decompression represents a promising approach for managing lumbar spinal stenosis. Future research should focus on long-term outcomes and comparisons with other minimally invasive techniques to further validate these findings and optimize patient care.
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conceptualization: DTT, DNS. Methodology: DTT, DNS. Software: DAT, VHL. Validation: DTT, DNS. Formal analysis: DTT, DAT, VHL. Investigation: DTT, DNS, LTD, DAT, VHL. Resources: DTT, DNS. Data curation: DTT, DNS. Writing—original draft preparation: DAT, VHL. Writing—review and editing: DTT, DNS. Visualization: DTT, DNS. Supervision: DTT, DNS. Project administration: DTT. All authors have read and agreed to the submitted version of the manuscript.
Fundings
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of the Hanoi Medical University.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability
The data used in this article are available upon request from the corresponding author. The data are not publicly available due to the protection of personal data.
Acknowledgments
We extend our sincere gratitude to the study participants and their families for their invaluable assistance. Additionally, we would like to express our gratitude to the Board of Directors of Viet Duc University Hospital, and Department of Surgery of Hanoi Medical University, for their support in completing this study.
Corresponding author
Associate Professor, Ph.D, MD Dinh Ngoc Son
Senior Lecturer of Department of Surgery, Hanoi Medical University, Hanoi, Vietnam
Head of Spine Surgery Department, Viet Duc University Hospital, Hanoi, Vietnam
Email: dinhngocson@hmu.edu.vn or Bsdinhngocson@gmail.com