Introduction
Lumbar facet joint syndrome (LFJS) is known to be an important negative factor regarding public health furthermore being the cause for the majority of working incapacities. Such, the importance of a successful long-term treatment of LFJS is not only of importance for the affected patients, for cost reduction of the healthcare system, but over and beyond for the society itself.1–3
A randomized controlled trial (RCT) conducted by Wu et al. found that PRP injections into lumbar facet joints significantly reduced pain and improved functional outcomes compared to steroid injections. This effect was sustained over time, with the PRP group reporting better long-term relief at 6 and 12 months.1 Another study by Patel et al. showed that PRP injections were effective in reducing chronic low back pain associated with facet joint dysfunction, especially in cases where conventional treatments like corticosteroids had failed.3
Platelet-rich plasma (PRP) injections have been identified as a treatment option for various musculoskeletal conditions, especially for a variety of different joint diseases, including facet joints of the spine, but the clinical data is still evolving. The facet joints are small joints dorsal of the vertebrae in the spine, stabilizing the vertebral column. Pain in these joints can result from different conditions like spondylosis, osteochondrosis, degenerative posttraumatic changes, or reactive arthritis, induced either mechanically, reactively or immunologically. PRP, which contains concentrated platelets and growth factors derived from the patient’s own blood, has been identified to promote tissue regeneration and to reduce inflammation, making it a potential treatment option for facet joint-related pain.4–6
For about 20 years PRP and other autologously conditioned biologics (ACB) are in clinical use and in further clinical development based on the idea to regenerate, and to get an effective biological treatment more or less free of side effects due to its autologous nature. Among these autologous biological therapeutical options PRPs are the most intensively investigated injection therapies.7–12 Clinicians become more and more experienced with the treatment of a variety of joints being affected by osteoarthritis, trauma, or other alterations. In our days PRP therapies achieve increasing importance and are available almost worldwide. That’s why cortisone, NSARs (non-steroidal-anti-rheumatics), or HA (hyaluronic acid) should not be the only and not be the first option for the treatment in any kind of joint disorders.9,13,14
The outcome of a PRP therapy in different joints has been investigated in various studies, most of them reporting a better success rate after 3 to 6 months the latest in comparison to patients treated with cortisone, local anesthetics, or hyaluronic acid. Very good to good results are described in about 75% of all patients after treatment based on autologous conditioned biologics (ACB). One major advantage is the extended period of pain relief, improved range of motion (ROM) and an improvement of the activities of daily living (ADL) in those patients. The positive effect after treatment has been described to last for up to 12 months.15–17
Platelet rich plasma is an autologous, strictly biological therapy. The idea of autologous conditioned biologics (ACB) is to benefit from the body’s own natural sources of the metabolism. All these therapies are restricted on using autologous growth factors and cytokines being extensively expressed by stimulating leukocytes without adding chemical, medicinal or other additives. PRP additionally uses the resources of thrombocytes releasing e.g. PDGF (Platelet derived growth factor) after being activated. Different PRP providers offer varying systems to produce PRP but in general PRP may be divided into two major PRP-groups: Leukocyte-rich PRP (LrPRP), and Leukocyte-poor PRP (LpPRP).10,11,14–16 LpPRP is used more often in orthopedics because of its less pro inflammatory effect to the addressed tissues. ACP is the brand name of the LpPRP from Arthrex ACP® (Arthrex Inc., Naples, FL, USA).18
Only few clinical studies and case series suggest that PRP injections may offer pain relief for patients with chronic facet joint pain. The theory is that the growth factors in PRP, such as TGF-β (transforming growth factor-beta), PDGF (platelet derived growth factor), and VEGF (vascular endothelial growth factor) can stimulate the repair of damaged joint tissues, reduce inflammation, and promote a healthier milieu within the joint.5,19
PRP is generally considered safe because it is produced exclusively from the patient’s own blood, which minimizes the risk of allergic reactions or infections. Most reported side effects are minor and temporary, including injection site pain and mild swelling.12
The purpose of this study is to generate further insights and create new data on the possible long-term effects of the PRP on facet joint mediated low back pain which is one major socio economical factor concerning working disability, and a serious personal burden for the patients affected.
Materials and method
This study was initiated to evaluate the long-term effect of CT-guided facet joint infiltrations with PRP/Arthrex ACP® (Arthrex Inc., Naples, FL, USA) in patients suffering from lumbar facet joint syndrome. The ethics committee of the Aerztekammer Nordrhein has approved this study (protocol-number SOS_EMEA#3 / 2020170).
Patients suffering from lumbar facet joint syndrome with long lasting pain due to facet joint degeneration or facet joint inflammation were included into this study. Before considering offering the opportunity to participate in this study the potential candidates underwent clinical and radiological diagnostics. All patients agreed to receiving 3-4 CT-guided injections to the affected facet joints (periarticular therapy / PAT), either based on PRP / ACP (PRP group) or based on bupivacaine (LA group). The patients were free to choose between the two offered medications. The presented study is a data collection study. Follow up data was collected by a web-based data collection system avoiding any personal contact using mail contact only. After signing the written consent at the CMO, and the initial data collection before administration of the first PAT, the given email questionnaires for follow-up data collection were sent at two and six weeks, and at three, six, and 12 months regarding the pain score, and at 3, 6 and 12 months regarding the Oswestry disability score. Inclusion criteria was longer lasting lumbar pain, located diagnostically (X-ray, MRI) predominantly to the facet joints. Co-morbidities of the lumbar spine were not classified as exclusion criteria. The exclusion criteria met all principles of good medical practice, including patients suffering from any malignancies, hematopoietic diseases, bleeding disorders, infectious diseases, patients with known allergy to bupivacaine or being younger than 18 years of age. Also mentally affected patients not being able to provide written consent were excluded, such as patients suffering from disabling neurological symptoms such as paralysis or cauda equina syndrome or severe scoliotic deformities.
The email questionnaire (SOS / Surgical Outcome Score) was used to collect data using three main categories. Pain was documented according to a range from 0 to 10 with 10 as the worst pain imaginable at every time point, and analyzed for Oswestry disability index at 3, 6, and 12 months. The Oswestry Disability Index (ODI) is a widely used questionnaire designed to assess a patient’s level of disability due to low back pain. It is primarily used in clinical settings to evaluate the impact of spinal disorders on a person’s ability to perform daily activities. The ODI score helps clinicians track a patient’s progress over time, determine the severity of disability, and guide treatment decisions. An improvement in the ODI score after treatment indicates reduced disability and an enhanced quality of life.20 Additionally patients recorded to the Veteran RAND-12 Score, divided into a physical (Physical Composite Score / PCS), and a mental section (Mental Composite Score / MCS).21 The VR-12 (Veterans RAND 12-Item Health Survey) is a standardized questionnaire designed to assess health-related quality of life (HRQoL). It was developed from the SF-12 (Short Form Health Survey) and is widely used in clinical research and healthcare evaluations. The two main aspects of this questionnaire cover pain, physical function, and its effects on daily living activities, and social limitations due to physical or emotional problems.21
Comparing data
The Excel analysis tool was used for data analysis, a p-value of p>0.05 was regarded as significantly different. Inner group analysis comparing result after time were evaluated using paired T-test, for comparison of the two different groups unpaired T-test.
Results
Patient analysis
There were 59 patients included in the PRP-group, the LA-group contained 19 patients. The two groups were comparable with a mean age in the PRP/ACP-group of 63.75 years, compared to 60.32 years in the LA-group. The male/female ratio in the PRP/ACP-group was 1.36, in the LA-group 1.375, each favoring the male patients. Average number of injection-repetitions in the PRP/ACP-group was 3.3, while it was 3.53 in the LA-group. The injection sessions were repeated on a weekly basis. At baseline only 2 patients from each group reported working incapacity. The education level differed between the two groups slightly. Comparing the level of education summarized as primary, secondary, and tertiary level with tertiary reflecting a professional qualification at University, PRP-group versus LA-group had a primary level of 22.5% versus 31.58%, a secondary level of 27% versus 21.05%, and a tertiary level of 50.85% versus 47.37%. A need for oral medication before starting the series of injection was 22.0% at the PRP-group, and 31.6% at the LA-group. With a quote of 17.5% patients, more patients of the PRP group admitted being smokers, compared to the LA-group with 8.3%.
Pain score
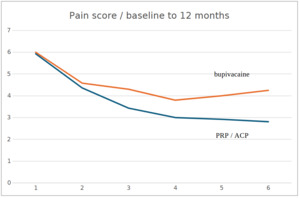
The pain score following PRP injections reduced significantly compared to baseline as early as 2 weeks following the first PAT with a p-value of p<0.001 and remained as significant up to one year, whereas the level of significancy at the LA group was p<0.01 at week 2 ,then p<0.05 up to 6 months. At one year follow up the difference failed to meet the equivalent level of significancy in the LA-group.
Pain at baseline was comparable in both groups with a level of 5.93 (SD 1.215) vs. 6.05 (SD 1.69) in the PRP vs. LA group. Early results after two weeks were also comparable with 4.58 (SD 1.51) for the LA-group compared to 4.36 (SD 2.03) in the PRP group, followed by less pain in the PRP group from week 6 on with a value of 3.44 (SD 2.78) vs. 4.31 (SD 1.75), and further improve at 3 months 3.0 (SD 2.59), remaining stable at 6 months 2.92 (SD 2.18), and 2.81 (SD 2.04) after one year. The LA-group was worse than the PRP-group in all follow-up controls with 6 weeks: 4.31 (SD 1.75), 3 months 3.81 (SD 3.80, 6 months 4.01 (SD 1.89), 12 months 4.25 (SD 2.22) (Table 1 & 2, Figure 1).
Oswestry disability index
The level of significancy at 3 months and six months in the PRP group was p<0.001 and remained significant at twelve months with a level of p<0.001. The LA group failed to meet the level of significancy at one year, but met the level of p<0.05 at month three and six.
While the Oswestry disability index was comparable at baseline between PRP-group vs. LA-group with 23.46 (SD 13.14) vs. 23.15 (SD 9.97), the improvement was significantly dropping in the PRP-group to half with 12.03 (SD 9.68) at 3 months, remaining stable at 6 months with 11.20 (SD 8.28), but slightly raising to 13.65 (SD 12.23) after one year, still being significantly better compared to baseline (p<0.01). The LA-group also improved after 3 months but less to a level of 15.72 (SD 10.63), remaining stable after 6 months with 15.94 (SD 12.41), and 14.38 (SD 9.25) after one year (Table 3 & 4, Figure 2).
Veteran RAND-12 (VR12) Score
At baseline the values of the PRP group and LA group were comparable for physical function (38.6 vs. 34.8) as for mental function (48.4 vs. 45.4). During the observation period the physical function in the PRP group improved, starting at 3 months (42.9) and remained consistently improved until 12 months (43.5, 43.0), while the LA-group only stabilized gradually for 6 months, not reaching the values of the PRP group during the observation period (12 months: 42.0). In the mental analysis the values of the PRP-, and the LA-group were also comparable (48.4 vs. 45.4). At 3 months post treatment both groups improved, but in favor to the PRP-group (53.3 vs. 48.4), remaining good at 6 months (54.6 vs. 47.9). While the PRP group remained on a good level, the LA-group reduced back to pretreatment levels after one year (52.7 vs. 45.0) (Table 7).
Discussion
Low back pain covers a spectrum of many different pain origins with degenerative or reactive arthritis of the facet joints as one leading pathology. That´s why the facet joints are of major importance in the context of disability due to lumbar back pain syndrome. Globally the lumbar spinal facet joint syndrome is an important health and socioeconomic challenge, recognized as an economic burden to all developed economies due to its immense number of employees with incapacity for work. Low back pain is the leading cause worldwide of years lost to disability. The problem is growing due to the increasing population, and even more the progressively ageing population.23,24
Thus, the importance of long-term pain relief respectively the development of new long-lasting treatments is a crucial task for physicians and scientists. Since autologous conditioned biologics (ACB) of other joints like knees or hips are known to lead to prolonged pain relief for up to, or even longer than one year, treating of facet joints offers the potential to handle this socioeconomic problem.10,11,25
Growth factors and cytokines are binding to specific cellular and non-cellular receptors, are so provoking a cellular reaction by changing the expression patterns of the cells. The hypothesis is that changing the cellular expression patterns leads to changings of the composition of the synovial fluid. Thus, leading to a deactivation of the inflammatory process of the activated osteoarthritis, changing the viscosity of the joints, and other potentially recreational biological effects and are so leading of a prolonged pain relief by changing the milieu of joints for longer to the better, and are so improving the activities of daily living.6,25
Clinical studies reporting the characteristics of such biologic therapies in all different joints are numerous, so are meta-analyses. They predominantly describe clinical improvement for an extended period of time, longer than any other injectable therapeutic. The superiority of PRP to HA, corticosteroids, and local anesthetics in terms of clinical improvement has been investigated in many different joints, predominantly for the knee.26,27
The final understanding of the physiology of this effect is still open, but to the best of our knowledge the mode of action might be explained by the given pathway: Injection of autologous biologics into the joint cavity, herewith binding of growth factors and cytokines to the cellular receptors to cells on the superficial layer intraarticularly, finally causing a change of the cellular expression patterns to anti-inflammatory and potentially regenerative expression. This effect of changed cellular expression patterns might explain the prolonged clinical effect to the better in patients treated with autologous biologics such as PRPs.6,27
The therapeutic success rate of PRP in joints has been broadly compared to corticosteroid injections, hyaluronic acid or local anesthetics, which are commonly used to manage facet joint pain. While local anesthetics provide short-term pain relief, such as corticosteroids by reducing inflammation and cutting down the cellular metabolism, PRP appears to offer longer-lasting effects due to its tissue-repairing and anti-inflammatory capabilities. Corticosteroids, on the other hand, carry the potential of side effects, such as cartilage degradation and tissue break down. In comparison to hyaluronic acid injections, which are used for joint lubrication and pain relief also in facet joints, PRP/ACP may have a stronger regenerative effect due to its biological properties. Our previous study6 examining the effect of PRP on the synovial layer in joints suggests that also PRP might enhance the lubrification of joints based on natural and biological mechanisms. However, head-to-head comparisons in facet joint treatments with local anesthetics, corticoids, or hyaluronic acid are still limited.8,9,13,14,22
In this present study we compared CT-guided PAT injections to facet joints based on PRP compared to local anesthetics (bupivacaine) using a pain score and the Oswestry disability index for analyzing the therapeutic effects. This study was designed to use a web based automated questionnaire system to follow up the patients’ complaints for up to one year. While the pain score was comparable to the VAS (visual analogue scale) ranging from 0-10, the Oswestry disability score reflects a sum of 10 different categories according to, and reflecting the activities of daily living, physical and mental restrictions, and is designed for the analysis of therapeutic results following any kind of therapy addressing spinal diseases. An Oswestry score resulting 0-20% is regarded as minimal disability, 21-40% as moderate. Patients included in this study were predominantly classified as moderate with an Oswestry score at baseline of more than 23 in both groups. Patients with moderate disability experience more significant limitations of daily living and may struggle with lifting, sitting, or standing, but basically the patients remain mostly functional.28
In the management of chronic low back pain caused by facet joint degeneration, injections with PRP or local anesthetics are two of many different therapeutic options. Typically, injections with local anesthetics (such as lidocaine or bupivacaine) provide rapid but temporary pain relief due to their action on local pain nerve conduction. Patients often experience a quick reduction in pain immediately after the injection, which may last a few hours to a few days. This makes local anesthetics beneficial for immediate pain relief but does not provide sustained effects on pain management or regeneration. In contrast, PRP injections may not provide immediate relief, as they rely on a slower local biological answer involving the activation of platelets, and the release of growth factors, cytokines, and regenerative proteins. This process might stimulate regeneration and modulates inflammation in the facet joints, but it takes time for these effects to develop. The growth factors and cytokines need to connect to their specific cellular receptors to modulate the expression patterns of the local cells addressed for a potentially prolonged period of time. Consequently, patients receiving PRP might not experience significant pain reduction immediately after the injection but benefit from prolonged effects as regenerative and anti-inflammatory processes set in. That’s why a group of patients suffering from moderate complaints instead of massive pain, is best to address with this biological approach of PRP injections.6,29
The effect of platelet concentrates goes beyond its mere placebo effect, and PRP injections provide better results than other injectable options. This benefit increases over time.30 In this present study we could demonstrate that PRP starts to be beneficial in terms of pain reduction and reducing the disability of patients suffering from lumbar facet joint syndrome after only two weeks. The full effect must be expected after three months reducing the pain level significantly to less than half of the baseline value. We can also show that PRP leads to long term beneficial effects up to one year, thus, not only for pain, but also regarding the Oswestry disability index. The disability of the patients could be reduced from a moderate level (>23) to a minor level of 11-13,5 in the Oswestry score 3-12 months after PAT injections. Patients with moderate Oswestry score usually suffer from reduced job performance, especially in physically demanding activities, even prolonged sitting becomes demanding, and sleep is disturbed leading to chronic fatigue during daytime. Individuals with minor disability experience minimal functional impairment according to pain, sleeping and working disability.
The patients undergoing PAT with PRP in this study improved to long-term minor disability. In contrast to reports in literature the PRP treated patients improved as early as from week 2 on significantly (p<0.001) remaining improved for at least one year post treatment (Table 1, Figure 1). These results contrast with the LA group, although these patients also improve from week 2 on, but showing a less profound improvement compared to the PRP group and the significance only lasts for 6 months. So the comparison of the PRP group to the LA group demonstrates a more profound pain reduction starting at week 2 and continuing during the complete observation period, being still statistically significant at 12 months after injection therapy (p<0.001)
Regarding the Oswestry disability score the data also showed more intense improvement being statistically significant at 3 and 6 months follow-up (P<0.05) (Table 3&4, Figure 2).
These effects are supported by the results of the VR12 score physically, and mentally. The physical VR12 score (PCS) shows significant improvement from month 3 on (p<0.05), with best significancy at 6 months (p<0.01), remaining significant even after 12 months (p<0.05). These results a supported by the results of the mental VR12 score (MCS). A mental score of about 50 represents the average of the general population, and codes for a normal well-being. After treatment, the PRP group is above 50 during the complete observation period, which codes for a mentally healthy, and unharmed collective. In contrary the LA group never reaches a value of 50, and after one year the mental results of the LA group are as bad as before treatment.
No notable complications had been reported in either group. Thus demonstrating a long term effect of PRP injections in terms of pain, and of reduced disability, having a serious impact an working capacity, and so it might be regarded as one suitable method to reduce the socio-economic burden induced by the lumbar facet joint syndrome.
These findings confirm the very few studies on PRP injections for the treatment of the lumbar spine syndrome, we can show that the effect of these biological injections last longer than 6 months for at least one year31–33 Wu et al. compared facet joint infiltrations by PRP also with local anesthetics or cortisone. As we can demonstrate with our results he had also found a longer lasting effect with no major side effects observed.17,34
In summary we can show that repetitive PAT injection using PRP/ACP as a medication are a serious therapeutic option to treat the lumber facet joint syndrome that might often become chronic if untreated. Here we can show that the pain and disability level may be majorly reduced, enabling the patients to live their lives more or less unharmed, and being fully functional for at least one year. These results certainly must be confirmed in follow-up studies probably with a multi-centric design and an even longer lasting control period to explore the full potential of PRP treatment for the lumbar facet joint syndrome.