Introduction
The most prevalent cause of shoulder pain is subacromial impingement syndrome (SAIS). The pain and dysfunction in the shoulder joint are the primary symptoms of this syndrome.1 SAIS represented about 44% to 65% of physician consultations for shoulder discomfort.2 It is often described as the impingement of the rotator cuff tendons in the subacromial space.1 The sub-acromial space is located between the anterior acromion, the acromioclavicular joint, the coraco-acromial ligament, and the humeral head.3
The acromiohumeral distance measures the space between the humeral head and the acromion. This measurement is typically used to assess the size of the subacromial space and can be obtained through various imaging techniques, including MRI, ultrasound, CT scans, and radiographs.4 During MRI analysis, several anatomical structures within the subacromial space are identified. These include the subacromial bursa, the supraspinatus and infraspinatus tendons, the biceps tendon, the fibers of the posterior superior labrum, and the suprascapular nerve.5 In extrinsic compression, acromial morphology and shapes play an important role. Research has demonstrated that acromial confirmation does not modify with age but the formation of acromial spur amplifies increases.6
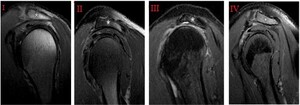
In most studies, two methods are commonly used for the classification of acromion shapes, In the first method, acromion types consist of the superior perspective that has been demonstrated: cobra (Type I), square (Type II), and intermediate type (Type III). The second classification method consists of the underlying perspective and tendency of the acromion described as types as Type I (flat inferior surface), Type II (curved inferior surface), and Type III (hooked inferior surface). In a previous study, the fourth type of acromion was identified by using MRI in 1995 by Vanarthos, which was then added as Type IV with characteristics of a convex underlying area.7 They are categorized as type I, II, III, or IV (flat, concave, hooked, and convex, respectively), as shown in Fig. 1.5 Type III acromion is commonly associated with rotator cuff tears. Biglani et al.8 report the prevalence of type I acromion as 17%, type II as 43%, and type III as 40%.
Another disorder rotator cuff tear (RCT) is described by a debilitated shoulder and pain. RCT is a disorder characterized by shoulder dysfunction and pain. The occurrence of RCT in the generic population is around 22.1%. This disorder is age-dependent as it is found in around 15 to 20% of individuals aged 60 years, 26 to 30% aged 70 years, and 36 to 50% aged 80 years. Its cause is multivariable and can be categorized as inherent factors including deterioration, slight injury, hypoxemia, and external factors including overuse and long-term impingement disorders.9 It is estimated that shoulder pain accounts for 30 to 86 percent of all cases.10 The tendons of the rotator cuff, especially the supraspinatus tendon, are impacted. Exercise treatment has been shown to enhance function and reduce discomfort.4 The prevalence of age-related acromioclavicular (AC) joint degeneration is 54–57% of patients examined with joint pain and is causally associated with rotator cuff tears.8,11–14 AC joint degeneration development has been significantly associated with the >25 years age group.14 Magnetic resonance imaging (MRI) is considered an excellent, non-invasive tool for the detection of SAIS, with the capability of identifying various associated risk factors.15 MRI is essential to assess tendon tear and delineate and evaluate the status of subacromial structures.16 It also allows the evaluation of related intraarticular involvement, bone marrow edema, and joint effusion.17 MRI features of subacromial impingement have been classified significantly into subtypes.17 Type I impingement is the least extreme and encompasses bursal thickening and subacromial bursitis with the normal signal intensity of the supraspinatus tendon; Type II impingement is categorized as an abnormally high signal within the supraspinatus tendon, but without tendon retraction or abnormal intramuscular signal; Type III impingement encompasses abnormal signal intensity with muscle retraction, representing full-thickness tears. There are various diagnostic criteria for the SAIS have been proposed. Typically, clinicians rely on the patient’s medical history with the specified signs and symptoms. Previous studies indicate that individual tests are not reliable for diagnosis while using multiple tests improves their clinical usefulness.18 The study aims to identify that the Acromion shapes (types I, II, III, and IV) combined with different stages of AC joint degeneration from mild to severe create risk conditions for SAIS development. The follow-up MRI assessment for patients reporting suspected Subacromial Impingement Syndrome (SAIS) aims to clarify the contribution of various anatomical structures, specifically the different types of acromion shapes and the degenerative status of the acromioclavicular (AC) joint, in relation to impingement symptoms. This detailed evaluation can help in understanding the underlying causes of the patient’s discomfort and guide appropriate treatment options. This study investigates structural risk factors for SAIS and their associations with rotator cuff injuries to develop improved diagnostic techniques and treatment approaches for impairments affecting this area.
Materials and Methods
Study Design and Setting
This retrospective study was conducted at King Abdul Aziz University Hospital in Jeddah, Saudia Arabia. The data was collected from shoulder MRI scans obtained between 2017 and 2020.
Inclusion and Exclusion Criteria
Patients aged 18 years or older with clinical uncertainty or a confirmed diagnosis of SAIS were included in the study. Medical professionals evaluated clinical symptoms of SAIS by examining reduced shoulder mobility, measuring the subacromial space, and assessing pain during overhead movements. The included patients underwent MRI scans for SAIS. The exclusion criteria included patients with a history of shoulder surgery, tumors, fractures in the shoulder region, or neurological diseases affecting shoulder motion, aside from SAIS.
Diagnosis Of SAIS
SAIS diagnosis is performed through the assessment of both clinical tests and MRI findings. The first step in patient evaluation involves complete medical assessments of the patient. To reduce interpretation biases, licensed physicians accredited by the Saudi Commission for Health Specialties (SCFHS) analyzed all the results. These findings, combined with physical examination tests such as Neer’s test and the Hawkins-Kennedy test, were used for impingement diagnosis. The diagnostic process included testing shoulder mobility for abduction and overhead activity and assessing subacromial space pain during physical examination. The results of the MRI test validated clinical assumptions as the scan evaluated both acromion structure and acromiohumeral spacing and rotator cuff involvement.
MRI Imaging and Assessment
Prior to the study, two independent and blinded MSK radiologists reviewed the sagittal and coronal oblique T1- or T2/PD-weighted MRIs at parallel or 90° to the long-axis of the supraspinatus tendon for possible tendinopathy or tears, obtained from Siemens and Philips machines. The imaging technique followed the standard protocol: Sagittal MRI sequences were used lateral to the acromioclavicular joint to classify the acromion shape and measure the acromiohumeral distance at its shortest point between the apex of the humeral head and the inferior cortex of the acromion [19]. The cut-off of normal acromiohumeral distance was set at 8 mm; below this level, the distance was considered shortened, and <6 mm was set as the significantly shortened distance [20-22]. Coronal oblique sequences were generally selected to evaluate AC joint pathology, the presence of down-sloping, and acromion spur. Axial or coronal oblique images were used to evaluate the presence of OS acromial. The following variables from the MRI examinations were used to analyze the data: type of acromion (I, II, III, and IV), the Presence of down-sloping (Yes/No), presence of OS acromial (Yes/No), Presence of AC degenerative changes (non, mild, moderate, and severe), Presence of acromion spur (non, small, and large), Size of the inferior osteophyte/spur (0.1–3.9 mm = small; >4 mm = large), Acromiohumeral distance, and the status of the supraspinatus tendon (normal, tendinopathy, bursal or articular partial thickness tear, and complete tear). The grading of AC joint used is rather subjective and depends on the degree of severity, based on the classification of Tossy et al.19
Statistical Analysis
The Statistical Package for the Social Sciences (SPSS for Windows, version 23, IBM, Chicago IL, USA) was used to perform the statistical analysis. Frequency and percentages were calculated for categorical variables and mean and standard deviation were computed for continuous variables. A chi-squared test was used to observe the association. A P-value of <0.05 was considered statistically significant.
Ethical Consideration
This study was approved by the Institutional Review Board of King Abdulaziz University with ethical approval Reference No. 350-20
Results
This study included 680 patients with suspected subacromial impingement syndrome (SAIS). Table 1 displays the demographic information of the study participants together with their MRI exam results (Table 1). The patients’ ages were divided into two groups where 327 (48.1%) patients were younger than 50 years and 353 (51.9%) patients were above 50 years. The participant group consisted of equally distributed genders with 340 (50%) male patients and 340 (50%) female patients. Type II acromions were the most frequently reported acromion type 328 (48.2%). The down-sloping behavior of the acromion was detected in 208(30.6%) of patients and OS Acromial was found in 41(6.0%) of patients. Nearly half of the patients 307(45.1%) showed mild signs of degeneration of their AC joint whereas moderate degeneration was present in 121(17.8%), severe degeneration in 22 (3.2%), and 230 (33.8%) patients did not show any degeneration. The study showed that inferior osteophytes occurred in 183 (26.9%) of patients among whom 142 (20.9%) had small osteophytes measuring 0.1–3.9 mm and 41 (6.0%) displayed large osteophytes measuring at least 4 mm. The results showed that supraspinatus pathology was found in 558 patients, 209 (30.7%) with partial thickness tears, complete tears were observed in 143 (21%) patients, and tendinopathy in 206 (30.3%), and normal tendon morphology was observed in 122(17.9%) of cases. The bursal-sided tear diagnosis occurred in 146 (21.5%) of patients who had a partial-thickness tear whereas articular-sided tear diagnosis was among 47(6.9%) patients. Confirmed suspected subacromial impingement syndrome was observed in 393 (57.8%) cases. Partial or complete tears of infraspinatus occurred in 147 (21.6%) of patients together with tendinopathy in 115(16.9%) of cases and 418 (61.5%) of patients did not show any pathology. The mean acromiohumeral distance was 7.62 mm with a standard deviation of 1.52 mm.
Table 2 demonstrates the Type of acromion and AC degenerative changes with the presence of SAIS. Results show that Type II and Type III acromion shapes exist in 184 (46.8%) and 175 (44.5%) of patients with SAIS, However, Type I and Type IV acromion types represent only 17 (4.3%) of cases each. The individual prevalence rate for SAIS shows Type I acromion as the highest at (63%) then Type III acromion (59.3%), Type II acromion (56.1%), and Type IV acromion demonstrating a lower prevalence of (56.7%). Patients diagnosed with SAIS show mild AC joint degeneration most frequently (48.1%) then moderate degeneration (16%) and severe degeneration (3.1%). SAIS shows a regular prevalence distribution across different categories where it reaches its highest level at 61.6% in patients with mild AC degeneration however declines to 52.1% in patients with moderate degeneration and to 54.5% in patients with severe degeneration. Acromion types II and III configurations appear to have a direct association with SAIS based on this evidence. SAIS shows a stronger association with mild AC degenerative changes than with severe degeneration thus suggesting that joint alterations at the early stages could affect impingement onset before degeneration progresses further.
Table 3 displays the relationship between SAIS and multiple associated risk factors. The results showed that females experienced SAIS occurrences at a rate of 54.7% whereas in males 178 (45.3%) cases were observed (p-value= 0.004). SAIS showed an insignificant relationship with patient age distribution (p-value = 0.161). Acromion subtypes did not demonstrate any correlation with the development of SAIS. Patients with down-sloping acromion showed a significant correlation with SAIS (p-value = 0.047). The occurrence of AC joint degeneration also showed an insignificant relationship with SAIS (p-value = 0.286). The evaluation for inferior osteophytes found no significant relationship with SAIS occurrence (p-value = 0.349). Supraspinatus tendon pathology exists in a strong connection to SAIS. The study results showed that supraspinatus tendons were normal in 7.4% of patients with SAIS compared to 32.4% of patients without SAIS at statistical significance (p-value= < 0.001). Complete tears of the supraspinatus tendon along with tendinopathy occurred more often in subjects with SAIS compared to those with AIS. The results further showed that infraspinatus tendon pathology had significant correlations with SAIS. SAIS patients displayed higher rates of partial and complete tears (p-value = 0.002) along with tendinopathy (p-value = 0.005). Acromiohumeral distance measurements proved to be significantly shorter among patients who had suffered SAIS (Table 3).
Discussion
This retrospective study was conducted to identify possible risk factors associated with SAIS. Neither shape of acromion nor AC pathology is associated significantly with SAIS. The results of this study indicated that acromion type and severity of AC degeneration were not a risk factor for SAIS. The results contradict some previous studies, which suggest that SAIS is associated with type III acromion.20–27 While type III was mostly associated with SAIS, the association was not significant. A study conducted by Hirano et al.28 questions the association found in these previous studies, and indicates that the relationship may not be significant, although suggests that the shape of acromion may affect the extent of rotator cuff tear.20–27 By contrast, the results of the present study suggest that the type of acromion is not associated with the pathology of the supraspinatus or infraspinatus tendon (tear or tendinopathy) It was found that AC degenerative changes were also not associated significantly with SAIS. According to Almekinders,29 aggravating factors, intensity, duration, and onset of shoulder pain should be scrutinized, and a gradual increase in signs and symptoms is an indication of rotator cuff pathology associated with SAIS. However, patients with SAIS that have AC degeneration can often pinpoint exactly where their pain occurs at the AC joint, which contrasts with the differential diagnosis in patients with subacromial pathology, who often point to a diffuse area where they are not able to locate the pain accurately.28
Consigliere et al.30 suggested that it is important to understand the underlying subacromial or acromioclavicular pathology in order to treat SAIS with the optimal surgical intervention. Contrary to the findings of the present study, Dalboge et al.31 found osteoarthritis of the AC joint to be related to SAIS, suggesting that the condition is often work-related and recommends further in-depth analysis of SAIS cases regarding the effect of spurs on subacromial tissue compensation. Around half of SAIS cases were found to have mild AC degeneration. Similarly, 47% of type III acromion cases with SAIS also had mild AC degeneration. Alternatively, when downsloping and OS acromial occurred concomitantly, there was a lower chance of having SAIS. Previous studies suggest that downsloping of the acromion is not predictive of SAIS and should not be considered in an examination carried out to classify pathologies of the shoulder joint.32 The clinical relevance of our study highlights the valuable findings in the clinical understanding of SAIS indicating the importance of rotator cuff tendon analysis and gender deliberations in treatment and diagnosis. The practical applicability of this study is to clarify the treatment process and guide clinical professionals in the diagnosis of SAIS. By adjusting the gender differences, acromion types, and AC degeneration the physicians can offer more effective care to SAIS patients that will improve the outcomes of patients. While this study finding suggests that the factors accessed such as acromian shape and AC degenerative changes do not have a significant relationship with SAIS, this study observation is related to an existing study where the relationship between acromion morphology and SAIS was observed as complex and multifactorial.33 In a previous study it was concluded that ASD does not provide any clinically relevant medium to long-term benefit as compared to diagnostic arthroscopy.34 The potential reasons for the difference in the results of studies could include alterations in the different factors like age, disorders, and MRI techniques used to access SAIS. This study aims to explore existing findings in a regional context, to better understand the risk factors of SAIS in our population. This study has several limitations. The retrospective approach introduces inherent biases, as it relies on previously collected data that might not be standardized for the study’s purpose. Furthermore, there were fewer cases of acromion type I and IV in the group, which may restrict the external validity of the findings for these particular acromion types. Although two independent and blinded MSK radiologists reviewed the MRI, interrater reliability was not calculated and will be incorporated in future studies. The possible risk factors for SAIS do not include the evaluation of their sensitivity and specificity as diagnostic tests. However, future research should investigate these MRI findings in the context of diagnosis to determine how effectively these radiological markers can differentiate between SAIS and other shoulder disorders. This would add another perspective to the study, allowing exploration of the diagnostic potential of MRI findings for SAIS. Another limitation was the lack of sub-group analysis in the results such as grouping by demographics or findings related to radiology which could provide an intense perception of the relationship between acromion shapes, AC joint degeneration, and SAIS. In future studies incorporating the subgroup analysis would strengthen the understanding of particular risk factors and their diverse effects among patient subgroups.
Conclusion
The study examined the relationship between acromion configurations, acromioclavicular (AC) joint deterioration, and the development of subacromial impingement syndrome (SAIS). The study findings demonstrate that both the shape of the acromion bone and the degree of AC joint degeneration fail to show meaningful relationships with SAIS occurrence. Type III acromion in conjunction with mild AC joint degenerative changes occurred most often among patients with SAIS, however, the statistical difference was insignificant. The combination of supraspinatus and infraspinatus tendon injuries, along with decreased acromiohumeral distance, was most strongly linked to the development of subacromial impingement syndrome. This indicates rotator cuff conditions play a key role in forming SAIS.
Acknowledgments
The author is thankful to all the associated personnel who contributed to this study by any means.
Author’s Contribution
Single Author paper, all contributions are made by R.A
Conflicting interests
The Author(s) declare(s) that there is no conflict of interest.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.