Introduction
Traumatic brain injury (TBI) is one of the leading causes of death in the United States, with about 1.7 to 3.8 million instances of TBI occurring each year.1 Falls are one of the most common causes of non-penetrating TBI, and account for 35.2% of TBI-related cases.2 A review of emergency department visits for fall related TBI noted an increase in incidence from years 2002-2017 and noted that there is a significantly higher risk in women and older patients.3
Understanding predictors of poor outcomes in TBI is necessary to develop preventative measures in patients and provide greater insight into how to effectively care for and manage TBI in patients. Factors such as age, sex, race and ethnicity, pre-existing medical conditions, medications, injury severity, and intent or mechanism of injury may impact a patient’s post-trauma recovery and outcomes.4 In this study, the authors evaluate the effect of such predictors on the morbidity and mortality of patients who have suffered from fall related TBI. Furthermore, the study seeks to determine the effects of the presence of an abnormal head CT as a predictor in determining outcomes such as hospital admission, in-hospital death, and ICU admission.
Methods
This study is a subset analysis of an emergency department-based traumatic brain injury registry.5 This analysis is limited to the subset of patients who sustained a TBI from a fall. Other mechanisms such as motor vehicle collisions, or assault were not included in this analysis.
Data were abstracted from the electronic medical record using an a priori-designed data abstraction form. Independent variables included patient demographics, and peri-injury symptomatology, including loss of consciousness (LOC), vomiting or seizure following the head injury, the presence of post traumatic amnesia (PTA), or alteration in consciousness (AOC). PTA was defined as being present if the patient had difficulty remembering events immediately after the head injury. AOC was defined as feeling dazed or confused, having difficulty thinking, or if the neurologic exam revealed a decreased mental status.
TBI severity was categorized using the Glasgow Coma Scale (GCS), with severe defined as a GCS score of 3-8, moderate as a GCS score of 9-12, and mild as a GCS score of 13-15. It is important to note that it has been written that there is actually nothing “mild” about TBI with GCS 15.6 Dependent variables included having an abnormal post-injury head CT, being admitted to the hospital, being admitted to the intensive care unit (ICU), and death in the hospital.
Statistical analyses were performed in JMP 17.0 for the Macintosh. Descriptive statistics are reported for cohort characteristics. Medians and interquartile ranges are reported for non-normally distributed variables. Multivariate logistic regression models were built for each of the four outcomes.7 Odds ratios were used to express the strength of association from logistic regression in studies with a binary outcome such as sex or the presence or absence of a symptom such as AOC, PTA, LOC or vomiting.8 The coefficient of variance (R2) was used to assess the extent to which independent variables explained the dependent variable in each of the regression models.9
Data was entered into our institution’s REDCap (Research Electronic Data Capture) database. REDCap is a secure, browser-based, metadata-driven EDC software and workflow methodology for designing clinical and translational research databases. This study was approved by the Institutional Review Board (IRB) as an expedited study with a Health Insurance Portability and Accountability Act (HIPAA) waiver (study # 1882011).
Results
The cohort consisted of 1439 patients, of which 57% were male. The median age was 50 years old, and the interquartile range was 28 to 71 years old. The overall age range of the patients was 18-101 years old. The racial breakdown was as follows: 82% white, 12% black, 3% Hispanic, and less than 5% represent other races. The majority of the cohort had mild TBI, with the median GCS being 15. 268 patients reported using medications of which 19% were on anticoagulants.
The frequency of symptoms was as follows: vomiting at 7%, loss of consciousness (LOC) at 50%, post-trauma amnesia (PTA) at 26%, and alteration of consciousness (AOC) at 37%. A brain CT was performed in 1356 (94%) of the cohort. The table lists the various abnormalities seen in neuroimaging along with their frequencies (Table 1).
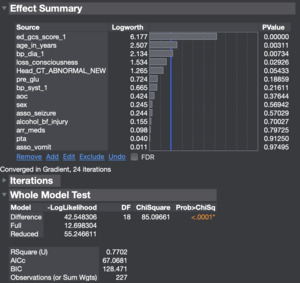
A multivariate model that demonstrates the outcome of in-hospital death correlated with various predictors of the patient without abnormal head CT (Figure 1). The variables that resulted in a statistically significant effect on in-hospital death included the GCS score (P < 0.0001), age in years (P = 0.0002), diastolic blood pressure (P = 0.0024), pre-hospital glucose (P = 0.048), and loss of consciousness (P = 0.02056). The in-hospital death of the patient is not remarkably affected by PTA or anticoagulants. This robust model had a coefficient of determination (R2) of 72%, suggesting that the variables in the model can explain the outcome to a large degree [Figure 1].
Another multivariate model was created with in-hospital death as the outcome, but in this model, abnormal head CT was included as a predictor. The variables that resulted in a statistically significant effect on in-hospital death in this model were the age in years (P = 0.0031), the diastolic blood pressure (P = 0.007), and loss of consciousness (P = 0.029). This model showed a higher, more robust relationship between the predictor variables and the outcome with an R2-value of 77%. The increase in the R2-value from 72% to 77% indicates that abnormal head CT assists as a predictor for the outcome of in-hospital death [Figure 2].
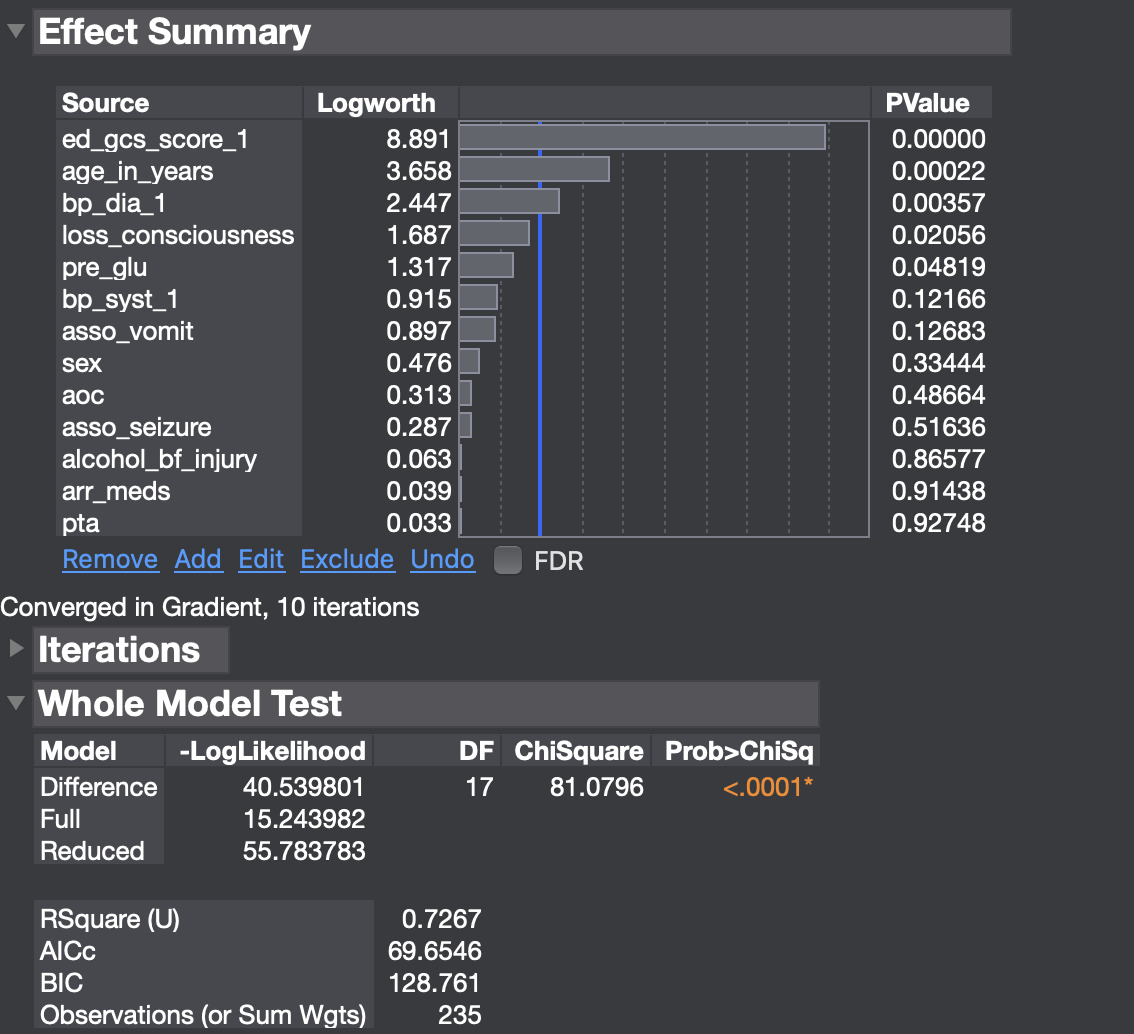
A total of 646 (45%) patients were admitted to the hospital. A multivariate model for hospital admission without abnormal head CT was constructed with various predictor variables as shown in Figure 3. The variables that resulted in a statistically significant effect on hospital admission were the GCS score (P = 0.00023), age in years (P = 0.00241), LOC (P = 0.00121), seizures (P = 0.01343), and pre-glucose levels (P = 0.02160). This model had an R2-value of 29%, indicating that the data shows a moderately strong correlation between patients with TBI after a fall and hospital admission [Figure 3].
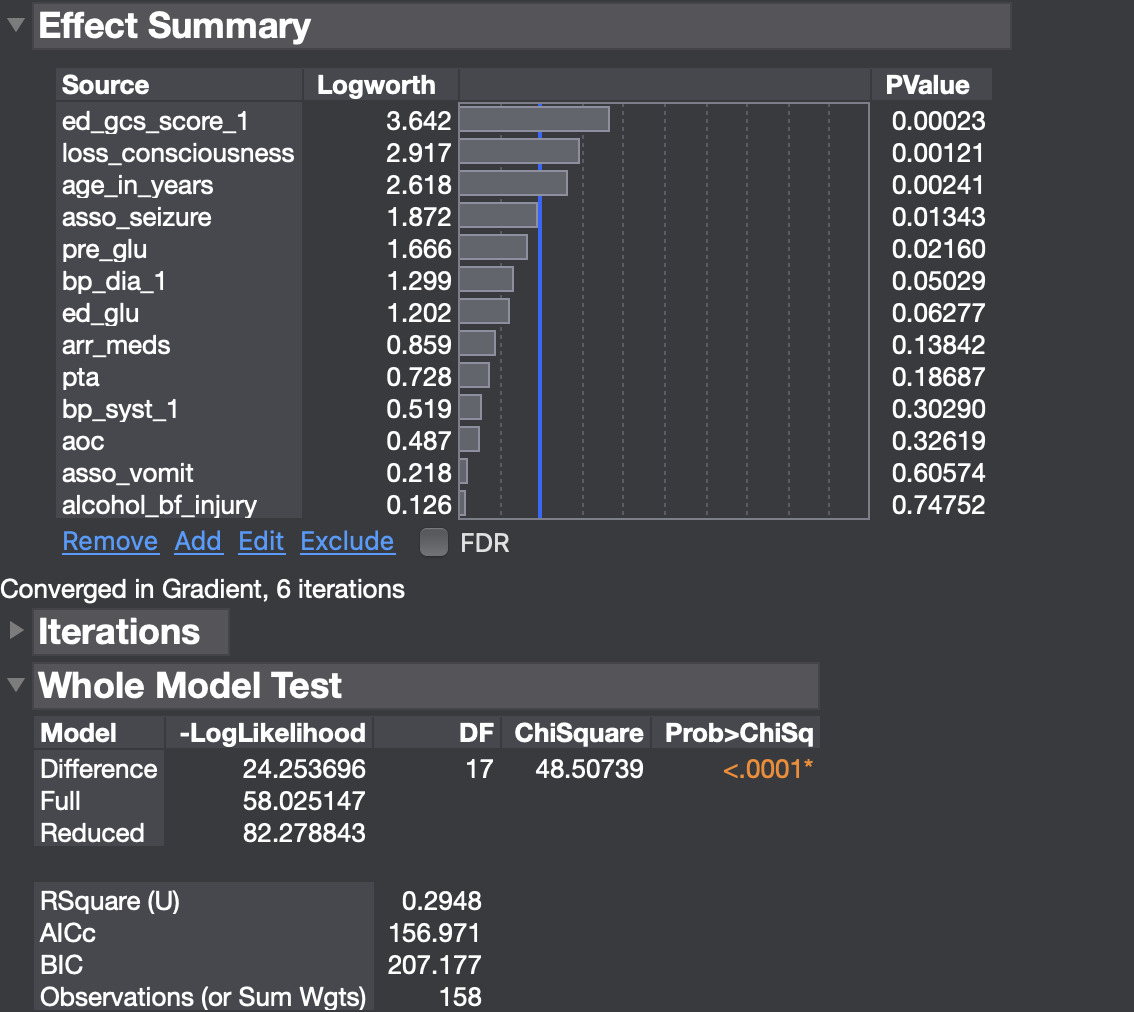
A multivariate model for hospital admission with abnormal head CT was constructed with various predictor variables as shown in Figure 4. The variables that resulted in a statistically significant effect on hospital admission were the presence of an abnormal head CT scan (P < 0.0001), loss of consciousness (P = 0.00514), associated seizures (P = 0.022), diastolic blood pressure (P = 0.04), and age in years (P = 0.048). This model had an R2-value of 59%, indicating that the data shows a strong correlation between patients with TBI after a fall and hospital admission.
A multivariate model for ICU admission as the outcome without an abnormal head CT was constructed with various predictor variables as shown in Figure 5. The variables that resulted in a statistically significant effect on ICU admission were the GCS score (P < 0.0001) and loss of consciousness (P = 0.03). This model had an R2-value of 32%, indicating that the data shows a moderately strong correlation between patients with TBI after a fall and ICU admission.
This multivariable model illustrates the association between abnormal head CT and other predictors of the patient’s admission into the ICU. Abnormal head CT (P < 0.0001), GCS score (P = 0.00003), loss of consciousness (P = 0.03268), and the usage of alcohol before injury (P = 0.04) showed significance in this model. Overall, this model was robust and showed an R2 value of 41% [Figure 6].
Discussion
This study demonstrates the association between various predictors and outcomes of patients with a TBI after a fall. Falling is a significant source of morbidity and was estimated to represent about 695,771 global deaths in 2017.10 Various preventative measures can be implemented to reduce the risk of sustaining a fall-related TBI injury. Adding grippers on socks, using a night light to enhance visibility in low light, adding a gripper mat to the shower, and eliminating any slippery carpeting in favor of less slippery carpet material are some practical measures that could have the potential to decrease the number of falls that occur in a domestic setting. The geriatric population should be especially cautious as age was found to be a key predictor associated with hospital admission, ICU admission, and in-hospital death.
The Glasgow Coma Scale (GCS) was specifically significant in predicting every outcome, with a low score most likely associated with higher mortality and ICU admission rate.11 A low GCS score indicates a more severe injury to the brain, which could increase the chances of herniation, different types of hematoma, hemorrhage resulting in secondary brain injury, and inadequate clinical results such as death and re-admission to the hospital.11 Moreover, patients with a low GCS score are at a higher risk of having cardiovascular and respiratory complications, which could result in a higher possibility of early mortality.12
All the multivariate models, except for ICU admission with/without an abnormal head CT, indicated that age is one of the significant predictors in TBI patients. The majority of elderly patients have some pre-existing medical conditions including hypertension, diabetes mellitus, cardiac arrhythmias, and fluid and electrolyte disorders.13 A greater medical comorbidities conditions in older patients are associated with longer rehabilitation. As such, for elderly patients, pre-existing medical conditions, as well as injury severity and mechanism, must be taken into consideration when attempting to predict outcomes for older trauma patients.13
Abnormal head CT findings in TBI patients show a robust significance with worse outcomes, such as hospital admission and ICU admission, emphasizing the necessity of neuroimaging in TBI patients to help medical professionals predict outcomes and provide proper care. Previous studies have suggested that brain region specificity is thought to play a crucial role in identifying TBI patient’s outcome type and severity.11 Through neuroimaging, medical professionals could identify any subsequent secondary brain injury pattern and develop a treatment plan in order to improve patient outcomes.12
Limitations
This investigation has several important limitations that should temper the interpretation of its findings. First, its retrospective single-center design introduces selection bias: only patients who reached our Level 1 trauma center and had complete electronic documentation were eligible, potentially excluding out-of-hospital deaths, transfers, or patients treated at non-tertiary facilities. Second, many clinical variables—particularly symptoms such as loss of consciousness, post-traumatic amnesia, and alteration of consciousness—were abstracted from routine clinical notes rather than collected prospectively, making them vulnerable to misclassification and information bias stemming from inconsistent charting.
Third, we relied on radiology reports rather than a standardized research re-read of head CT images; inter-observer variability among radiologists and the absence of advanced imaging modalities (e.g., MRI or CT perfusion) may have resulted in under- or over-estimation of intracranial pathology. Fourth, several potentially relevant covariates— for example, anticoagulant type and dose, frailty indices, detailed comorbidity burden, pre-injury functional status, and in-hospital therapeutic interventions—were either unavailable or incompletely documented; consequently, the multivariable models are at risk of residual confounding and may have omitted key effect modifiers.
Fifth, we examined outcomes only through index hospitalization; longer-term sequelae such as 30-day mortality, functional recovery, or readmission were not captured, thereby limiting insight into sustained morbidity. Sixth, although the overall cohort size was adequate, some predictor subgroups (e.g., seizures, herniation patterns) were small, which may have reduced statistical power and produced unstable estimates. Seventh, the study period predates the widespread use of contemporary neuro-trauma care protocols (e.g., direct oral anticoagulant reversal agents, precision blood-pressure targets), so temporal changes in management could affect external validity.
Finally, because all data originated from a single emergency department in an urban academic hospital, generalizability to community hospitals, pediatric or geriatric specialty centers, and international health-care systems remains uncertain. Multicenter prospective studies with standardized imaging review, comprehensive confounder capture, and extended follow-up are warranted to validate and refine the present findings.
Conclusion
The study demonstrates the correlation between the predictors in TBI patients who suffered from a fall and their outcomes after the fall. In the data set, the comparison between models that included abnormal head CT as one of the predictors suggests that abnormal head CT has a strong connection with the outcome of the patients, increasing the R2 in each of the models.