Introduction
Speciality training in the UK has been under immense pressure for the last few years, with Trauma and Orthopaedics speciality training being no different.1–5 Between the introduction of the European Working Time Directive (EWTD) and service provision, trainees face more challenges towards their learning tasks and achievement of the targets set by the Joint Committee on Surgical Training (JCST).6–8
On one hand, the implementation of the 48 working hour scheme per week means less exposure to operative skills alongside other clinical duties for the trainee, which in turn would put the trainee under pressure to deliver the expected quality of work in a timely manner.8,9 On the other hand, the obligation to deliver a standard of care alongside the strain on hospitals to accommodate the long waiting lists led to a further decrease in the operative opportunities and the supervised sessions for the trainees. This was best demonstrated in a national review, published by the British Orthopaedic Association (BOA), of the adult elective orthopaedic services in England; more than half of the trusts included in this review struggled to maintain the 18 week referral to completion of care target which could be due to various factors, such as ageing population and the increase in the joint revision rates.10 On further analysis of the results, it was found that the surgeons who were involved in hip and knee operations were mostly experienced consultants, prompting fears towards the productivity of the following cohort of surgeons.11 Therefore, in the light of all these challenges, trainees will have to maximise their benefit out of the available operative time.
It is understood that with the current financial strain on the National Health Service (NHS), light is shed upon the cost-effectiveness of operating theatre time. This led to the introduction of “The Productive Operating Theatre” initiative in the NHS, which aims to counteract the inefficiency found in the operative theatre environment.10,12 It is understood that the average hourly cost of a single operative theatre is around £1,200. In October 2017, NHS Improvement published a study across 100 NHS trusts in England that operating theatres waste nearly two hours daily. Furthermore, an additional 280,000 operations would have fit in the operative list schedules had the operative lists been properly planned.12 An important component of operative list planning is being conversant with the duration of each of the commonly performed procedures, as well as the different components of an operative theatre session.13 The anaesthetic duration should also be considered in the planning of the list. It has been reported that anaesthetic time can be underestimated by up to 31 minutes, which led to operations taking 167.5% longer than the anticipated time.14–16
Our study aims to evaluate the differences in operative time between orthopaedic trainees and orthopaedic consultants, as well as provide realistic timings for each stage encompassed within the entire duration a patient is in theatre.
Methods and Materials
We performed a retrospective analysis of prospectively collected data on seven JCST mandatory Orthopaedic trauma procedures performed in our Trauma Unit over one year. The JCST procedures evaluated were dynamic hip screw (DHS), Hip Hemi-arthroplasty, Intra-medullary Hip screw (IMHS) fixation, Tibial nailing, Femoral nailing, Lateral fibular ankle plating and Bi-malleolar Ankle open reduction & internal fixation (ORIF).
A cohort of 946 operation records from our electronic theatre database was included in this study. Parameters evaluated were: Individual procedures, patients’ American Society of Anaesthetists (ASA) grading, anaesthetic time, grade of surgeon and the total surgical time. If the operating surgeon is a consultant, this was noted as such and operating surgeons of Specialists Registrars level (ST3+) were identified as trainees.
Statistical analysis
To analyse the difference in duration taken by both consultants and trainees to perform certain operations, we used a two-tailed Student t-test for unequal variances. A p-value of <0.05 was considered significant.
Results
Of the cohort of 946 operative procedures, a little over half of them were performed by trainees (54%) while the remainder were performed by consultants. Majority (80.4%) of the procedures performed during the study period were hip related (DHS, intramedullary hip screws & Hemi-arthroplasty). To improve accuracy in statistical analysis, the numbers of procedures in the consultant and trainee groups were equalised by random selection. Furthermore, the set-up time is added to the surgical time prior to statistical analysis (Table 2).
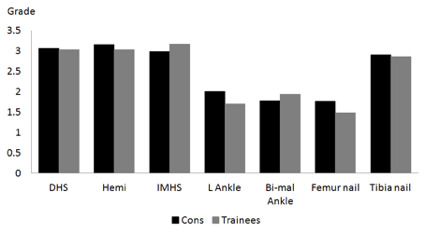
The approximate ASA grading of patients operated by trainees was approximately 2.45, with no significant differences in those operated by consultants (see Figure 1). Patients who underwent hemiarthroplasty had the highest ASA grading at a mean of 3.05, whilst the patients who underwent femoral nailing and ankle ORIF procedures had the lowest ASA grading (1.5 -2).
The mean total operative duration (from commencement of anaesthetic to transfer out of theatre) was found to be the shortest with Dynamic Hip screws (107.4 min), of which 55% was the actual surgical duration. The mean total operative time for diaphyseal femoral nailing was found to be the longest (173.7 min). The anaesthetic duration for both aforementioned procedures was about 30 minutes (Table 2).
To evaluate the differences in the surgical times between consultants and trainees, the set-up times were added to the surgical times and get accurate results for the surgical time difference between trainees and consultants. An equal number of operations from both groups were statistically analysed. It is understood that set-up is influenced by the operating surgeon as well as the surgical time. Therefore, to get realistic, factual results, the set-up time was added to the surgical time for comparison. Set-up time & surgical time were found to be shorter in DHS & Hemi-arthroplasty with consultants as first surgeons (see Table 3).
Discussion
One of the key factors by which a hospital’s success is judged is the number of patients it can serve within a given period. This commonly involves the number of operative cases that can be completed on a particular theatre list. This often puts a lot of pressure on the surgical department due to the expectation of service provision. This creates a dilemma of achieving a balance between service provision and training opportunities.17,18
Furthermore, there tends to be a large focus on the duration of individual surgical procedures and less recognition is given to the other components of an operative list, such as transfer time, anaesthetic time and turnover time.19–22
Our study has attempted to present an objective analysis of operative times for common Orthopaedic Trauma procedures. Knowledge of the operative duration for these procedures when either a consultant or a trainee is the primary surgeon can allay the generalised notion that trainees always take a significantly longer duration to operate in comparison to consultants.23
More recently, “list planning” has been introduced as a mandatory component of the higher surgical training interviews for Orthopaedic trainees in England. Trainees are expected to be conversant in the duration of the components and be proficient in Orthopaedic Trauma list planning.24
To the best of our knowledge, this is the first study that evaluated the real times taken for common Orthopaedic Trauma procedures. Our study revealed that other components of a theatre list, other than the surgical duration, contributed up to 45% of the total operative time in some cases.25,26
This was highlighted and supported as well by the NHS Improvement report in February 2019, “Operating Theatres: opportunities to reduce waiting lists” from data submitted by 92 trusts; it was found that one third of the operating lists lost a whole hour due to late start & early finish. In other words, a whole hour, which is equivalent to the surgical time in some cases, such as DHS, has been lost in roughly one-third of the operating theatres due to poor theatre planning.27,28
It is estimated that the lost theatre time can make as little as 19,000 more Plastic operations or as high as 57,000 more Orthopaedic operations. Having mentioned that, better theatre planning can improve theatre efficiency and this can in turn enhance training opportunities for Orthopaedic Trainees whilst still maintaining appropriate service provision.29 Our study also shows a high ASA grading in patients operated by consultants, but the differences in the grading compared to the patients in whom the Trainees were the primary surgeons were not found to be statistically significant. Higher ASA gradings were expected to be found in patients who underwent hip procedures and this could be explained by the frailty and falls of the elderly population group, in contrast to, say, the ankle fracture group, which happens in younger age groups as well.30
Another interesting finding is that the duration of intramedullary nail fixations is commonly underestimated; our study shows that the surgical duration for these procedures can be up to 2 hours. Of the 7 JCST mandatory procedures, no significant differences in operative times between trainees & consultants were found in 5 procedures. However, significant differences were found in the other 2 procedures (DHS & Hemi-arthroplasty).
In the hip procedures (DHS & Hemi-arthroplasty), the duration of surgery was found to be 15 minutes quicker when Consultants were the primary surgeons. Our data is similar to the results of a study, assessing the difference in operative time and outcome only in Total hip replacements; despite having a similar significant difference in operative time between trainers and trainees, a similar complication rate was observed. That study also concluded that performing a total hip replacement by a trainee is equally satisfactory in terms of outcome to that of a consultant.31,32 On closer analysis of our data, more than two-thirds of hip procedures were performed by Orthopaedic specialist hip Consultants, which could be a contributing factor to the time difference as well.
Limitations
Complex procedures tend to require longer operative times. However, the complexity of each procedure was not assessed, which may have influenced operative durations for two primary reasons. First, the complexity of individual procedures and the intraoperative challenges encountered are not consistently documented by the operating surgeon in the operative notes. Secondly, the surgical logbook does not specify the recording of case complexity.
Furthermore, we were unable to match the exact number of procedures performed (e.g., intramedullary nails); as such, discrepancies in the number of cases across procedural groups may have affected the resulting p-values.
Finally, the level of trainee seniority was not considered in the analysis. It is recognised that more senior trainees are typically expected to possess the skills and experience necessary to complete procedures in a shorter duration compared to their more junior trainees.
Conclusion
Our study provides realistic times for different components of an operative list. This will be beneficial for list planning and consequently a more efficient use of theatre time. Moreover, this information will be useful to more junior trainees who are not yet conversant in planning an operative list.
Furthermore, our study demonstrated that for the majority of the procedures evaluated in this study, the differences in operative times were not statistically significant. Moreover, we did not find a trend towards increased postoperative complications in patients operated on by trainees compared to consultants, although this was not critically analysed in this study.
Our study will also hopefully bring about some reassurance that productivity is not adversely affected if a trainee is the primary operating surgeon in an operative list. To the best of our knowledge, this is the first such study evaluating the operative times in these Orthopaedic Trauma procedures.
Authors’ contribution
Herbert Gbejuade: Conceptualisation, Data collection, Data analysis and article write-up
Mira Odeessa Pereira: Article write-up and manuscript submission
Conflict of interests
The authors declare no potential conflicts of interest.
Funding Statement
No external funding was received for this study.
Acknowledgements
None