Introduction
Noise exposure in the operating room (OR) has attracted attention in medical literature due to its potential impact on the health of both surgical staff and patients. This issue is particularly pertinent in the orthopedic OR, as the use of power tools and instruments is often and they generate very high levels of noise. For reference, noise exposure is quantified in decibels (dB), a unit that measures sound intensity or the power level of an electrical signal. The dB scale is logarithmic, meaning that a 10 dB increase corresponds to a doubling of perceived loudness. For example, a normal conversation occurs between 60 and 70 decibels (dB).1 Noise-induced hearing loss (NIHL) is dose dependent. Damage can occur with prolonged (6-8 hours) noise at 80 dB, equivalent to the noise produced by a propeller plane or a diesel train. Just one minute of exposure at 110 dB equivalent to an automobile horn at 1 meter can adversely affect hearing. Exposure to 150 dB can cause eardrum rupture.1 In a broad orthopedic setting, hammering has been reported to generate sound levels exceeding 100 dB(A), while the use of oscillating saws can produce sound levels above 95 dB(A).2
Noise exposure and sound is measured and reported in several ways depending on the context and application of use, this difference is known as weighting. Weighting primarily considers the frequency and filters frequencies according to the necessitated analysis. Unweighted decibels (dB) measure raw sound pressure levels across all frequencies equally, providing a baseline measurement. A-weighted decibels (dBA) adjust the measurement to match human hearing sensitivity, emphasizing frequencies between 500 Hz and 6 kHz, and are commonly used for environmental and workplace noise assessments. C-weighted decibels (dBC) offer a flatter frequency response with less attenuation of low frequencies, making them suitable for measuring peak sound levels and low-frequency noise in settings like concerts or industrial environments.2
Medical professionals, especially those working in orthopedic surgery, are vulnerable to Noise Induced Hearing Loss (NIHL), with studies indicating that up to 50% of orthopedic surgeons show signs of NIHL.1 A recent study investigating 386 orthopedic surgeries revealed that 294 surgeries (76%) exceeded the noise regulations on an A-weighted scale and 22% (10 out of 46) of the surgeries surpassed the maximum acceptable noise level on a C-weighted peak scale. This study however did not report specific orthopedic instrumentation and their corresponding decibel levels.3 According to one study, it has been reported that approximately fifty percent of orthopedic staff members report experiencing noise-induced hearing loss.3 Numerous efforts have been made to implement tools aimed at reducing noise exposure for orthopedic surgeons, such as active noise-reducing headphones (ANRH) ear muffs, and continuous decibel monitoring.4,5 However, early research has shown that some orthopedic surgeons are hesitant to use these protective devices as they may hinder communication between the operating room staff and further research is required on the topic.6
Understanding and quantifying the extent of noise exposure is essential to understanding how it may impact those within and prompt more extensive research into strategies to mitigate any potentially dangerous exposures. The objectives of this study were to conduct a scoping review of the existing literature on noise exposure related to orthopedic instrument use, examine the current recommendations and guidelines for noise exposure in operating rooms, and lastly to identify gaps in current research and propose areas for future investigation.
Methods
Study Design
A scoping review was performed to explore the previous literature that exists regarding noise exposure produced by orthopedic instrumentation. The review process was done using Covidence, a web-based platform designed to facilitate and streamline the process of conducting literature reviews.
Search Strategy
PubMed was the database used to complete this literature review, and the search timeline consisted of studies published between January of 1990 and December of 2023. The search was filtered through terms contained within the “abstract/title” and “mesh terms” selections in PubMed. The general search query consisted of the following inputs: “noise, exposure”, “hearing, loss”, “noise”, “orthopedics”, “orthopedic, surgery”, “operating, room”, “orthopedic, instruments”, “hearing, loss, noise, induced”, “noise, occupational”, “noise”, “arthroplasty, replacement, knee”, “arthroplasty, replacement, hip”, “orthopedics”, “orthopedics”, “operating, rooms”, “orthopedic, equipment”.
Study Selection and Screening
The primary inclusion criteria of this study included noise-based studies in the orthopedic operating room and exclusion criteria included noise-based studies that were not specific to orthopedics, non-instrument-based noise exposure (i.e. measuring level of all noise including music and speaking in the OR) and being unable to evaluate due to a non-English manuscript or inability to access the journal.
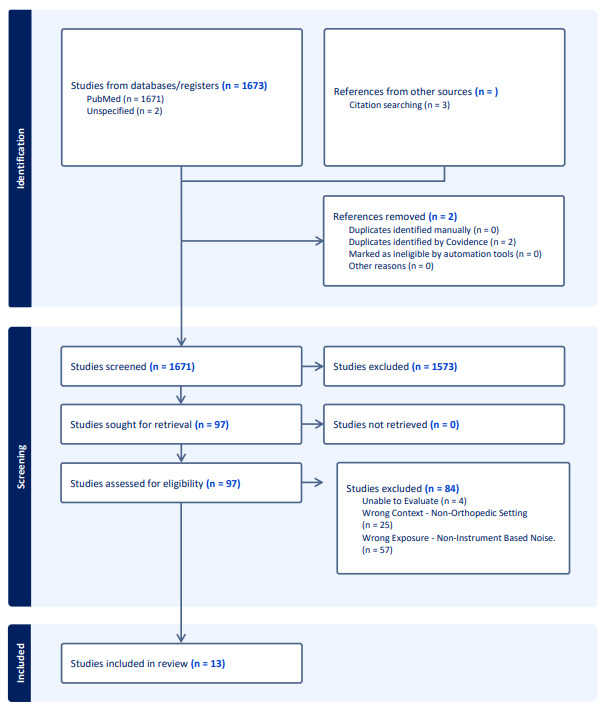
According to our search strategy, 1671 studies were identified for initial screening and 1573 deemed to be irrelevant after subsequent abstract review, leaving 97 papers remaining. These studies then underwent full-text assessment for eligibility which resulted in the exclusion of an additional 84 studies, leaving 13 remaining studies.2,4,7–15 Of the 84 studies reviewed, 57 were excluded due to incorrect exposure (i.e., non-instrument-based noise data), 25 were excluded for incorrect context (i.e., non-orthopedic setting), and 4 could not be evaluated as they were not written in English as seen in figure 1. These final 13 studies were then reviewed, and data was extracted and compiled to provide a review of the noise exposure across orthopedic instrumentation in the available literature. Our reviewer process consisted of a single reviewer protocol through the initial abstract screening phases and then a dual reviewer process for the complete paper review and data extraction phase. Conflicts in decisions or discrepancies in data extraction were then left to a third reviewer to resolve.
Data Extraction
The noise data that was extracted consists of noise levels in A-weighted, unweighted decibels, and A-weighted over time across different types of orthopedic surgery instrumentation. Additional variables include measuring distance from instrumentation to recording device, types of orthopedic instruments, and noise exposure recommendations per various governing bodies presented in each study.
Results
Results were categorized based on whether decibel levels were reported as unweighted or A-weighted, the duration of noise measurement, the type of instrument used (e.g., oscillating and reciprocating saws, drills, drivers, hammering, and reamers), and relevant noise exposure recommendations.
Unweighted Decibels
Three studies evaluated noise levels produced by oscillating and reciprocating saws, drilling, and hammering using unweighted decibel (dB) measurements (Table 1). The findings revealed that oscillating and reciprocating saws generated the highest noise levels, with an average of 99.2 dB and a wide range of 81–131 dB. Drilling produced an average noise level of 88.8 dB, ranging from 78.3 to 97 dB, while hammering activities registered an average of 97.1 dB, with a narrower range of 92 to 103.4 dB.
A-Weighted
Six studies reported the A-weighted maximum decibels (dBA) for various instrument types (Table 2). Oscillating and reciprocating saws had an average maximum of 91.35 dBA, ranging from 53 to 100 dBA. Drilling systems had an average maximum of 87.3 dBA, with a range of 74.6 to 97 dBA. Rasping systems reported an average of 97.6 dBA, ranging from 87 to 110 dBA. Finally, a single study reported a maximum of 87 dBA for acetabular reaming.
A-Weighted over Time (minutes)
Three studies reported on the A-weighted decibels over time, measured in minutes, for different instrument types (Table 3). Time was calculated by the average time the instrument was being used in minutes. Oscillating and reciprocating saws reported an 87.5 dBA average, with a range of 68-100 dBA. Hammering reported an average of 73 dBA with a range of 65 to 81 dBA, while drilling systems reported an average of 82.3 dBA with a range of 72 to 90 dBA.
Noise Exposure Recommendations
In addition to instrumentation data, noise exposure recommendations were analyzed across 13 studies to provide a comprehensive overview of the current literature regarding noise mitigation in orthopedic operating rooms. Analysis revealed that 8 of 13 studies (61.5%) of studies identified clear risks and provided explicit recommendations for noise mitigation, while three (23.1%) presented mixed or ambiguous recommendations. The latter were primarily attributed to the absence of clear conclusions, or insufficient evidence and subsequent calls for further research. The remaining two (15.4%) of studies found no significant risk and, consequently, made no recommendations for noise mitigation. These recommendations were based on various governing bodies in the sphere of environmental and occupational health including guidelines such as the UK Control of Noise at Work Regulations and the European Commission’s Directive for Workplace Noise. These guidelines provide three standards that are designed to protect the health of workers including: lower and upper action values (80 and 85 dBA) and a maximum exposure limit (87 dBA). When the lower exposure action value is triggered, it requires employers to assess the risk to workers health, provide information and training to employees about noise risks, and make hearing protection available. When the upper exposure action value is triggered, it requires employers to take measures to reduce noise exposure and mandates the use of hearing protection if noise cannot be sufficiently reduced by other means. Lastly, the maximum exposure limit at which workers should not be exposed to noise, taking into account implemented reduction provided by hearing protection.
Discussion
Elevated Noise Levels and Their Impact on Hearing and Health
The recognition of excessive noise exposure in orthopedic surgery is not a recent development. Early authors such as Holmes at al. and Willett, publishing data in 1996 and 1991 respectively, identified and quantified the risks of noise-induced hearing loss among orthopedic surgeons laying the groundwork for more modern research.1,9 One excellent example comes from noise data collected during total joint arthroplasty procedures, a common orthopedic procedure performed in the US. Several studies in this review collected noise data from total knee and hip arthroplasties and the resulted in volumes exceeding the recommended 85 decibel (dB) limit set for prolonged exposure, ranging from 74.6 to 123 dBA as demonstrated in Table 2.2,8,10 This elevation was not only seen in one specific instrument but ranged across several including the use of oscillating saws, mallets, and acetabular reamers. These elevated noise levels are not isolated incidents but are found across many other studies outlined in this review and underscore the need for critical examination of decibel levels during orthopedic surgery procedures. As demonstrated by this review, the large majority of the instrumentation volume recorded by our included studies exceeded the maximum recommended exposure limit set in place by their associated occupational health governing bodies. In addition, nearly all data points that didn’t trigger the maximum exposure limit, triggered the lower or upper action values, indicating the need for intervention in the form of education and hearing protection of exposed individuals.
One primary concern associated with exposure to elevated and prolonged noise in orthopedic operating rooms is the risk of noise-induced hearing loss (NIHL) among surgeons and staff. One systematic review included in this review examining literature on NIHL rates among orthopedic surgery personnel revealed that 51% exhibited evidence of NIHL after adjusting for expected age-related hearing loss.3 This review included two early studies, published in 1991 and 1982 and was referenced in many studies also included in this review.1,3,5,7,9,16,17 This evidence is troubling not only due to the high incidence of NIHL but also due to the absence of updated data.
Call for Protective Measures
As indicated by the results of this review, noise exposure in the orthopedic operating room is a significant risk and potential solutions must be considered to protect at-risk individuals. Previous literature has proposed solutions including additional personal protective equipment including noise canceling headphones and earplugs. Multiple authors in this review advocate for the implementation of such noise reduction interventions including the mandatory monitoring of noise levels during surgeries and regular hearing evaluations for orthopedic surgeons.2–4,16 Furthermore, one author proposed real-time decibel measurements to ensure that staff are alerted when noise exceeds safe limits.3
In addition to implementing protective equipment to mitigate exposure to noise in the operating room, efforts should also be focused on reducing the noise profile of new surgical instrumentation. For example, the creation of new instrumentation such as pneumatic broaching systems using in total hip arthroplasties, must be assessed and their noise profile should be considered in both design and clinical use. One study, compared different oscillating saw systems utilized in joint arthroplasty cases and found that different systems produced significantly varying noise volumes, suggesting that there are safer choices of surgical equipment.13
Future Research and Calls for Standardization
This review reveals a significant variation in noise exposure levels across a wide range of orthopedic instruments, underscoring the complexity of assessing noise exposure in the orthopedic operating room. Many of the noise levels documented in the included studies exceeded the recommended exposure limits set by governing bodies, posing potential risks to both surgical staff and patient health. However, the variance in recommendations among the included studies highlights the need for additional research to establish more definitive conclusions and potentially develop evidence-based noise mitigation protocols for orthopedic operating rooms. One critical factor to consider in future research is the standardization of noise evaluation methodologies, as significant variation can contribute to discrepancies in results and subsequent noise exposure recommendations.7,10,13 Several methodological factors that could be standardized, as observed across the 13 included studies, include evaluation distance, decibel weighting, and the use of standardized measurement equipment.
Moreover, the publications reviewed in this paper span nearly three decades of research on noise exposure, with the most recent publication being several years old. This temporal gap highlights the pressing need for contemporary, comprehensive evaluations given the constant development and incorporation of new orthopedic instrumentation across all subspecialties. Noise levels may be an overlooked portion of instrument development in orthopedics and should be considered going forward to minimizing hazards to both medical staff and patients. Furthermore, a detailed analysis of individual instruments is crucial, as recent research has failed to incorporate this aspect, identifying instruments that pose the highest levels of noise exposure. Such standardization and updated research would significantly contribute to our understanding of noise-related occupational hazards in orthopedic surgery and inform evidence-based mitigation strategies.
Conclusion
In conclusion, these findings have significant implications for orthopedic operating room practices. There is a clear call for implementing noise reduction strategies throughout the literature and the potential for designing quieter instruments where possible, improved room acoustics, and further research into adoption of personal protective equipment is key. While this review provides valuable insights into the current state of noise exposure in orthopedic operating rooms, it has also highlighted significant gaps in our current methodology, assessment, and approach to this issue. Addressing these gaps through standardized, comprehensive research and implementing evidence-based noise reduction strategies will be crucial in protecting the health of surgical staff and ensuring optimal conditions for patient care in orthopedic surgeries.
Author Contribution
Mitchel Hawley-Data review and manuscript writing/editing, Anne Boeckmann - Data review and manuscript writing/editing, Lachlan Anderson- Data review and manuscript writing/editing, David Shau - Data review and manuscript writing/editing.
Conflict of interest
None of the authors have any conflict of interest related to this study.