Introduction
Total Hip Arthroplasty (THA) is a surgical procedure that is the conventional modality in treating pathological hip conditions including osteoarthritis or bone necrosis through replacement of the hip joint with artificial components. Removal of the femoral head, acetabular and femoral preparation and reconstruction of the joint all represent possible intraoperative events in THA. Due to innovations in implant design, materials, and surgical techniques, total hip arthroplasty has become one of the most effective and successful surgeries in medicine.1
The first step of THA is in preoperative templating to establish proper positioning and dimensions of patient-specific implants. This is executed by removing damaged parts of the hip joint and replacing it with personalized implants (Fig. 1). A digital templating software is first used to determine femoral, acetabular, and combined offset, as well as leg length discrepancy for a more personalized procedure. From this, there are various approaches such as the direct anterior approach, modified lateral approach, and the uncemented total hip arthroplasty, among others.2 However, the most common technique is the posterior approach, which has been widely adopted since the 1950s. In this methodology, the patient is placed in the lateral decubitus position, lying on one side, with the operative limb draped for easy access for dislocation and to assist with visualization. A skin incision is made from distal to proximal, starting at the greater trochanter and going to about 6 cm along the spine. The underlying muscle is split to expose the short external rotators, and the tendons between these rotators and the piriformis are severed. After incision, the femoral neck and head are exposed and dislocated through controlled hip rotation. The osteotomized bone is removed, and a retractor holds back the posterior capsule for better visualization.3 The acetabulum is reamed, and the femur undergoes preparation. The area is then reconstructed, and artificial components are added depending on patient needs. Following reconstruction, the rotators and posterior capsule are repaired through bone tunnels or by direct soft tissue repair and the wound is closed.4
Although not prominent, total hip arthroplasty can lead to potentially fatal postoperative complications such as a stroke/cerebrovascular accident (CVA). Stroke ranks third as the most prominent cause of mortality in the Western world5 and encompasses a broad spectrum of pathologies characterized by a lack of cerebral blood flow through an obstructing (ischemic stroke) or ruptured (hemorrhagic stroke) blood vessel.6 This event may occur from perioperative hypertension, platelet buildup, as well as complications that can occur due to side-effects of pain-relieving drugs.7 Understanding the various risk factors leading to postoperative stroke is essential to mitigating the incidence of postoperative stroke and other potential complications to ensure perioperative patient safety.
In order to ensure the safety of the surgical procedure, it is critical to take note of potential consequences and risk factors that may worsen patient outcomes. Key potential risk factors include a previous history of diabetes, coronary artery disease, smoking, renal insufficiency, patient age, among others.8
While postoperative stroke is generally uncommon, its potential severity necessitates an in-depth understanding of potential perioperative risk factors. As total hip arthroplasty becomes more prominent and more frequently used, existing comorbidities, demographics, and other intraoperative variables must be examined as factors to further examine to minimize patient complication uncertainty. This study aims to evaluate potential risk factors pertaining to postoperative stroke specifically after total hip arthroplasty to better inform existing protocols, guide decision making, and ensure consistent improvement in patient outcomes.
Methods
This retrospective cohort study utilized patient data from the American College of Surgeons: National Surgical Quality Improvement Program (ACS-NSQIP) database, a robust, de-identified surgical registry that aggregates clinical information from over 700 hospitals across the United States on an annual basis.9 This data looks at over 11.6 million HIPAA compliant participant use files (PUF) and categorizes patient information by utilizing over 200 surgical perioperative variables, allowing for comprehensive analysis of surgical risks, trends, and outcomes.10
A search query initiated between January 1st, 2017 and December 31st, 2021 examines patients who underwent total hip arthroplasty recorded under the respective identifier for the current procedural terminology (CPT; code 27130). Analysis of relevant indicators yielded risk-predictive variables associated with postoperative stroke including demographic characteristics (age; sex), baseline comorbidities (diabetes; hypertension), relevant preoperative laboratory values (albumin; INR), ASA physical status classification, and other intraoperative metrics (general anesthesia). JMP (SAS), a statistical software environment for data exploration and discovery, was employed for statistical experiments with its embedded graphical user interface (GUI) for dynamic regression analysis11
A threshold value of p<0.05 was set to determine statistical significance. Parameter estimates, Pearson’s chi-square p-values, and confidence intervals (CI) contributed to the computation and estimation of regression per unit increase in variables.12 A native 95% CI from JMP was also utilized for all odds ratios.13 Screening with a preliminarily univariate analysis of these variables against mortality determined factors associated with postoperative stroke. The identified variables were used in a multivariate logistic regression model to isolate independent predictors.14 Univariate and multivariate analyses were then repeated excluding the frailty index to avoid functional redundancy and overlap with functional status.15 This approach allows for targeted evaluation of patient specific and procedural factors that contribute to stroke and cerebrovascular accident risk following THA.
Results
This analysis includes 199,960 patients in the cohort (54.8% female; median age of 66). This study analyzes data from the National Surgical Quality Improvement Program (NSQIP) from over 700 hospitals nationwide (Fig. 2). The most common self-reported race was White (69%, n=137351) followed by a significant portion of patients whose race was reported as unknown or not reported at 21% (n=41336). The study population included patients from age 18 to 89 years with a median age of 66. The median BMI was 29.6 with an interquartile range from 25.8 to 34.0 Additionally, 88% of studied patients were nondiabetic and nonsmokers, while 98% of patients reported independent functional status. ASA class was also mainly level 2 and 3, representing 51% (n=101057) and 44% (n=87912) of the data respectively. The findings of this study show that age, use of general anesthesia, a history of smoking, and longer surgical duration are all significant predictors for postoperative stroke after total hip arthroplasty.
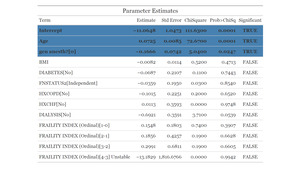
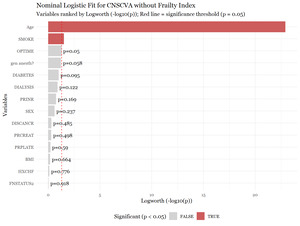
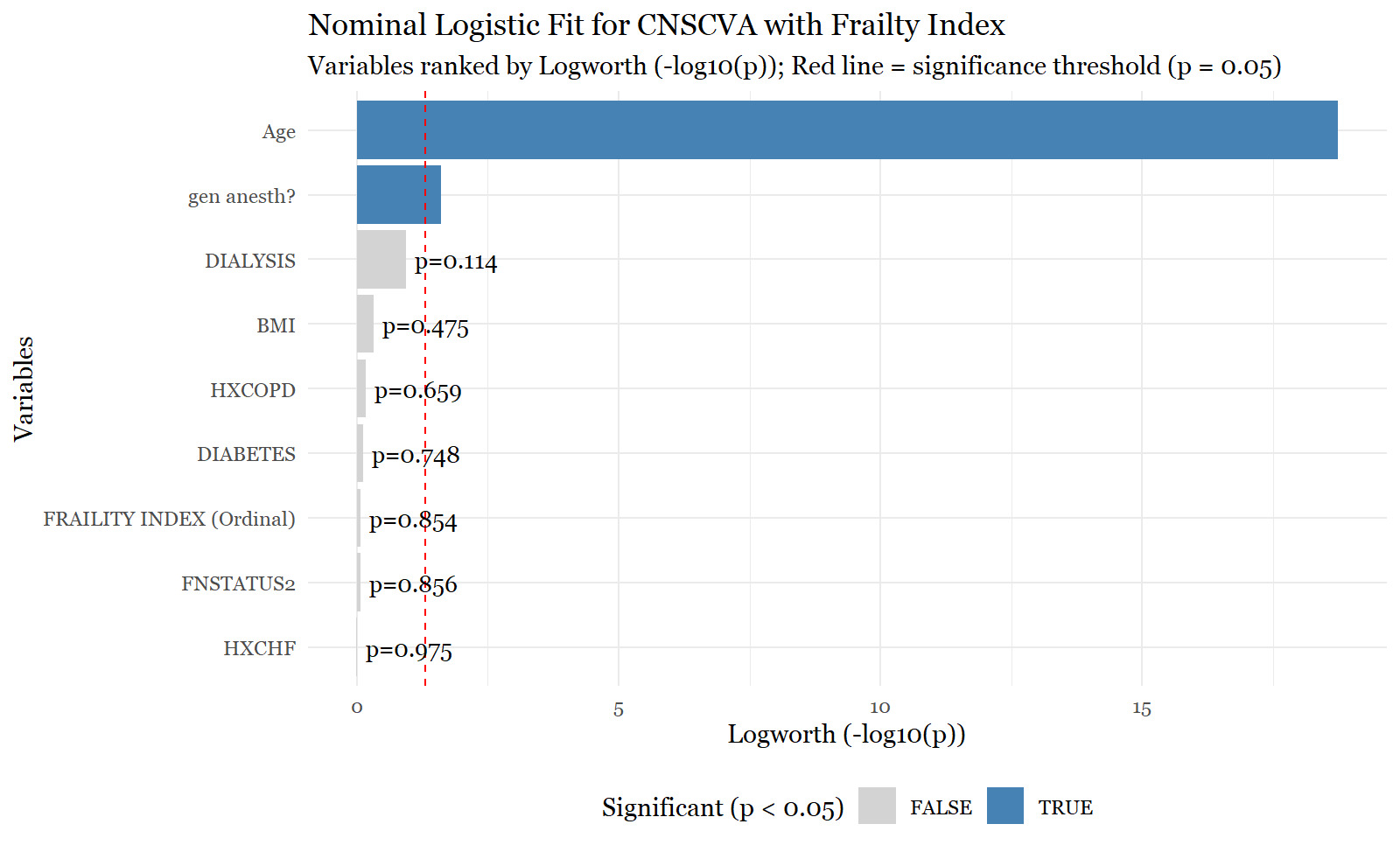
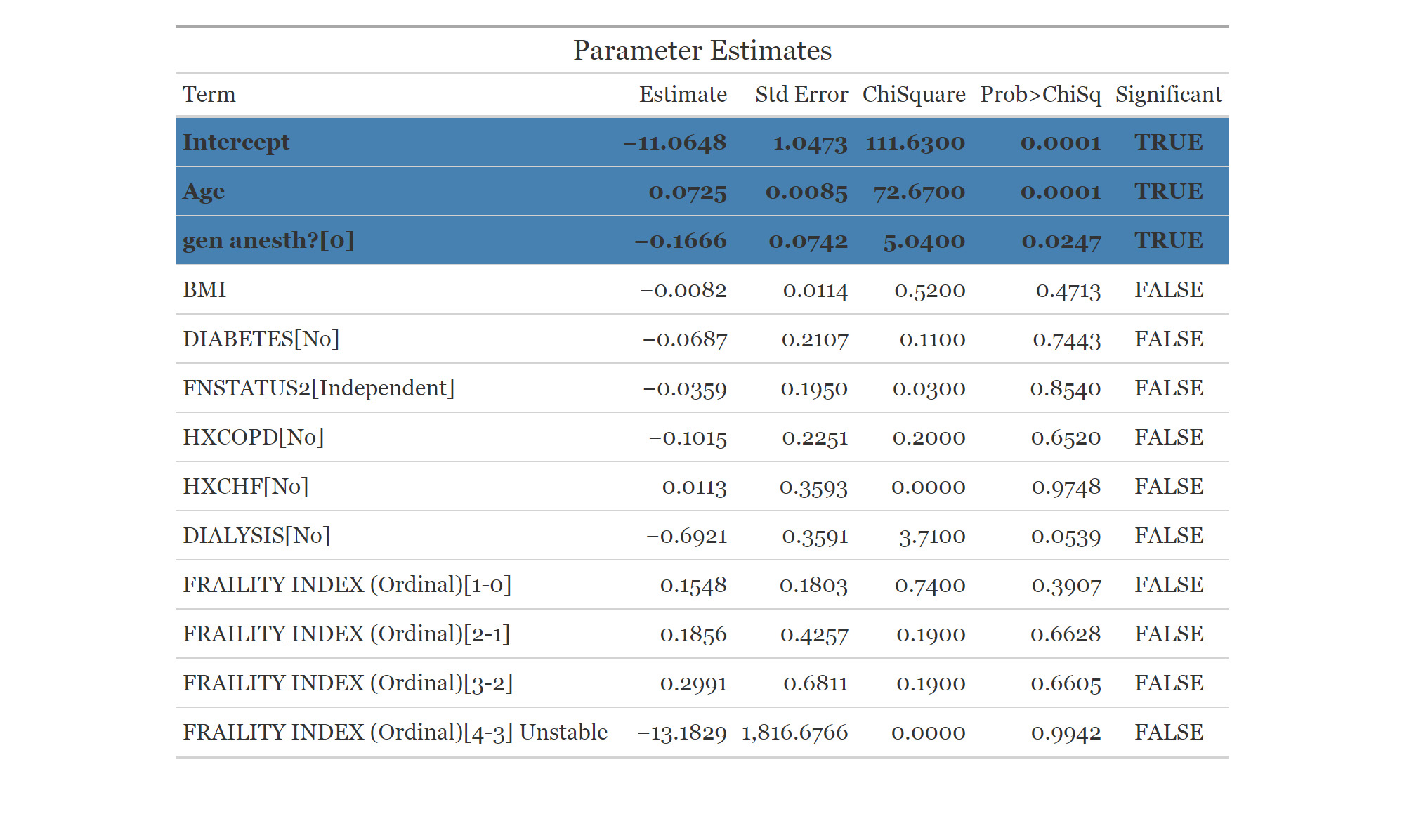
In the univariate analysis, variables were ranked according to their logworth values and significance was determined using standard p-values. For postoperative stroke or cerebrovascular accident (CVA), significant individual predictive variables were mainly age (p < 0.0001) and the use of general anesthesia (p = 0.0250) (Fig. 3). These risk factors did not lose significance in the multivariate analysis, nor did any additional risk factors become significant. The p-values for these multivariate values were p <0.0001 for age and p = 0.0247 for a patient undergoing general anesthesia (Fig. 4). Additionally, the odds ratios for these variables in the multivariate analysis were 1.075 with a 95% confidence interval between 1.057 and 1.093 for age and 1.395 with a 95% confidence interval between 1.043 and 1.866 for patients undergoing general anesthesia (Fig 5). This indicates that age is a very strong predictor for postoperative cerebrovascular accidents with each additional year of age increasing stroke risk by around 7.5%. Patients who had general anesthesia during the procedure had about a 40% higher chance of postoperative stroke. Additionally, when taking into account confidence intervals in the test for significance, body mass index also becomes significant. The R2 value for this model was 0.0397, suggesting that the majority of variation of the predictive factors does not align with that of the model. Therefore, about 4% of the variation in patients who experience a stroke can be explained through this model, demonstrating that other factors may contribute further to predict stroke risk.
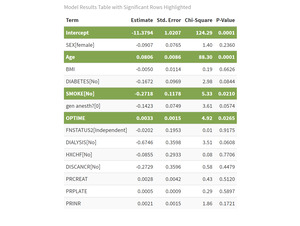
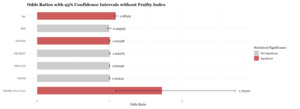
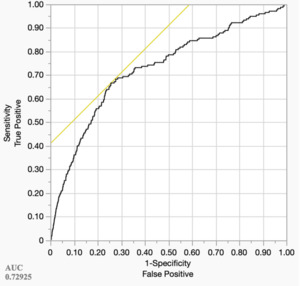
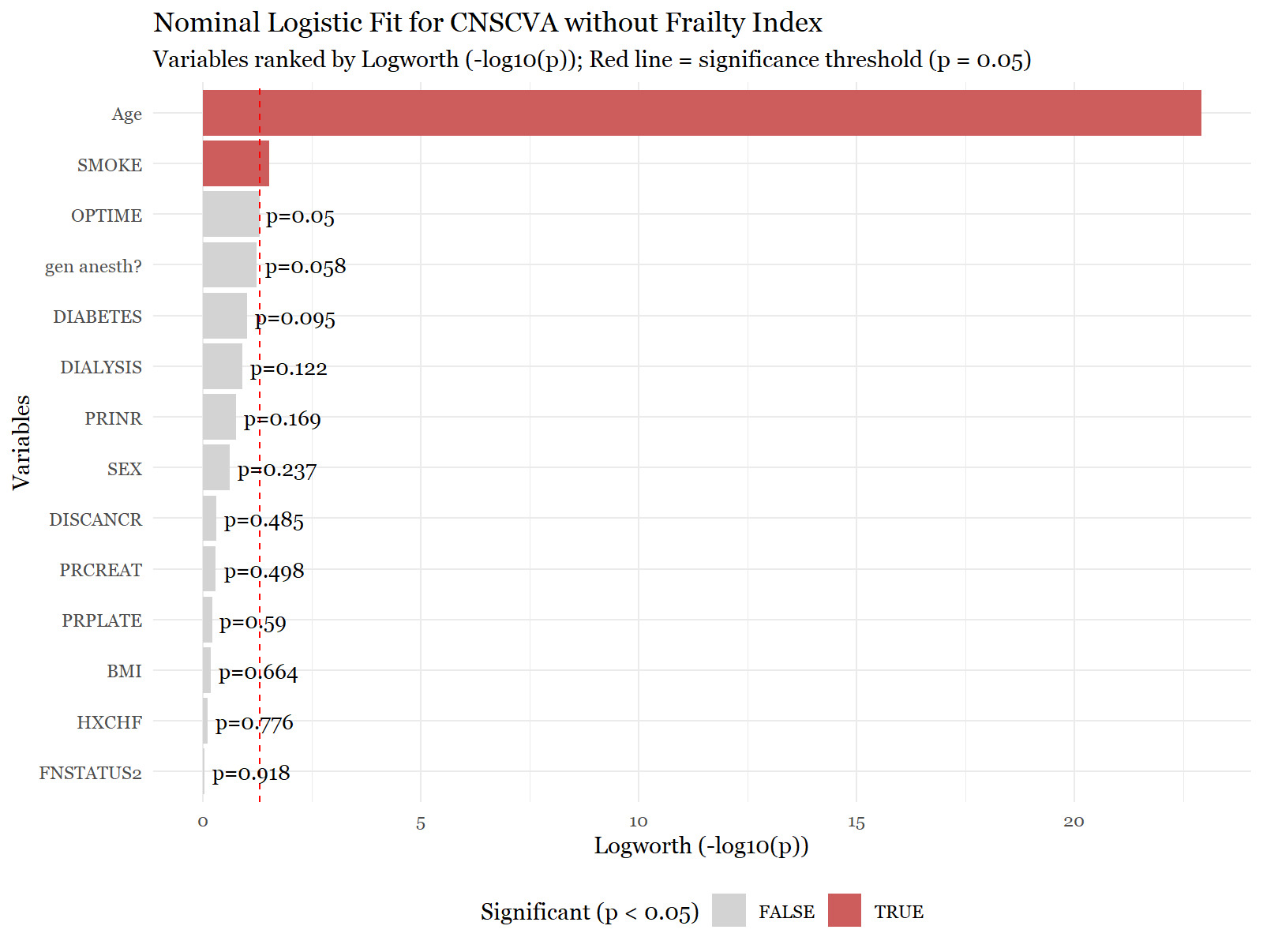
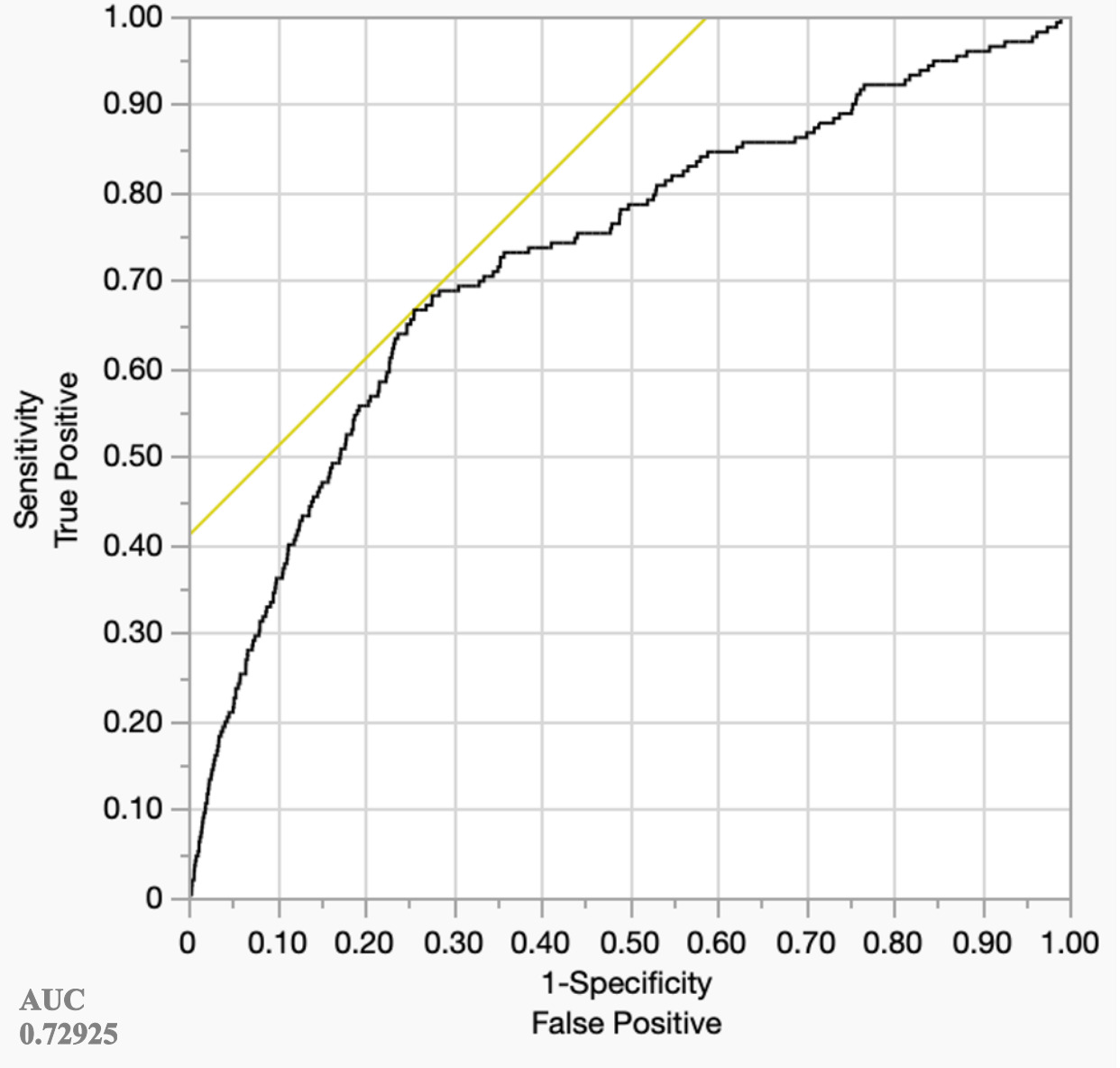
Following this, a sensitivity analysis was conducted where the predictive parameter of frailty index was excluded from the dataset due to its statistical and conceptual redundancy with functional status, as both are utilized to evaluate patient health and potential vulnerabilities.16 Under this model, the univariate analysis for postoperative stroke has significant risk factors of age (p < 0.0001) and smoking status (p = 0.0298), which is further depicted in Figure 6. In the multivariate analysis, as seen in Figure 7, the statistically significant values include age (p < 0.0001), smoking status (p = 0.0210), and operation time (p = 0.0265). According to Figure 8, the odds ratios for these variables were the following: 1.084 with a 95% confidence interval between 1.066 to 1.102 for age, 1.722 with a 95% confidence interval between 1.085 to 2.732 for patients who smoke, and 1.003 with a 95% confidence interval between 1.000 and 1.006 for surgical duration. Once again, age is a very strong predictor of postoperative stroke with increasing odds of 8.4% with each additional year. Moreover, smokers have a 72% higher odds of stroke, and each additional minute of surgery increases the potential of stroke by about 0.3% meaning that every additional hour may lead to about 20% higher risk for complications. Overall, the AUC for the ROC was acceptable at 0.72925 (Figure 9). The R2 value for this model was 0.0437, indicating a higher alignment of variation between the predictive factors and the model. These statistical metrics depict that there is a generally acceptable chance of around 72.9% chance that the model correctly distinguishes between risk factors and complications. The lower R2 value indicates that roughly 4.37% of the variance of stroke risk can be explained by the model.17
Discussion
Age was the most consistent predictor of stroke in univariate and multivariate models, with or without the frailty index included. In the preliminary model, results displayed that each additional year increased stroke risk by about 7.5% while it has an even greater risk, 8.4% in the more refined model. Advancing age may predispose individuals to microbleeds, additional unaccounted for comorbidities, or dysregulated cerebral mechanisms that enhance potential complications following surgery.18
The initial model also displayed the use of general anesthesia to increase stroke risk by 40%. Although this finding did not retain its statistical significance in the adjusted model, it indicates the potential benefits and need for further study on different forms of anesthetics and their varying physiological effects on patients. Patients receiving general anesthesia often experience extended hospital stays, which may be linked to a more complex recovery period. General anesthetics also are correlated to arterial hypotension and pulmonary infections and outcomes that could possibly explain why stroke may be more common.19,20 This may lead future research to discuss the possibility of using other anesthetics on patients for improved surgical outcomes, such as using caudal epidural anesthesia, which has shown to be promising.21
The adjusted model also showed smoking increasing stroke risk by 72% and longer surgical time increasing risk by 0.3% per minute. This could be due to smoking’s subsequent relation to diabetes, increased blood pressure and heart rate. All of these factors play large roles in increasing the likelihood of stroke.22 Specifically, the nicotine in cigarettes and other smoking products activates nicotinic acetylcholine receptors (nAchRs) which activates various neurotransmitters that will increase heart rate and blood pressure. This can cause oxidative stress, change cerebral blood flow, or increase inflammation in the body, which can all lead to cerebrovascular issues.23 Another possibility is that the increased carbon monoxide in the body made during smoking reduces the oxygen carrying capacity of erythrocytes, which causes endothelial damage. Additional free radicals and excess metals in smoking products may also lead to further endothelial damage, putting patients at higher risk for thrombosis, and therefore stroke as well.24
Moreover, additional surgical duration can consequently come from complications during surgery, which may predispose individuals to a higher probability of experiencing a postoperative stroke. For example, increased operation time during orthopedic surgery is linked with further cardiac complications, renal failure, and sepsis. The complications are all indicators that place patients at higher stroke risk following surgery.25 This highlights the importance of doing further research to ensure efficient timing when in surgery.
Limitations
This study is limited by its retrospective approach and reliance on data entry from this database alone, which may lead to statistical variances in reported strokes and potential variations in reported comorbidities. Additionally, postoperative stroke is not a common complication succeeding total hip arthroplasty, which also limits potential results. Future work would aim to expand the patient database to receive more information regarding potential stroke. Additionally, the modest R2 value of 0.0437, meaning its discriminatory abilities are moderate. This likely points to the fact that stroke tends to be uncommon as a later complication of THA. For instance, from a prior study of over 1.7 million total joint arthroplasties, 0.14% of the selected sample experienced a postoperative stroke, of which 79.45% were identified as ischemic strokes while 20.55% were hemorrhagic.26 The ROC curve (Fig. 9) includes a reasonable AUC of 0.72925 which indicates an acceptable level of model performance in describing and predicting outcomes from patients who were affected by a stroke against those who did not. This value above 0.7 reflects that although this model gives meaningful data, there may also be other potential confounding variables that may affect outcomes and therefore require further study. For example, specific types of anesthesia or other predisposing conditions may play a role in postoperative outcomes. In the future, studies should expand on the type of data collected to offer more accurate results with more discriminatory values that may explain this model further.
Conclusion
This national cohort study showcases key patient demographics and comorbidities that are associated with postoperative stroke after undergoing total hip arthroplasty. Advancing age was the most prominent risk factor for cerebrovascular events in both univariate and multivariate analyses in the preliminary and adjusted model. The preliminary model also informed that using general anesthesia during the procedure increased risk of further complications. Additionally, minimizing operation duration and addressing modifiable lifestyle alterations such as smoking may be beneficial to improve surgical outcomes. Integrating these findings to clinical strategy may influence operative decision making and will add critical data to inform future investigations. Although postoperative stroke remains a low frequency complication following total hip arthroplasty, its clinical severity permits additional research into prevention, early detection, and long-term effects. Further refining and studying such perioperative strategies will be able to reduce stroke incidence and will serve as an imperative foundation for future risk reduction strategies.