Introduction
With advancing age, the human body undergoes a progressive decline in bone mass and alterations in bone mineralization dynamics, leading to significantly compromised bone integrity. This physiological deterioration exponentially elevates fracture susceptibility. Against the backdrop of an accelerating global demographic shift toward an aging population, this emerging public health challenge demands urgent interdisciplinary attention and evidence-based preventive strategies. According to the WHO age stratification criteria, the population is classified into three groups: young adults (<44 years), middle-aged adults (45-59 years), and older adults (≥60 years).1 Epidemiological studies indicate a prevalence rate of 30% in females and 15% in males under 50 years old with osteoporosis.2 Approximately 8.9 million osteoporotic fractures occur annually worldwide based on comprehensive survey data.3
The decline in bone mineral density (BMD) following peak BMD attainment constitutes a multifactorial and intrinsically complex process. While alterations in sex hormones, nutritional factors, and mechanical loading on the skeleton collectively drive lifelong bone loss in both sexes, significant sex-specific divergences exist in their pathophysiological pathways and clinical manifestations.4,5 In males under 50 years and premenopausal women, the annual bone loss rate ranges from 0.3% to 1.1%. During the 4–8 years following menopause, women experience accelerated bone loss (1.5%–3.5% annually) due to declining estrogen levels. In contrast, bone loss progression is more gradual in males, with an average annual rate of approximately 0.7% after age 506. Given that approximately one-third of osteoporotic fractures occur in middle-aged and older men, understanding the role of preventive strategies (e.g., exercise interventions) in mitigating age-related bone loss within this demographic is of critical importance.
In recent years, the therapeutic advantages of Traditional Chinese Medicine (TCM) in preventing and managing osteoporosis have gained increasing recognition. As a pivotal movement therapy within TCM, long-term Tai Chi practice demonstrates substantial benefits in enhancing bone mass and strength, thereby improving skeletal health. Notably, Tai Chi exhibits significant clinical efficacy in ameliorating symptoms among elderly populations, individuals with osteoporosis, and perimenopausal/postmenopausal women, as evidenced by its capacity to regulate bone metabolism and mitigate age-related bone loss.6
Current research predominantly focuses on the effects of Tai Chi on bone mineral density (BMD) in postmenopausal women. However, the three published meta-analyses investigating this specific population have reported conflicting conclusions regarding its efficacy.7–9
1. Methods and material
1.1. Literature search
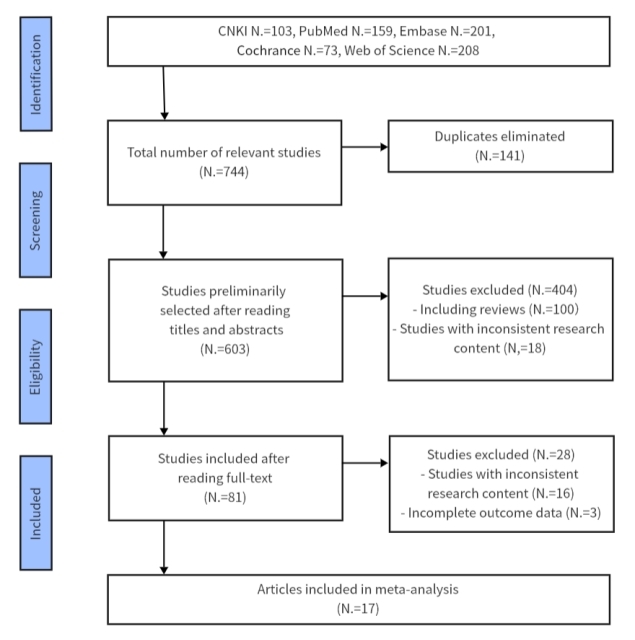
In the Chinese databases CNKI, WeiPu and WangFang as well as PubMed, Web of Science, Embase and Cochrance, The subject headings (" Bone density “OR” Bone Densities “OR” Density," Bone “OR” Bone Mineral Density “OR” Bone Mineral Densities “) AND (” Taijiquan “OR” T’aiChi “OR” Tai Chi Chuan “OR” Tai Ji" OR “Tai-ji” OR “TaiJiQuan” OR “Quan,TaiJi”), using the PubMed search formula as an example (Fig. 1). The literature search covered records from database inception until 28 February 2025. All retrieved raw results were imported into EndNote 20 for screening and duplicate removal.
1.2. Inclusion Criteria
(1) Articles published in English or Chinese. (2) Study type: randomized controlled trials (RCTs). (3) Participants: middle-aged and older adults. (4) No restrictions on gender or age. (5) Intervention: Tai Chi exercise group vs. control group with routine daily activities.
1.3. Exclusion Criteria
(1) Studies involving non-middle-aged/older adults. (2) Meta-analyses or systematic reviews. (3) Literature with inaccessible experimental data. (4) Animal experiments; Irrelevant or duplicate publications. (5) Non-randomized controlled trials.
1.4. Data screening and extraction
The search results from seven databases were imported into the EndNote 20 reference management software. Initially, two independent researchers conducted duplicate screening through both automated (utilizing EndNote 20’s built-in duplicate detection algorithm) and manual verification processes. Subsequently, researchers manually excluded non-qualifying studies according to the predefined screening criteria outlined in Section 1.1. Any discrepancies in literature selection were resolved through consensus discussions with a third investigator.
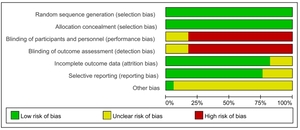
1.5. Risk of bias
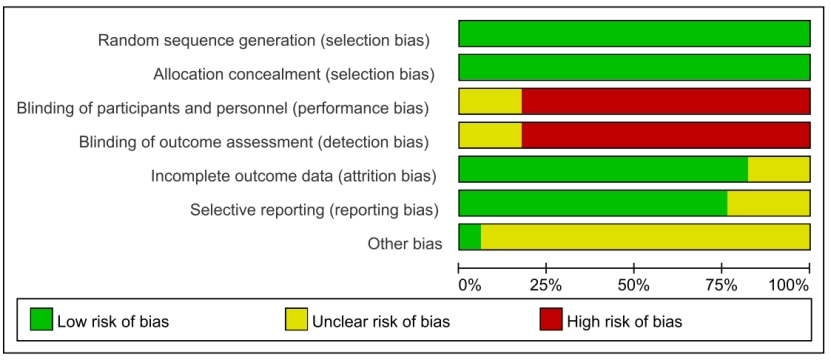
Two reviewers used the “risk of deviation assessment” tool in the Cochrance systematic review to evaluate the quality of articles. The “risk of bias assessment” tool in the Cochrance systematic review assessed the risk of bias of seven indicators including the generation of random sequence, concealed grouping, blinding, selective reporting, incomplete outcome reporting and other bias in articles. Each item was assessed separately for high risk, low risk, and unclear. After the review, the reviewers compared the results, and disagreements were discussed or decided by a third reviewer through consultation.
1.6. Statistical analysis
RevMan5.4 and Stata SE 15.0 software were used for Meta-analysis. The combined effect size of continuous variables was expressed as mean difference (MD). The standardized mean difference (SMD) was used when the means of the outcome indicators were significantly different or the units of the same indicator were different.
The Q test and I2 test were used to test the heterogeneity. p>0.05 and I2≥50% were considered as small heterogeneity, otherwise the random effect model was used. The sources of heterogeneity were further explored by subgroup analysis according to gender, age, and intervention time or frequency. Sensitivity analysis was used to determine the stability of the results. Publication bias was tested by funnel plot.
2. Results
2.1. Literature search results
A comprehensive search across seven databases initially identified 744 potentially relevant studies. Following pre-defined inclusion/exclusion criteria through title/abstract screening and full-text review, 17 eligible articles were ultimately included in the analysis (Figure 2).
2.2. Basic characteristics of the included literature
A total of 178,10–27randomized controlled trials were systematically reviewed (Table 1), encompassing 1,253 participants (experimental group: n=675; control group: n=578). The cohort was stratified into two age-based subgroups: 634 participants aged <60 years and 619 participants aged ≥60 years. All interventions exclusively utilized Tai Chi as the exercise modality, with all 17 studies adhering to this protocol (Table 1).
2.3. Risk of bias assessment
The included 17 studies were evaluated using the Cochrane Risk of Bias Tool for Systematic Reviews. Methodological quality was appraised with the Physiotherapy Evidence Database (PEDro) Scale, a validated instrument for assessing clinical trials in rehabilitation research (Figure 3, 4).
3. Meta-analysis results
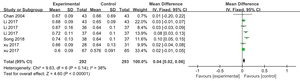
3.1. Vertebral bone density
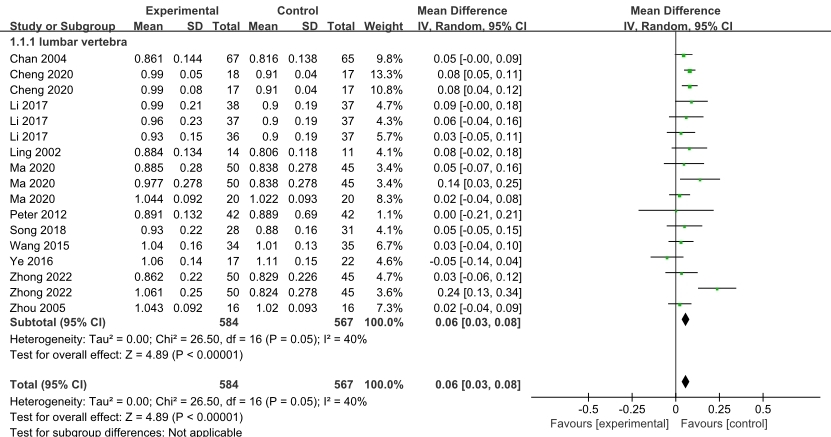
Lumbar Spine: Among the 12 included studies, 18 trial arms reported lumbar spine bone mineral density (BMD) outcomes, comprising a total sample of 1,239 participants (experimental group: n=659; control group: n=562). The meta-analysis demonstrated significant heterogeneity across studies (I²=69%, p<0.00001), warranting the application of a random-effects model. Pooled effect estimates revealed that Tai Chi practice significantly improved BMD at the lumbar spine compared to control interventions (WMD=0.07 g/cm², 95% CI: 0.05 to 0.08, p<0.00001). To further investigate the sources of heterogeneity, sensitivity analysis of the included studies revealed that removing the article by Liu et al. resulted in a significant reduction in heterogeneity (I² decreased from 68% to 32%), while the overall study findings remained unchanged. This indicates that this particular study exhibited higher sensitivity and contributed substantially to the observed heterogeneity, though its exclusion did not alter the direction or significance of the pooled effect estimates. After excluding the Liu et al. study and synthesizing effect sizes, heterogeneity testing revealed low between-study heterogeneity (I² = 40%, p < 0.05). A fixed-effects model was subsequently employed to pool effect sizes. The intervention demonstrated a statistically significant improvement (WMD = 0.06, 95% CI: 0.04–0.08, p < 0.00001), as visually detailed in Figure 5.
Further Analysis of Tai Chi’s Impact on Bone Mineral Density: Subgroup Analyses by Intervention Duration, Training Frequency, and Age Stratification. Participants engaging in Tai Chi training at a frequency of ≥3 sessions per week demonstrated superior efficacy compared to the control group (Z=3.798, p <0.01), whereas those with ≤3 weekly sessions showed no statistically significant difference (Z=1.690, p>0.05). Tai Chi exercise interventions exceeding 6 months demonstrated superior efficacy compared to control groups (Z=10.08, p < 0.01), while interventions ≤6 months also showed significant differences (Z=0.84, p < 0.05). Participants aged 60 years and older demonstrated significantly superior therapeutic efficacy of Tai Chi exercise compared to the control group (Z = 3.893, p < 0.01), whereas no statistically significant difference was observed in those under 60 years (Z = 1.951, p > 0.05) (Table 2).
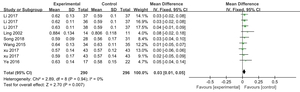
3.2. Trochanteric Bone Mineral Density
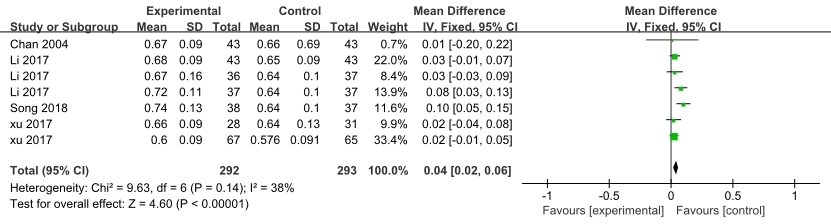
Femoral Greater Trochanter: Four articles included in the analysis encompassed 7 distinct studies reporting bone mineral density (BMD) measurements at the femoral greater trochanter, comprising a total sample of 585 participants.
Meta-analysis results demonstrated low heterogeneity among the included studies (I² = 38%, p > 0.05) based on heterogeneity testing. A fixed-effect model was employed to pool effect sizes. Compared to the control group, Tai Chi significantly increased bone mineral density (BMD) at the femoral trochanter in middle-aged and older adults (WMD = 0.04, 95% CI: 0.02–0.04, p < 0.00001). (Figure 6)
Subgroup analyses revealed statistically significant differences in the efficacy of Tai Chi training interventions based on duration and age stratification: Training Duration Interventions exceeding 6 months demonstrated a significant treatment effect (Z=4.426, P<0.01), Shorter-term interventions (<6 months) showed no statistical significance (Z=1.237, P>0.05). Age Stratification Participants aged 60 and above exhibited marked improvements (Z=4.543, P<0.01) No significant benefits were observed in those under 60 years (Z=1.411, P>0.05) (Table 3).
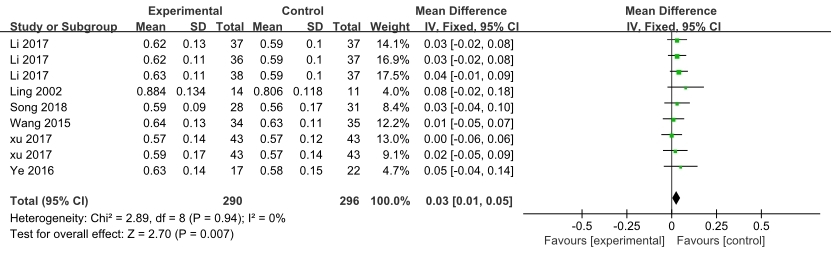
3.3. Bone Mineral Density in Ward’s Triangle
Ward’s Triangle: Six eligible studies were included in the analysis, comprising 9 independent measurements of Ward’s triangle bone mineral density (BMD) across a pooled sample of 586 participants. Meta-analysis findings demonstrated minimal heterogeneity among the included studies (I² = 0%, p > 0.05) based on the heterogeneity test. A fixed-effect model was employed to pool the effect size due to the homogeneity of the data. Compared to the control group, Tai Chi intervention significantly improved bone mineral density (BMD) at the Ward’s triangle in middle-aged and older adults (Weighted Mean Difference [WMD] = 0.03, 95% Confidence Interval [CI]: 0.01–0.05, p < 0.01) (Figure 7).
Subgroup analyses revealed significant differential effects across intervention parameters: Intervention Duration ≥6 months training: Statistically significant improvement (Z=2.351, P<0.01), <6 months training: No significant difference (Z=1.067, P>0.05). Training Frequency ≤3 sessions/week: Demonstrated therapeutic efficacy (Z=2.327, P<0.05), >3 sessions/week: Non-significant trend (Z=1.488, P>0.05). Age Stratification Participants >60 years: Clinically meaningful enhancement (Z=2.41, P<0.01), Participants ≤60 years: No detectable benefit (Z=1.269, P>0.05) (Table 4).
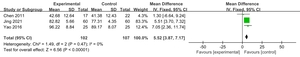
3.4. Femoral Neck Bone Mineral Density
Femoral Neck: Nine studies (12 comparative datasets) with 890 participants reported bone mineral density (BMD) measurements at Femoral Neck. Heterogeneity testing revealed minimal between-study variance (I²=0%, p>0.05), justifying the application of a fixed-effects model for effect size synthesis. The meta-analysis demonstrated that Tai Chi exercise significantly enhanced femoral neck BMD in middle-aged and older adults compared to control groups, with a weighted mean difference (WMD) of 0.03 g/cm² (95% CI: 0.02–0.05, p<0.01) (Figure 8). Subgroup analysis revealed no statistically significant associations between training duration, frequency, and age groups (Table 5).
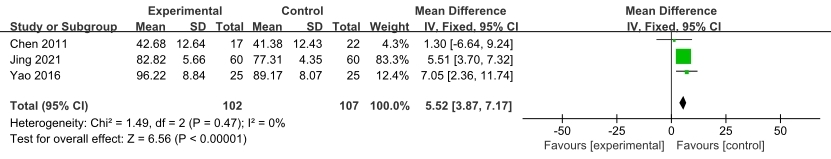
3.5. Calcaneal Bone Mineral Density
Calcaneus: Three randomized controlled trials (RCTs) incorporating calcaneal bone mineral density (BMD) metrics were included, comprising 209 participants across 3 independent investigations. Heterogeneity testing revealed minimal between-study variance (I² = 0%, p > 0.05), justifying the application of a fixed-effects model for effect size synthesis. Meta-analysis demonstrated that Tai Chi intervention significantly enhanced calcaneal BMD in middle-aged and older adults compared to control groups, with a weighted mean difference (WMD) of 5.52 (95% CI: 3.87–7.17, p < 0.01). This effect magnitude indicates clinically meaningful improvements in bone health outcomes (Figure 8).
4. Discussion
With advancing age, the progressive increase in inorganic components and concomitant decrease in organic constituents within bone tissue lead to reduced elasticity and toughness, resulting in brittle bone structure. This biomechanical deterioration significantly elevates fracture risk upon falls and delays fracture healing.28 Physical exercise serves as a critical dynamic regulatory factor in maintaining the equilibrium between osteogenesis and bone resorption, positioning it as one of the key approaches for both prevention and therapeutic management of osteoporosis. Bone strength dynamically responds to alterations in muscular force. The underlying mechanism manifests as mechanical stress generated during physical activity, which modulates bone morphology and architecture. However, in middle-aged and older populations, the progressive degeneration of bodily systems renders vigorous and high-intensity exercise regimens physiologically inadvisable. Research indicates that moderate-intensity aerobic exercise is the most suitable form of physical activity for middle-aged and older adults. Tai Chi (Taijiquan), as an essential component of traditional Chinese culture with a centuries-old history, has gained substantial popularity among elderly populations. Simultaneously, this practice qualifies as a moderate-intensity aerobic exercise characterized by accessibility and simplicity, while demonstrating significant health-promoting efficacy and preventive effects against age-related pathologies.29
As a comprehensive whole-body aerobic exercise, Tai Chi enables participants to enhance musculoskeletal strength through breath regulation. During Tai Chi training, the body maintains a semi-flexed posture, with the lower extremities performing continuous spiral-arc movements against gravitational resistance. This weight-bearing mechanism functions as a natural resistance training modality for lower limb musculature. The specific biomechanical loading patterns exerted on skeletal structures stimulate osteocyte activity and promote structural remodeling, thereby increasing bone mineral density (BMD).30 Clinical observations indicate these adaptations are particularly pronounced in weight-bearing regions such as the lumbar spine and femoral neck.
This study explored the effects of Tai chi on bone mineral density in middle-aged and elderly people, and then selected the appropriate training frequency, period and age, so as to provide guidance for improving bone mineral density index in middle-aged and elderly people. In this paper, the lumbar spine, greater trochanter of femur, neck of femur, Ward’s triangle and calcaneus were analyzed in the intervention of Tai chi in middle-aged and elderly people. Meta-analysis showed that Tai chi can improve the BMD of middle-aged and elderly people, and the content of Tai chi in improving the BMD of lumbar spine was the highest in middle-aged and elderly people. Among them, different intervention period, frequency and age have different training effects. Tai Chi training for improving the BMD of lumbar spine, femoral neck, Ward’s triangle and greater trochanter of femur for more than 6 months training intervention is better than 6 months training intervention. The training frequency of more than 3 times per week is the best to improve the lumbar spine training effect, and the training frequency of 3 times per week or less is the best to improve Ward’s triangle bone density. The effect of Tai chi training intervention on improving the lumbar spine, Ward’s triangle and greater trochanter of femur in middle-aged and elderly people aged 60 years and over is better than that in middle-aged and elderly people aged under 60 years.
The results of this study show that the effect of tai chi training is more obvious when the training period is more than 6 months. The reason is that during the remodeling process of bone, bone resorption is maintained for 4-6 weeks, and the subsequent bone formation takes 4-5 months, which is consistent with the results of this study.31 Training more than 3 times per week can significantly improve the BMD of the lumbar spine of the subjects, which is consistent with the results of previous studies.14
However, training more than three times a week has an insignificant effect on increasing the bone mineral content in Ward’s triangle, and the effect is lower than that of training less than three times a week, which contradicts the results of many studies.8,12,13 As people age, the bone mineral density continuously decreases. In men aged 40 - 50, the medullary cavity of the bone starts to gradually expand. Among them, the changes in the lower limbs are more obvious than those in the upper limbs, especially in the upper part of the femur.1 This study demonstrates that older adults over 60 years exhibit superior improvements in bone mineral density (BMD) through Tai Chi practice compared to middle-aged and older adults under 60, indicating that appropriately designed Tai Chi regimens yield enhanced osteogenic effects with advancing age. Specifically, Cheng’s 48-week Tai Chi intervention trial revealed significant elevation of BMD levels at the femoral neck and greater trochanter in participants aged ≥60 years. Cheng’s12 study demonstrated that a 48-week Tai Chi intervention significantly increased bone mineral density (BMD) at the femoral neck and greater trochanter in adults aged over 60.
While this study implemented rigorous inclusion criteria, certain non-Chinese publications were excluded due to copyright restrictions. Additionally, the predominance of female participants (65.8% of the total cohort) and substantial variability in age ranges (SD=8.2 years) within the included studies precluded subgroup analyses stratified by gender and age. Consequently, the potential gender-specific differences in Tai Chi-induced bone mineral density (BMD) improvements among middle-aged and older populations remain unexplored.
5. conclusions
-
Tai Chi exercise intervention helps improve the bone density of middle - aged and elderly people, with a medium effect size.
-
Tai Chi intervention helps improve the bone conditions of the femoral neck and greater trochanter of the femur in middle - aged and elderly people.
-
Tai Chi exercise for less than or equal to three times per week or more than three times per week can improve bone mineral density in middle-aged and elderly people, but tai chi exercise for more than three times per week is more effective.
-
Tai Chi had an intervention time effect, and the effect of Tai chi training for more than 6 months was better.
-
Tai chi intervention is more effective for the elderly over 60 years old.
Conflicts of interest
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Funding
This study was funded by Traditional Chinese Medicine Research Project of Heilongjiang Province (ZHY2024-021).
Authors’ contributions
Jiqing Cui: formal analysis, writing - original draft, visualization, data curation, conceptualization. Chunsheng Qian: funding acquisition, supervision, writing - review and editing. Jiqing Cui,Yufei Liu,Chunsheng Qian: formal analysis, visualization, data curation. All authors read and approved the final version of the manuscript.