Introduction
Since its introduction in 1960s, total hip arthroplasty (THA) earned the title of the gold standard treatment for endstage hip osteoarthritis either primary or secondary.1,2 Due to the high success rates and the excellent functional results, THA has even been referred to as “the operation of the century”.3 Therefore, the demand for THA is increasing exponentially, with a projected increase of 176% by 2040.4 Albeit the evolution of prosthesis’ designs and materials, revision-THA (R-THA) remains a major concern with an incidence of 11% whereas a growth of 42% by 2040 is also expected.4,5 R-THA is a very demanding procedure, especially when the acetabular component needs to be revised, which in 58% of all cases is the prevailing scenario.5 The main causes for isolated acetabular revision are instability (33%), aseptic loosening (24.2%), implant failure (10%), periprosthetic osteolysis (8%), wear of the bearing surfaces (8%), infection (5%) and peri-prosthetic fractures (1.8%). The main challenge, when revising an acetabular cup, is the proper management of the consequent bone loss.6
Regarding the acetabular bone defects, various classification systems have been proposed in order to adequately guide the treatment strategy. Paprosky classification is the most commonly utilized, that also showcases great reliability and validity.7 It focuses on four aspects; the degree of migration of the hip center of rotation in relation to the superior obturator line, the extent of teardrop and ischial osteolysis and the ilioischial line’s (Kohler’s line) integrity. In acetabular bone deficiencies classified as Paprosky 1, 2A and 2B, a cementless or a cemented cup with or without impaction grafting is usually sufficient for the appropriate management.8 However, in more severe acetabular bone losses (Paprosky 2C-3B) the therapeutic strategies are more complex and demanding. For these cases, various treatment options are available. Reinforcement devices, such as reinforcement rings and antiprotrusio cages, were traditionally implemented.9 Nevertheless, due to their high complication and revision rates, with a mean of 29.2% and 8.2% respectively, and since they do not offer a biological fixation, their popularity is slowly decreasing.10,11 Porous-coated custom-made triflange acetabular components is another treatment option that offers a more biological approach but their limited availability, high cost and the fact that they do not achieve superior results make their adoption controversial.10,11
Recently, trabecular metal systems have also been utilized in such challenging cases. These systems are comprised of a highly porous-coated acetabular component, supplemented by trabecular metal augments, hence promoting substantial bone ingrowth. From the existing literature, they demonstrate encouraging short-term and mid-term results, with a mean of 97.2% survival rate, but their long-term results are still lacking.8,11,12 Based on these promising preliminary results, a new acetabular revision system, manufactured using trabecular titanium (TT), has been recently introduced, aiming for even more superior outcomes comparing to other implants. The Delta Revision TT system (LimaCorporate, Villanova di San Daniele del Friuli, Italy) incorporates a cup-cage design combining the characteristics of a cementless multihole cup that also possesses a caudal hook and three superior iliac flanges. To date, there is only a limited number of studies examining the efficacy of this new cup-cage construct. Although, the initial reports seem optimistic, the available evidence is still scarce and more research is necessary.13,14 In the present study we aim to present the clinical outcomes, the survival and complication rates as well as the osseointegration of the impacted morselized allograft in a cohort of patients in which this new cup-cage construct was implanted.
Patients and Methods
This is a retrospective study with prospectively collected data. The study included subjects with isolated aseptic loosening of the acetabular component and acetabular bone defects that were classified as 2B to 3B according to the Paprosky classification. Subjects were excluded from the study if they had less than one year of follow-up, underwent revision surgery for reasons other than aseptic loosening and those who presented with defects classified as 1, 2A or Pelvic Discontinuity. Demographic data, ASA score alongside complications were meticulously collected. Functional outcomes were assessed using Harris-Hip score, HOOS-JR score, Forgotten Joint Score and VAS score. Three main radiological outcomes were evaluated in the current study˙ the osseointegration of the allograft according to the Oswestry classification and the occurrence of heterotopic ossification which was assessed using the Brooker’s classification. Patient-reported outcome measures (PROMs) were quantitatively measured utilizing the EQ-5D-5L score to assess the patient’s health status and quality of life post-intervention. Statistical analysis of the data was conducted utilizing the SPSS version 23.0 statistical program (SPSS Inc., Chicago, IL, USA).
Surgical Technique & Postoperative Protocol
All revision procedures were performed by one senior surgeon (G.D.) who is an expert in major joint reconstruction surgeries. A modified Hardinge’s approach was performed in all patients. After the removal of the acetabular components, the soft tissue membranes and the cement, in cases where a cemented cup had been implanted previously, the acetabular bone bed was reamed with progressively larger reamers until sufficient bleeding was evident from the remaining host bone. All bone losses were managed exclusively with fresh-frozen femoral heads. The articular cartilage was removed from the femoral heads which were subsequently cut into bone chips of 1cm size using a rongeur. The bone chips were meticulously cleaned with warm saline solution from fatty tissue and other debris and packed into the defects that were prepared and cleaned from blood clots, fatty tissue and debris. In the existing literature, it has been shown that washing of the bone grafts before impaction leads to increased friction, allows for tighter impaction and reduces the risk of infection.15,16 Rinsing of the bone grafts does not influence negatively their incorporation but it actually causes the opposite effect.17,18 It must be highlighted that washing of the grafts after impaction does not alter bone ingrowth.18
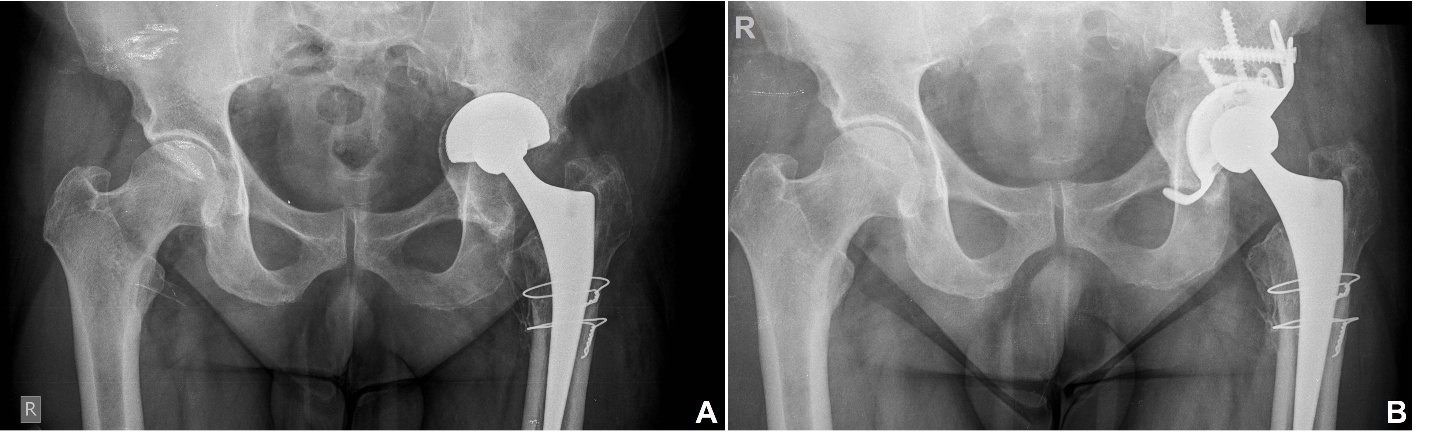
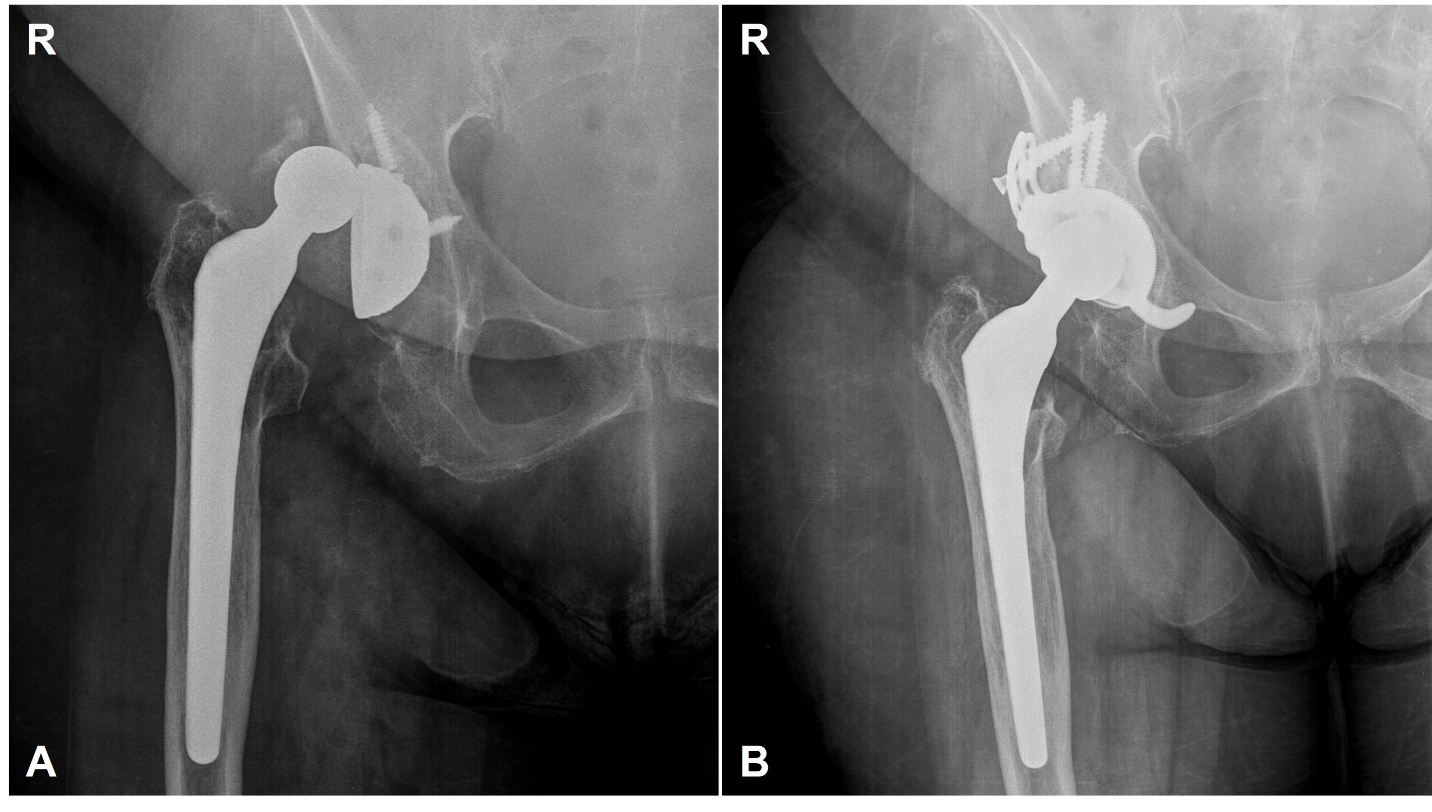
The defects were packed with morselized allografts, followed by firm impaction using various impactors and a hammer. In any case no reverse reaming was performed since it has been shown that it is inadequate in terms of impaction force and primary cup stability.17,19 The appropriate size of the cup-cage construct was chosen afterwards and a final reduction was performed. Before the implantation of the final components, an intraoperative fluoroscopic image was obtained in order to confirm the correct size and position-orientation of the construct. The ischial hook was placed at the obturator foramen and the iliac flanges were adjusted accordingly to the iliac bone and stabilized with minimum five screws.
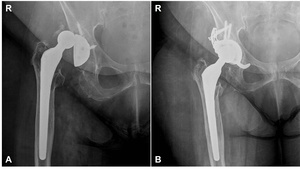
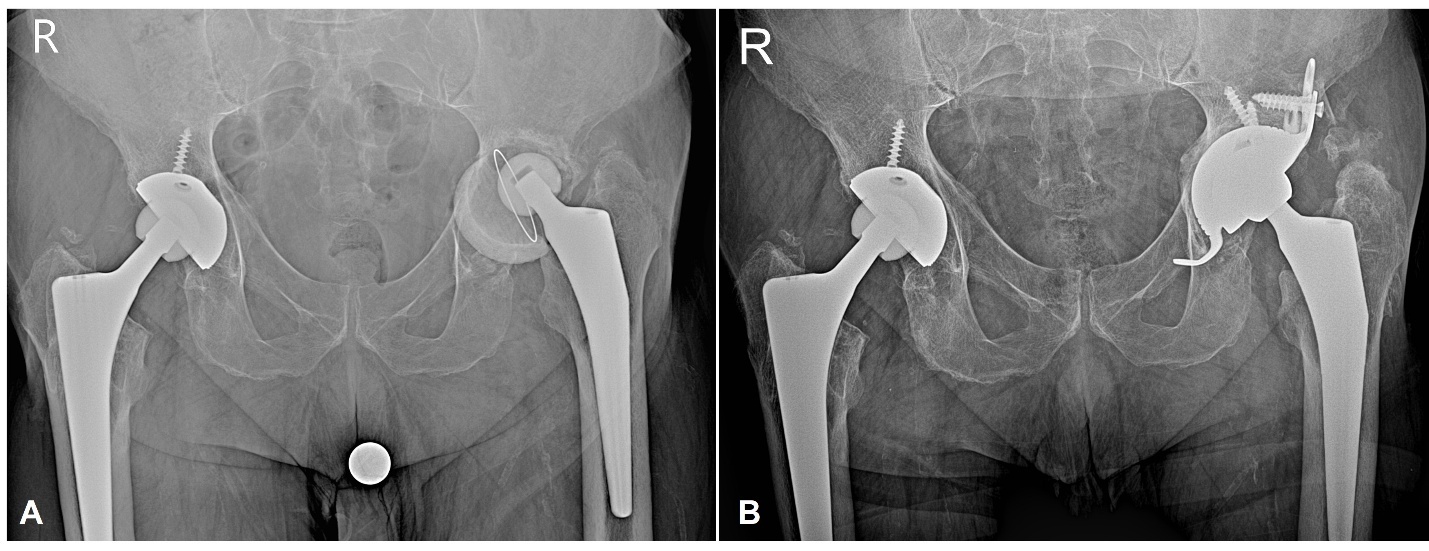
Patients were instructed to walk with toe-touch weight-bearing the first 6 weeks and gradually increase their weightbearing status thereafter. At 3 months after surgery, they were instructed to walk without any support. Clinical as well as radiological evaluations were performed at 6 weeks, 3, 6, 12 months and yearly thereafter (Figures 1-3).
Results
The study included 11 patients (8 males – 72.7%, 3 females – 27.3%) with a mean age of 67.9 years (±8.9 years) and a mean follow-up of 54.64 months (±23.07 months). The patients were grouped into four categories according to their acetabular bone defect using the Paprosky classification (2B-3B). Additionally, a logistic regression analysis was performed which evaluated the effects of variables sex, age and ASA score (American Society of Anesthesiologists score) on the outcomes. None of the variables had statistically significant effects (p-value=0.6) (Table 1). The patients’ demographic characteristics, acetabular bone defects, complications as wells as radiological outcomes following the revision surgery are presented in the Table 2. With regard to the functional outcomes, Harris Hip score (from a mean 44.8% to 80.7%), HOOS-JR score (from a mean 49.86% to 70.43%) and Forgotten Joint Score (from a mean 13.63% to 81.82%) were improved in all patients. The same trend was also observed for the VAS score and the EQ-5D-5L score from a mean 0.464 to 0.749 and from 7.91 to 1.91 respectively.
Discussion
The key finding of this study underlines the promising mid-term results achieved by using the Delta Revision TT system combined with morselized impaction allograft for the treatment of moderate-to-severe acetabular bone defects. The goals of a revision surgery, in addition to a stable and durable construct, should also be the restoration of the hip joint biomechanics.20,21 Deficiency of acetabular bone stock is usually caused by osteolysis due to wear of the implants, stress shielding from an excessively stiff implant, loosening and migration of the cup, or infection.15
Severe pelvic bone deficiencies present as a difficult problem in hip reconstruction. Specifically, the goals of restoring or preserving the pelvic bone stock, placing the acetabular component in the anatomical position, optimizing joint stability, restoring leg-length discrepancies and achieving a stable fixation are not easily achieved in such situations. Reconstruction with cages is an appealing option since they act as plates that bridge bony defects, protecting the underlying bone graft as it incorporates eventually restoring the pelvic bone stock. This approach might allow later revision, if necessary, to be achieved with a regular (uncemented) hemispherical cup.21 For these reasons, we perform acetabular revision using the aforementioned cup-cage in combination with impaction grafting.
For acetabular bone deficiencies type 2 and 3 according to Paprosky classification there have been proposed many surgical techniques with varying rates of survivorship. These techniques include the usage of high hip center (HHC) cups, jumbo cups, oblong cups, cemented acetabular shells, custom-made triflange cups, reinforcement rings and cup-cages in conjunction with any of the following: impaction bone grafting, bulky allografts, structural allografts, metal meshes or augments.15,20–23 Regarding these techniques, there have been shown fluctuations in their survival and complication rates in the existing literature. Moreover, the majority of these techniques do not offer a biological reconstruction rendering a future re-revision case even more challenging since they lead to subsequent bone loss in the already compromised bone stock.
The existence and usage of an accurate classification system is of utmost importance in order the bone defects to be addressed accurately and to achieve the best possible result. Till now, an ideal radiological classification system that would provide accurate and standardized algorithm to evaluate the extent of bone loss, assist in pre-operative planning and clinical management does not exist. All these reasons might have been the cause of the proposal of so many classification systems that aim to describe the acetabular bone loss in the setting of a R-THA. Such classification systems that have been used intermittently for the estimation of the acetabular defects are the D’ Antonio (AAOS) classification, Gustilo classification, Engh classification, Groos classification, Charnley classification and the newly proposed SCAR classification.24–26 All of the above-mentioned classification systems didn’t reach acceptable reliability and validity neither the reproducibility needed for a standardized grading system.24 Among of the existing classification systems, the Paprosky classification and/or the AOOS seem to be the most commonly used systems among surgeons. They rely on pre-operative imaging and intra-operative assessment to classify the acetabular bone loss.27 Another commonly used classification system is the Saleh classification. It is based on the anticipated remaining bone stock following removal of the failed implant. It is the only classification system that has shown excellent association and interobserver reliability.24
The last two decades there has been introduced the notion of the cup-cage reconstruction systems. These constructs were firstly described by Nehme et al in 2004. They are considered a hybrid technique in which a cemented liner is implanted in the cage in the vast majority of the cases.23,28 However, in the current study, Paprosky 2B-3B acetabular bone defects, we used the Delta Revision TT system (LimaCorporate, Villanova di San Daniele del Friuli, Italy), a highly porous titanium cup-cage construct, that combines the features from two otherwise different implants into a single reconstruction system. In other words, it combines the unique characteristics of the highly porous titanium along with the characteristics of a reinforcement device. This revision construct, is highly versatile, offering solutions that addresses even the most challenging cases of acetabular revision with severe bone loss. This construct features also three iliac flanges and an ischial hook that can offer supplementary fixation. The ischial hook prevents the whole construct from superior migration while the iliac flanges offer an additional stability. Thus, the primary stability is not entirely shifted to the impacted morselized allograft hence the risk of failure is low.29 Furthermore, hemispherical modules from pure TT can be additionally utilized for the coverage of cavitary defects, that don’t require cement, but rather can be secured by screws. Lastly, intra-cup titanium modules (liner spacers) of 10° or 20° inclination are available in order to facilitate better version as well as coverage, and can also lateralize the center of rotation if needed, as they come in different thicknesses.
To date, there are no many studies reporting on Delta Revision TT system effectiveness. The studies that are available, are mainly case series, consists of small numbers and are highly heterogeneous in term of indication for acetabular revision, as well as the technique that was performed. Moreover, in the majority of these studies, both
Delta Revision TT system and Delta TT One were implanted, and their outcomes were presented in conjunction. However, both short-term as well as mid-term results appear promising with the survivorship ranging between 77.8% and 100% for a median follow-up period varying from 20.75 to 91 months. The details from the available studies are summarized in Table 3.13,14,30–35 In contrast, the present study constitutes a more homogeneous cohort, as only cases with aseptic loosening were included, and the same technique, Delta Revision TT system with supplementary impaction grafting, was used in every case; hence, allowing for safer conclusions regarding the midterm outcomes of this method in particular.
All of our patients were treated with this cup-cage construct, without the usage of hemispherical modules, along with morselized impaction allograft derived from fresh frozen femoral heads. The technique of impaction bone grafting was firstly described by Slooff et al in 1984.17 In the literature, there is a considerable number of studies that refer to the benefits and disadvantages of the different types of bone grafts. It is widely reported that the autologous bone graft is the gold-standard source in cases where a bone defect needs to be restored since it combines the three ideal properties of a bone graft˙ osteoconduction, osteoinduction and osteogenesis. However, the need for additional incisions, the adverse events from the donor site and its limited amount, makes it unsuitable for restoring the acetabular bone defects.29,36 Another option for the management of bone defects are the synthetic grafts (e.g., calcium phosphate, tricalcium phosphate, calcium sulphate, hydroxyapatite particles) and the xenografts. Until now, there is little and inconclusive evidence regarding their effects so their use is either limited or unauthorized for reconstruction of the acetabular bone defects.16,29 Our approach, by utilizing the Delta Revision TT System, provides a structural and biological advantage that overcomes the constraints of autografts, synthetic grafts, and xenografts, offering a reliable alternative for complex reconstructions. The fresh-frozen allogenic bone constitutes the standard source both for structural and for morselized allograft although it carries the risk of disease transmission. Irradiation and freeze-drying (lyophilization) are the two methods of processing the bone graft that are also responsible for their decreased biomechanical properties.15,29 Indeed, irradiation has a detrimental side effect more for the lyophilized bone grafts than the fresh-frozen.29 Regardless the risks, the fresh-frozen allograft is carrying the best results and for this reason is the main choice for the reconstruction of the acetabular bone defects.15
Strengths & Limitations
In assessing the outcomes of the present study, it is imperative to highlight both its strengths and limitations. One of the core strengths lies in the homogeneity of our patient sample and the consistency in the surgical technique applied across all patients in contrast to the other studies presented in the Table 3. This consistency was further supported by a mid-term follow-up period, which aligns with the follow-up durations reported in other available studies. Moreover, this study employed a thorough assessment methodology evaluating functional, clinical and radiological features in order to provide a comprehensive overview of the patients’ outcomes.
However, this study is not without limitations. The sample size, being relatively small, presents a hinder that may limit the generalization of the current findings. Additionally, the retrospective nature of the study, which involved the analysis of prospectively collected data, could induce biases concerning the selection of patients. Such biases might affect the overall interpretation and applicability of the results. Acknowledging these limitations is crucial for understanding this study’s contributions to the existing literature and for promoting future research in this domain.
Conclusion
This study demonstrates promising mid-term outcomes using the Delta Revision TT system combined with morselized allograft for moderate-to-severe acetabular defects. Prioritizing restoration of acetabular bone stock, implant longevity, and favorable clinical results, our approach emphasizes a biologically sound reconstruction method with low complication rates. Nonetheless, long-term studies are imperative to determine the optimal management strategy for each type of acetabular bone defect, particularly in younger patients who are at risk of requiring at least one re-revision surgery in the future.
Corresponding author
Ioannis S. Vasios, MD e-mail: giannisvasios@hotmail.gr
Phone: +30 25513-53000
Academic Orthopaedics Department, Unit for Major Joint Reconstruction, University General Hospital of Alexandroupolis
Address: 1 Dragana str, 68100, Alexandroupolis, Greece
Acknowledgments
None
Author Contributions
Ioannis Vasios: Writing-Original Draft, Methodology, Investigation
Konstantinos Makiev: Writing-Original Draft
Efthymios Iliopoulos: Formal Analysis, Writing-Review Editing
Konstantinos Tilkeridis: Validation, Writing-Review Editing
Georgios Drosos: Conceptualization, Supervision, Project Administration, Performing surgical procedures
Ethical Statement
This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. All procedures involving human participants were approved by the local ethics committee, and informed consent was obtained from all participants prior to their involvement in the study. Data collection, analysis, and reporting adhered to ethical standards to ensure accuracy, transparency, and integrity in the research process. Confidentiality and privacy of participants were maintained throughout the study, with personally identifiable information anonymized where appropriate. No conflicts of interest are reported by the authors. All authors contributed to the study in a meaningful way, and the final manuscript was approved by all co-authors prior to submission.
Patient’s Consent
The patients were informed that data from the research would be submitted for publication, and gave their consent.
Financial Disclosure
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Conflict of interest
No conflicts of interest to declare.