Introduction
The rotator cuff plays a vital role in shoulder stability and movement. Massive rotator cuff tears (MRCTs), defined as tears involving two or more tendons or exceeding 5 cm in size, present a significant challenge.1–4 These extensive tears often resist repair using traditional techniques and have high rates of retearing, limiting treatment options for patients.5,6
For smaller rotator cuff tears, arthroscopic or open surgical repair remains the gold standard treatment, aiming to reattach the torn tendon to the bone.7–9 However, for MRCTs deemed irreparable, alternative approaches are necessary. Tendon transfer surgery has emerged as a promising option in these cases.5,6,10 The latissimus dorsi muscle transfer is currently the most widely used tendon transfer procedure for MRCTs, attempting to restore function by transferring a healthy tendon to substitute for the damaged rotator cuff.11–13
The lower trapezius muscle, located on the back beneath the shoulder blade, plays a crucial role in shoulder depression and rotation. Due to its anatomical location and potential to generate external rotation force, the lower trapezius has emerged as a promising candidate for tendon transfer surgery in patients with MRCTs.14–16 Lower trapezius transfer (LTT) is a developing surgical technique that utilizes the lower trapezius tendon to functionally replace the damaged rotator cuff tendons. This approach aims to restore external rotation and improve overall shoulder function in patients with irreparable tears.
Despite the promise that LTT holds for treating MRCTs, the current body of evidence on its outcomes remains limited. Existing research primarily consists of small, isolated studies, often focusing on short-term follow-up. This scarcity of high-quality data makes it challenging to definitively assess the long-term effectiveness of LTT for pain reduction, functional improvement, and complication rates. A systematic review is therefore crucial to synthesize the available research on LTT for MRCTs.
This systematic review aims to comprehensively evaluate the current evidence on the outcomes of LTT for the treatment of MRCTs. Our primary objective is to assess the functional outcomes achieved with LTT, particularly using Achilles allografts, focusing on key areas such as pain reduction, range of motion improvement, and regained strength in the affected shoulder. By analyzing patient-reported outcome scores and objective measures of function, we aim to understand the effectiveness of LTT in restoring shoulder function in patients with MRCTs. Additionally, this review will evaluate the complication rates associated with LTT surgery. This includes investigating the incidence of surgical site infections, nerve injuries, and any other potential complications that may arise during or after the procedure.
Methods
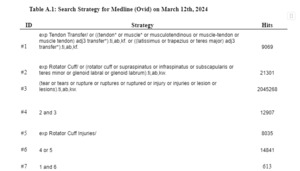
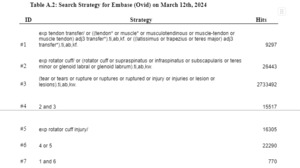
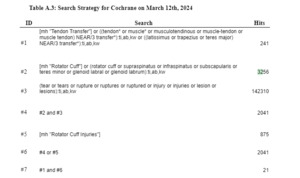
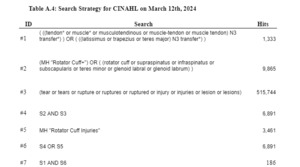
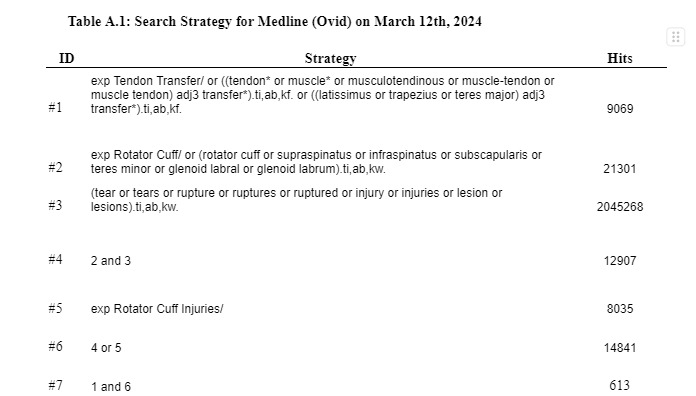
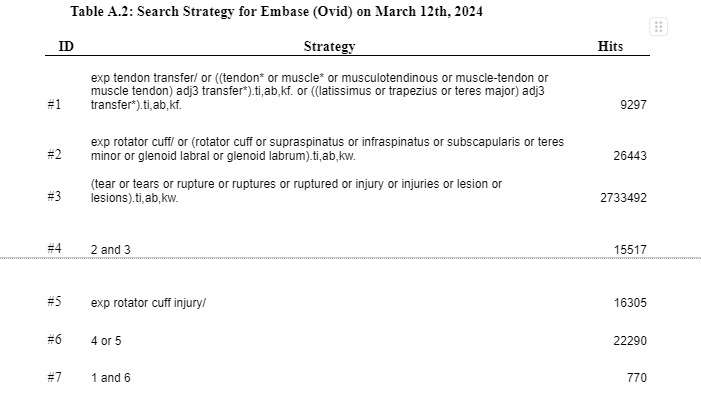
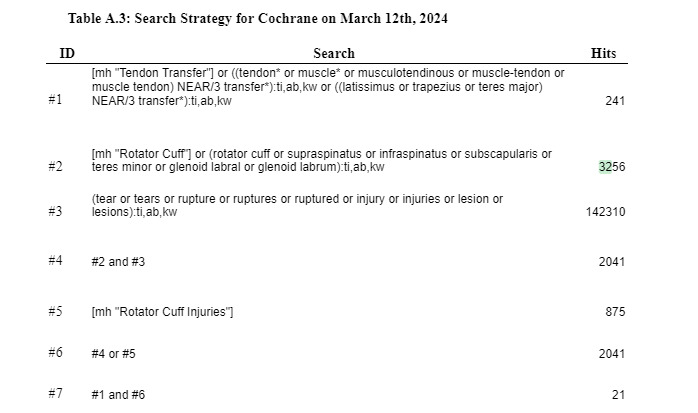
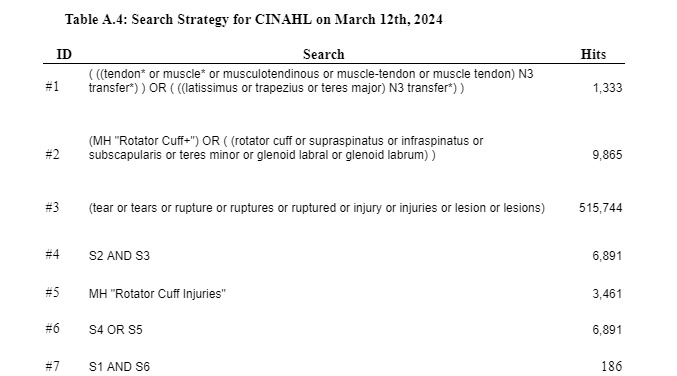
This systematic review involved a search of Medline (Ovid), Cochrane, and Embase that was conducted from the inception of the databases to March 2024. The study followed PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for self-reporting. The study was registered on Prospero (CRD42024520286). A research librarian conducted a search on the aforementioned databases using relevant keywords and mesh terms (Appendix A). Keywords and concepts included: ‘massive rotator cuff tear’, ‘irreparable rotator cuff tear’, ‘posterior-superior rotator cuff tear’, ‘lower trapezius transfer’, ‘management of massive irreparable rotator cuff tear’, ‘tendon transfer’, ‘outcomes’, ‘patient-reported outcomes’, ‘long-term outcomes’, ‘return to activity’, and ‘complications’. References were uploaded into Covidence () for screening according to eligibility criteria.
Eligibility Criteria and Study Selection
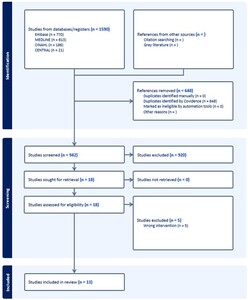
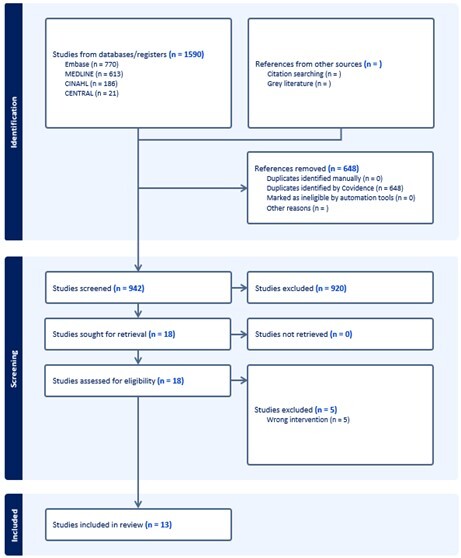
Abstracts and titles were screened initially (Figure 1). Two blinded reviewers (S.R.V and K.S) included studies in English that reported on trapezius tendon transfer for massive irreparable rotator cuff tears. Eligible study designs included case reports, case series, retrospective cohort studies, and randomized controlled trials. Exclusion criteria comprised studies that did not directly investigate trapezius tendon transfer, non-English studies, reviews, non-human studies, and cadaveric studies. A second full-text review was performed on the remaining papers based on the same criteria to exclude additional studies. A third author (C.N) resolved any conflicts between reviewers if necessary.
Data Extraction
Two authors (S.R.V and K.S) independently extracted data points. The opposite reviewer then performed a second review, with any discrepancies being resolved by the senior author (C.N). Data points included the following: study type, level of evidence, number of patients, sex, mean age, injury mechanism, associated injuries/comorbidities, surgical indication and techniques, complications, follow-up duration, secondary surgeries, return to activity measurements, postoperative management, and outcome scores.
Methodological Quality Assessment / Risk of Bias
The JBI protocol checklist (https://jbi.global/critical-appraisal-tools) for cohort studies, case series, and case reports was utilized to evaluate the methodological quality of included studies to analyze the validity of methods, appropriateness of analysis, and quality of presentation for their given study type.
Statistical Analysis
Meta-analysis was not performed. Categorical variables were summarized and presented as counts or proportions, while continuous variables were presented as means. Outcomes of interest were aggregated and reported in tables highlighting individual studies and their findings. The research team reported findings from data synthesis as tables and figures. A meta-analysis was not performed, and individual participant data was not collected.
Ethical Considerations
This data is publicly available and contains no patient information. This study has been performed in accordance with the ethical standards in the 1964 Declaration of Helsinki and has been carried out in accordance with relevant regulations of the US Health Insurance Portability and Accountability Act (HIPAA). IRB approval was not required.
Results
Literature Search and Screening
The initial search of the databases yielded a total of 1,590 studies (770 from Embase, 613 from MEDLINE, 186 from CINAHL, and 21 from CENTRAL). After removing 648 duplicates identified by Covidence, 942 studies remained for screening. Titles and abstracts were screened, resulting in 18 studies that met the initial review criteria for inclusion. After full-text screening, 5 studies were excluded due to the wrong intervention, leaving 13 studies for data extraction. Another 4 studies were subsequently manually removed due to not having full manuscripts available for analysis, ultimately resulting in the analysis of 9 studies. Data extraction was performed on these 9 studies, which included 7 case series, 1 case report with Level V evidence and 1 retrospective cohort study with Level III evidence.17–24 All results were reported per the PRISMA reporting standards.25
Methodological Quality Assessment
Two reviewers (S.R.V, K.S) analyzed studies according to JBI Clinical Appraisal tools for each study type. 7 case series had a mean score of 8.1 out of 10, 1 case report had a score of 7 out of 8, and 1 retrospective cohort study had a score of 8 out of 10. All 9 studies were determined to have adequate methodology to be included in the review.
Patient Demographics
All nine studies focused on patients with various injuries and included a total of 214 cases of trapezius tendon transfer surgeries (Table 1). The patient cohort consisted of 161 males and 53 females with a weighted average age of 57.7 years (range 31-73 years). The injury mechanisms varied, including incidents such as slipping on ice, falling from stairs, car accidents, motorcycle accidents, sports injuries, repetitive heavy lifting, onset of injury at work, and direct trauma to the shoulder.
Surgical Indications, Techniques, and Implants
In the reviewed studies, surgical indications for trapezius tendon transfer were comprehensively reported, reflecting a wide range of clinical scenarios. All nine studies also utilized MRI evidence of a tear as a surgical indication, confirming the presence of massive irreparable rotator cuff tears. Other common indications included failed conservative treatment and high-grade fatty infiltration, reported in multiple studies. Additionally, limited range of motion, shoulder weakness, and the presence of arthritic changes were also noted as crucial factors prompting surgical intervention. These indications collectively emphasize the critical condition of the patients selected for trapezius tendon transfer, who typically present with severe and functionally debilitating shoulder pathology.
The operation types and surgical techniques varied across the studies, reflecting advancements and preferences in surgical practice. Three studies reported using both open and arthroscopic methods, allowing for flexibility based on patient-specific factors and surgeon expertise. Open surgery was described in detail, including patient positioning and specific techniques to expose the rotator cuff and perform the lower trapezius transfer. For instance, the patient was often positioned laterally, and meticulous steps were taken to prepare the surgical site, ensuring optimal exposure and graft placement.
The predominant technique reported was the lower trapezius transfer, mentioned in eight studies. This technique involves the transfer of the lower trapezius muscle to compensate for the deficient rotator cuff, utilizing its anatomical and functional advantages. The type of graft used for this procedure was predominantly Achilles allograft, utilized in eight studies. The Achilles tendon graft may be favored for its strength and compatibility, providing a robust scaffold for the transferred trapezius muscle. One study reported the use of a hamstring allograft, highlighting an alternative graft option that may be selected based on specific patient needs or surgeon preference.
Reoperations and Surgical Complications
Surgical complications and the necessity for reoperations were critical aspects addressed in the reviewed studies, reflecting the inherent challenges and complexities associated with trapezius tendon transfer surgeries. Complications were reported in eight of the nine studies, underscoring the importance of caution and comprehensive postoperative care in managing these high-risk patients. The retear rate was determined to be 7.5% and infection rate was 2.3%, these were determined to be the most common surgical complications. Seromas were only noted in 3 patients. The most frequently cited orthopedic complication was hardware failure, which necessitated additional surgical interventions in several cases. For instance, infections were a notable concern, with one patient requiring debridement followed by shoulder fusion due to persistent infection-related complications. This case exemplifies the potential severity of postoperative infections and the need for prompt and effective management strategies.
In terms of reoperations, six studies documented secondary surgical procedures, affecting a total of 10 patients, which constituted 4.67% of the overall patient cohort. These reoperations were performed for a variety of reasons, including hardware failures, persistent pain, and failure of the initial tendon transfer to provide the desired functional improvement. For example, three patients underwent conversion to reverse shoulder arthroplasty due to inadequate clinical improvement following the initial trapezius tendon transfer.
Moreover, the studies provided detailed accounts of other surgical complications beyond hardware failures and infections. Early postoperative complications included seroma formation in three shoulders, a superficial infection in one shoulder, hand numbness in four shoulders, and traumatic rupture of the transferred tendon in two shoulders. These complications required varied management approaches, from conservative treatments to additional surgical interventions.
The reported complications also extended to graft-related issues, with several studies highlighting the occurrence of retears in the transferred tendon. For instance, one study reported a 19.4% retear rate of the Achilles tendon allograft, predominantly at the medial aspect of the supraspinatus footprint.
The follow-up duration across the studies varied, with an average of approximately 38.4 months, providing a substantial period for monitoring and assessing long-term complications and reoperations. This extended follow-up is crucial for understanding the durability and effectiveness of trapezius tendon transfers, as it allows for the identification of late complications and the assessment of sustained functional improvements.
Return to activity and Postoperative Management
The return to activity (RTS) outcomes following trapezius tendon transfer surgeries were documented across multiple studies. Of the studies included in this review, several highlighted successful return to unrestricted activities postoperatively. Patients were generally allowed to resume their previous levels of activity after a comprehensive rehabilitation period, which included the use of braces or splints and a structured physiotherapy regimen.
In one study, patients were permitted to return to unrestricted activities after 6 months, following the use of a custom-made shoulder spica brace for 8 weeks and subsequent active-assisted range of motion exercises. Another study reported that of 36 patients, 30 (83.3%) were able to resume their previous work, with the Single Assessment Numeric Evaluation (SANE) score averaging 8.7 ± 1.2, indicating prominent levels of patient satisfaction and functional recovery. Similarly, another cohort showed that 7 out of 15 patients (50%) returned to full duty, while 4 patients (28.6%) returned to modified duty, and 3 patients (21.4%) were unable to return to work.
Furthermore, specific postoperative protocols were outlined, such as immobilization in an abduction brace for a defined period, followed by gradual progression through passive and active-assisted motion exercises, leading to full range-of-motion and strengthening exercises. These protocols were crucial in achieving optimal outcomes and enabling patients to return to their pre-injury levels of activity.
Overall, the reviewed studies demonstrate that with proper surgical technique and rigorous postoperative care, a considerable proportion of patients undergoing trapezius tendon transfer for massive irreparable rotator cuff tears can expect to return to their previous activities and experience improvements in shoulder function.
Discussion
Massive rotator cuff tears, often defined by involvement of 2+ tendons or tears of 5 cm or larger, can be treated using a variety of techniques, ranging from biceps incorporating techniques to trapezius transfers.16,26–29 These tears are also often associated with advanced fatty infiltration of the muscles.30–32 Our review of 9 studies yielded 214 patients with 184 patients having undergone lower trapezius transfers using lower trapezius allografts and 20 patients with superior trapezius transfers using hamstring allografts. The primary objective of this systematic review was to evaluate the efficacy of trapezius transfer, primarily using Achilles allografts, in managing massive irreparable rotator cuff tears. The results indicate a promising alternative for patients with massive irreparable rotator cuff tears, particularly when compared to other tendon transfer techniques. The use of Achilles allograft in trapezius transfer appears to provide substantial improvements in pain and functional outcomes. The average follow-up period of 38.4 months provides a robust basis for assessing the long-term efficacy of the procedure.
Complications and Reoperations
Despite the promising outcomes of trapezius transfer, it is essential to acknowledge and address the complications associated with this procedure. Complications were reported in eight of the nine studies reviewed, underscoring the complexity and risks involved in managing massive irreparable rotator cuff tears through tendon transfer surgeries.
The most frequently observed complication was hardware failure, which required additional surgical interventions in several cases. Hardware failures can significantly impact patient recovery, often necessitating reoperations to replace or adjust the failed components. Infections were another notable concern, with an incidence rate of 2.3%. For instance, one patient required debridement followed by shoulder fusion due to persistent infection-related complications, highlighting the potential severity of postoperative infections and the necessity for prompt and effective management strategies.
Other early postoperative complications included seroma formation in three shoulders, a superficial infection in one shoulder, hand numbness in four shoulders, and traumatic rupture of the transferred tendon in two shoulders. These complications required varied management approaches, from conservative treatments to additional surgical interventions. The reported complications also extended to graft-related issues, with several studies highlighting the occurrence of retears in the transferred tendon. The retear rate of 7.5% is a notable finding that requires attention. For example, one study reported a 19.4% retear rate of the Achilles tendon allograft, at the medial aspect of the supraspinatus footprint. Due to the lack of studies detailing complications and reoperations there have not been many consistent reports of types of complications following a lower trapezius transfer.33 However, some case-reports, case-series, and reviews report findings that are similar to our own. Marinis et al, notes, in their review, a contrasting and much higher complication rate of 17.6% but similar to our own study reports seromas/hematomas as being common complications along with conversion to shoulder arthroplasty as being the most common reoperation.34,35
Comparison of Achilles Allograft with Latissimus Dorsi Transfer
The comparison between trapezius transfer and latissimus dorsi transfer is critical in understanding the landscape of surgical options available for managing massive irreparable rotator cuff tears. Latissimus dorsi transfer, a more traditional and widely adopted technique, has historically been the preferred choice due to its capacity to restore anterior and internal rotation.36,37 However, the emergence of the trapezius transfer, especially with the use of Achilles allografts, presents a compelling alternative that might be more anatomically and functionally suited for certain patients.22,38,39
While both techniques aim to improve shoulder function by compensating for the deficient rotator cuff, they differ in their biomechanical implications and the specific aspects of shoulder motion they address. The trapezius transfer with Achilles allograft is particularly beneficial for enhancing external rotation and overall shoulder stability, leveraging the unique line of pull and strength of the lower trapezius muscle.38 In contrast, the latissimus dorsi transfer primarily supports internal rotation and adduction, which can be more beneficial in patients whose daily activities or occupational demands require these specific movements.37
Studies comparing these techniques directly are limited, but existing literature suggests that the choice of technique should be tailored to the patient’s specific deficits and functional demands. For instance, trapezius transfer might be more advantageous in patients with significant external rotation deficits, where the posterior force vector of the lower trapezius can be maximally utilized. Additionally, the use of Achilles allograft in trapezius transfers has shown promising results in terms of graft durability and integration, potentially offering a more robust reconstruction with fewer complications such as graft failure or retear, which are occasionally observed with latissimus dorsi transfers.38,39
Postoperative Rehabilitation
Specific postoperative rehabilitation protocol is essential following the trapezius transfer surgery for massive irreparable rotator cuff tears. Studies show slight variances in rehabilitation protocol with the majority incorporating immobilization with an induction brace followed by progressive passive and active-assisted motion exercises and ending with strengthening exercises.22,40 Typically active-assisted range of motion exercises began after 6-8 weeks of immobilization and unrestricted activity was allowed 6 months postoperatively. The progressive increase of mobilization and strengthening is crucial in allowing patients to regain full range of motion and return to work and recreational activities.
Patient Selection and Surgical Techniques
Currently, surgical indications for trapezius transfer are loosely based on failed conservative treatment or MRI-confirmation.6,38,41 Overall, patients that received surgery were included due to demonstrably severe pathology. Given the variability of surgical indications in the selected studies, it may be beneficial for patient outcomes to standardize surgical indication factors. Based on the studies presented in this review, indications should include MRI-confirmed massive irreparable rotator cuff tears, failed conservative treatment, and significant functional limitations which may include fatty infiltration, limited range of motion, or weakness. By focusing on patients who meet these specific criteria, surgeons can potentially optimize the benefits of trapezius transfer for patients suffering massive irreparable rotator cuff tears.
The studies in this review included a variety of operative approaches, due to both surgical advancements and individual surgeon discretion.14,42,43 Despite the variations in surgical approach, patient outcomes in the studies included in this review appear to have similar outcomes. The variation in surgical technique may highlight the need for further standardization within the surgical community to optimize the outcomes for trapezius transfer. Standardizing key aspects such as surgical approach, patient positioning, and graft selection of Achilles versus hamstring would facilitate a more controlled surgical environment, potentially minimizing variability and maximizing functional benefits. It should be recognized that flexibility in surgical approach and technique is beneficial to adapt to patient factors and surgeon learning-curve. While the Achilles allograft may offer superior strength and compatibility, the hamstring allograft still may be the optimal technique for specific cases.
Long-Term Outcomes and Follow-up
The current review adds to the growing body of evidence supporting the use of trapezius transfer for the management of massive irreparable rotator cuff tears. While the average follow-up of 38.4 months in the included studies provides valuable analysis into the efficacy of this procedure, longer follow-up periods are necessary for an understanding of durability and long-term efficacy. Continual monitoring of patients undergoing trapezius transfer is crucial to identify any potential late-onset complications and to ensure sustained functional improvements.
Limitation
We acknowledge a number of study limitations. The evidence in this review comes primarily from case series and a single retrospective cohort study, which are observational designs and inherently less robust than randomized controlled trials. This prevents establishing a definitive cause-and-effect relationship between the trapezius tendon transfer surgery and patient outcomes. The heterogeneity in surgical techniques and postoperative protocols makes it difficult to definitively determine the most optimal approach for trapezius tendon transfer surgery. The generalizability of the findings may be limited. The studies included a relatively small patient sample size (214 patients) and focused on patients with severe shoulder pathology. The results may not be applicable to other patient populations with less extensive rotator cuff tears or different underlying conditions. The follow-up duration across studies varied, with an average of 38.4 months. While this provides a reasonable timeframe, longer follow-up periods would be ideal to capture potential late-term complications and ensure the sustainability of functional improvements.
Conclusion
This systematic review demonstrates the promise of lower trapezius tendon transfer with Achilles allograft for regaining function in patients with massive irreparable rotator cuff tears. The procedure offers significant improvements in pain, mobility, and overall function, with a high percentage of patients returning to their prior activities. While a modest complication rate exists, the overall benefits outweigh the risks. This study adds to the growing body of evidence supporting trapezius transfer as a valuable tool for shoulder surgeons managing these challenging cases. Further research should aim to standardize surgical techniques and post-operative protocols to refine the procedure and potentially improve outcomes even further.
Author Contributions
Suhas Rao Velichala: Writing – review & editing, Writing – original draft, Methodology, Investigation, Formal analysis. Kush Savsani: Writing – review & editing, Writing – original draft, Methodology, Data curation, Conceptualization. Chase Nelson: Writing – review & editing, Data curation, Conceptualization. Matthew Smith: Writing – review & editing, Formal analysis, Conceptualization. James Satalich: Writing – review & editing, Supervision, Conceptualization. Conor O’Neill : Writing – review & editing, Supervision, Conceptualization. Jennifer Vanderbeck: Writing – review & editing, Supervision. Douglas Boardman: Writing – review & editing, Supervision.
Conflicts of interest
No Relevant Disclosures or Potential Conflicts of Interest
Funding
No Funding to Report