Introduction
Low back and leg pain related to lumbar radiculopathy is a common chronic pain complaint, often resulting from nerve root compression due to degenerative disc disease, spondylosis, spinal stenosis, or disc herniation.1 Interlaminar epidural steroid injections (ILESIs) are widely utilized in the management of radicular symptoms, offering anti-inflammatory effects through the delivery of corticosteroids to the epidural space.2,3 There are a variety of approaches to performing lumbar epidural steroid injections including interlaminar approach, transforaminal approach, and the caudal approach, each with distinct advantages and limitations depending on anatomical and clinical considerations.3–7 In the interlaminar approach, corticosteroids and local anesthetics are injected into the epidural space, situated between the ligamentum flavum and the dura mater, to reduce inflammation and alleviate pain.
The parasagittal technique is one variation of the interlaminar method. This approach may result in more unilateral contrast and medication spread, which raises concerns about its efficacy in patients with bilateral radicular symptoms.8,9 A prior case series described outcomes in six patients who underwent parasagittal ILESIs for bilateral radicular pain.10 The present study expands upon this previous work by evaluating a larger cohort of 12 patients, analyzing both ipsilateral and contralateral pain relief outcomes following parasagittal ILESI for bilateral lumbar radiculopathy.
Methods
A retrospective chart review was conducted on 12 patients who underwent parasagittal ILESIs for bilateral lumbar radicular symptoms. All patients were diagnosed with lumbar radicular pain based on clinical symptoms and corroborating lumbar spine imaging (MRI or CT) demonstrating nerve root compression. All procedures were performed by board-certified pain physicians using the parasagittal approach under fluoroscopic guidance. A 20-gauge Tuohy needle was advanced into the epidural space at either the L4/5 or L5/S1 interlaminar level under anteroposterior (AP) fluoroscopy. A contralateral oblique or lateral fluoroscopic view was also used to verify needle depth and trajectory. After loss-of-resistance technique confirmed epidural placement, 1.5 to 3 mL of contrast was injected to verify contrast spread. All patients exhibited unilateral contrast spread. A therapeutic injection with a combination of local anesthetic, preservative free normal saline, and a steroid was administered. An example of the contrast spread is shown in Figure 1.
Symptom relief was assessed at a two-week follow-up using patient-reported percentage improvement for each leg. Descriptive statistics were used to calculate mean and range of symptom relief on the ipsilateral (same side as contrast spread) and contralateral (opposite side) sides. No additional imaging or repeat injections were performed within the follow-up window.
Results
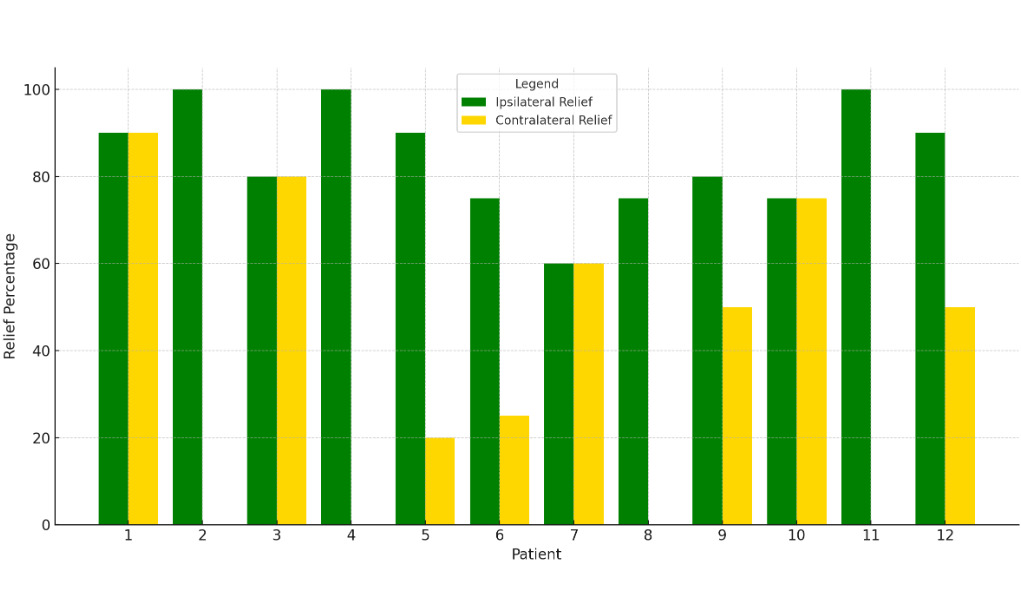
A total of 12 patients underwent parasagittal ILESIs at either the L4/5 or L5/S1 levels with an age range of 37 to 68 years. All patients presented with bilateral lumbar radicular symptoms prior to the procedure. At the two-week follow-up or post-procedure call, all patients reported ipsilateral symptom improvement, with percentages ranging from 60% to 100% (mean: 84.6%). Contralateral symptom relief was more variable, with reported improvement ranging from 0% to 90% (mean: 37.5%). Notably, only three patients achieved high levels of bilateral relief (≥75% on both sides).
There were no reported complications or adverse events during or after the procedures. All patients tolerated the injections well. These findings suggest a strong correlation between the side of contrast spread and ipsilateral symptom relief. Contralateral relief was variable and may reflect systemic steroid effects or delayed epidural diffusion beyond the visible contrast pattern.
A summary of patient outcomes is presented in Table 1.
The results are also presented visually in the bar chart for ease of comparison between ipsilateral and contralateral symptom relief (Figure 2).
Discussion
The results from this case series demonstrate that the parasagittal interlaminar approach to lumbar epidural steroid injection can yield substantial relief of radicular symptoms, particularly on the ipsilateral side of contrast spread. On average, patients experienced 84.6% relief ipsilaterally, and a more modest 37.5% relief contralaterally. This supports the notion that accurate needle placement and target level are important for outcomes.
While traditional midline interlaminar and transforaminal approaches are well-established in the treatment of lumbar radiculopathy, the parasagittal interlaminar technique may offer an advantage by combining the relative safety of the interlaminar route with the directional control of the transforaminal approach.9
The variability in contralateral relief observed in this series highlights the importance of contrast guidance and patient selection.11 Although several patients reported no relief on the contralateral side, a subset experienced significant bilateral improvement, suggesting either spread of medication beyond what was observed with contrast during the procedure or central modulation of symptoms. It is possible that inflammation affecting central canal structures, rather than isolated foraminal pathology, may have contributed to symptom patterns in these cases.
Of importance, this study is limited by its small sample size and retrospective design. Outcomes were based on patient-reported percentage relief rather than standardized pain scores or functional assessments, which may introduce subjective bias. Future studies with larger cohorts and prospective designs are warranted to better characterize predictive factors for bilateral symptom relief and to compare outcomes against midline or transforaminal techniques.
Nonetheless, the data presented in this series support the parasagittal interlaminar approach as a viable and effective technique for managing lumbar radicular pain, offering valuable insight to guide procedural planning for interventional pain physicians.
Conclusion
This small-scale study demonstrates that unilateral contrast spread when performing a parasagittal ILESI provides effective relief on the ipsilateral side with variable relief on the contralateral side. Further prospective studies with larger sample sizes and standardized outcome measures are warranted to validate these findings and refine patient selection criteria.