Introduction / Background
Complex tibial plateau fractures (CTPF) in elderly patients can present a challenging dilemma to the surgeon, often with no clear “best” treatment option. In the younger, active patient open reduction internal fixation (ORIF) has been well described,1 with clear guidelines and proven success for articular reconstruction.2 However, post-traumatic arthritis (PTA) is a well-known complication following articular injury. Subsequent surgeries for hardware removal and conversion arthroplasty carry increased risks, including delayed wound healing, infection, and implant failure.1,3–7 Prolonged immobility is associated with increased morbidity and mortality.1,8–11 Furthermore, these injuries pose a significant financial cost to both the individual and health care system.3,12
For those with pre-existing arthritis who sustain CTPF, acute arthroplasty may allow for a quicker recovery, increased mobility, and decreased risk of subsequent surgeries with associated complications.13 A common concern with acute arthroplasty is compromised tibial bone stock requiring the use of higher-cost and complexity revision style implants.14 While revision implants are often needed to achieve implant stability, modern knee revision designs include more diaphyseal-friendly stems and metaphyseal fixation.15
Incidence of TPFs
The incidence of tibial plateau fractures is roughly 10.3 per 100,000 people, with approximately 8% occurring in elderly patients.13,16 Vestergaard et al analyzed the 20-year Danish data on 74,106 knee periarticular fractures (PAF), of which 51% were proximal tibia.17 Overall, PAF treatments varied with 34% undergoing surgery, including ORIF (86%), external fixation (9%), and arthroplasty (5%). Those undergoing arthroplasty were 855 patients who had a mean age of 68 (range, 59 to 76), with 74% being women. The study concluded that women over 51 years of age and patients who had comorbidities had the highest incidences of PAF, surgery for PAF, and the development of PTA following surgery. While ORIF for the distal femur is successful,18,19 there is a lack of consensus regarding acute TKA for tibial plateau fractures. However, several studies show favorable outcomes of arthroplasty for TPFs in well-selected patients.20–26
Arthroplasty Outcomes for TPFs
Sarzaeem et al reported on 30 patients (19 men, mean age 67) with baseline osteoarthritis (OA) who underwent acute TKA for TPFs, including 22 AO/Orthopedic Trauma Association (AO/OTA) type 41B, 5 type 41A, and 3 type 41C.24 The 3-year Knee Society Score (KSS; knee score) was favorable at 90.7, with 28 excellent and 0 poor outcomes. Similarly, Malviya et al reported satisfactory outcomes in a series of 15 proximal tibia fractures undergoing acute TKA.22 Notably, all patients in their cohort were allowed to weight bear immediately. At the 3-year follow-up KSS and SF-36 scores were 90.2 and 37.3, respectively.
When comparing arthroplasty to ORIF, Abdelbadie et al compared 22 acute TKAs with 21 ORIF for TPFs and found that acute TKA resulted in improved knee range of motion (ROM), higher KSS and knee function scores, earlier weight-bearing, and a lower complication rates.21 The authors recommended a stemmed tibial component for elderly patients.21 Tapper et al conducted a systematic review of 16 studies with 197 patients (mean age range 68 to 86 years) assessing acute TKA for TPFs.23 They reported a complication rate of 6.1% and revision rate of 3.6% at 4-year follow-up. By contrast, they noted, patients who underwent conversion TKA for PTA following ORIF experienced much higher complication (20-48%) and revision rates (8-20%). The authors concluded that while acute TKA for TPFs may have a higher complication rate than elective primary TKA, the risks remain lower than reported complication rates for conversion TKA after ORIF.23
Post-Traumatic Arthritis and Conversion Arthroplasty
Post-traumatic arthritis is a well-known complication following treatment of TPFs with either ORIF or nonoperative management. It is also an established risk factor for numerous complications following TKA. Wasserstein et al reported a 7.3% 10-year risk of subsequent TKA for PTA after TPF, with an odds ratio (OR) of 5.3 when compared to a matched cohort.27 Performing arthroplasty for PTA poses several challenges including prior incisions, scar formation, malunion or nonunion, arthrofibrosis, and the frequent need for hardware removal. Additionally, these cases present a higher risk of deep infection, aseptic loosening, stiffness, and wound complications.1,7,15,28 In a study by Bala et al, TKA for PTA had a higher incidence of periprosthetic joint infection (PJI) (OR 1.72), cellulitis/seroma (OR 1.19), wound complications (OR 1.80), and revision (OR 1.23) compared to elective primary TKA.6 Houdek et al also noted that PTA was associated with a 25% risk of revision at 15 years.5 Furthermore, Lunebourg et al described a 19° decrease in knee flexion following TKA for PTA from all PAF when compared to TKA for OA.12
Stake et al evaluated a matched cohort of patients undergoing conversion arthroplasty comparing 1640 elective primary TKAs for OA with 823 ORIFs for PAFs converted to TKA (53.4% TPF conversion to TKA).4 At 2 year follow-up the conversion cohort had significantly higher all-cause revision rate (5.47 vs 2.45%), PJI (4.74 vs 1.34%), and periprosthetic fracture (1.58 vs 0.55%). Kester et al also reported longer operative times, more transfusions, more surgical site infections, and higher readmission rates following conversion arthroplasty.29
Implant Survivorship
Short and midterm data demonstrates favorable implant survivorship after acute TKA for TPFs, however long-term studies are lacking.20,26 Ebied et al evaluated a cohort of 25 patients treated with arthroplasty for TPF finding no radiographic signs of implant failure at 6-year follow-up.20 Similarly, Tapper et al studied 22 patients undergoing TKA for TPF (Schatzker II-VI), with mean follow-up of 19 months, showing a high survivorship with two revisions (arthrofibrosis and PJI).26
Economic Considerations and Cost-Effectiveness
With an increased focus on value-based health care initiatives, consideration of relative costs affixed to various treatments remains important.30 Yayac et al reported that conversion TKA incurred greater 90-day post-acute care costs ($4,714) compared to primary TKA for OA ($3,759), with conversion TKA presenting an independent risk factor for readmission and complications.3 A large Belgium study in 2022 included 36,087 patients looking at cost analysis of tibial plateau fractures and determined the main driver of cost is length-of-stay.31 Therefore, when evaluating the value of acute TKA versus ORIF, it is critical to consider the often exorbitant cost of advanced rehab care, complications, and secondary procedures.
Methods
A PubMed search was used to compile relevant literature. Emphasis was placed on studies reporting acute primary arthroplasty (performed at the time of initial fracture management) and comparative outcomes with traditional open reduction and internal fixation (ORIF) strategies. Relevant information was extracted and synthesized to highlight key themes, including patient selection criteria, surgical approaches, implant choices, functional outcomes, and complication profiles.
We included original research articles, case series, review articles, and expert opinions that addressed the indications, techniques, outcomes, or complications of acute TKA for tibial plateau fractures. Studies focusing exclusively on delayed or staged arthroplasty were excluded, as were articles not available in English or lacking sufficient clinical detail.
Literature findings were interpreted with expert clinical experience to highlight practical considerations for these specialized cases.
Evaluation of the Acute Tibial Plateau Fracture
Clinical Assessment
The initial workup of acute TPFs should note the mechanism of injury, associated injuries, and previous knee pathology. Clinical exam may reveal tenderness, swelling, ecchymosis, effusion, and/or deformity.
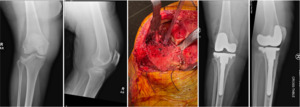
Imaging
Routine orthogonal knee radiographs must be obtained for adequate fracture classification and management planning. A ‘traction view’ can be beneficial if significant comminution and impaction hinder fracture evaluation. Contralateral knee films may be useful for pre-operative planning and templating by characterizing the native joint line and limb alignment. Ultimately, a computed tomography (CT) scan should be obtained for definitive treatment planning. Particular attention should focus on bony fragments with critical ligamentous or tendinous attachments, including the tibial tubercle, fibular head, and medial tibial meta-diaphysis.
Classification
Whether planning for ORIF or TKA, a clear understanding of the fracture pattern is essential for appropriate management. Traditionally, the Schatzker (Table 1) and AO/OTA Foundation (Table 2) classifications have been used to plan ORIF.32,33 The Schatzker classification identifies condylar involvement, articular depression, and metaphyseal involvement. The AO/OTA Foundation classification, more commonly used for educational and research purposes, identifies additional variations.
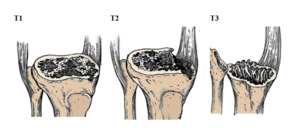
The Anderson Orthopedic Research Institute (AORI) classification (Table 3/Figure 1) provides a useful foundation when planning joint reconstruction for TPFs.1,34 It is traditionally used in revision TKA to assess bone loss, identify structural defects, and anticipate the extent of fixation and constraint required. While not designed for TPFs, the AORI classification encompasses the essential defects one may encounter in these cases. The Schatzker and AO/OTA classifications remain helpful for initial TPF characterization, while the AORI classification becomes useful in arthroplasty surgical planning.
Total Knee Arthroplasty for Acute Tibial Plateau Fractures
Indications for Arthroplasty
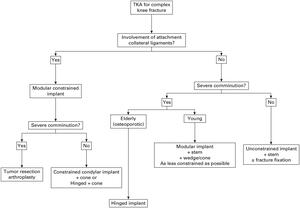
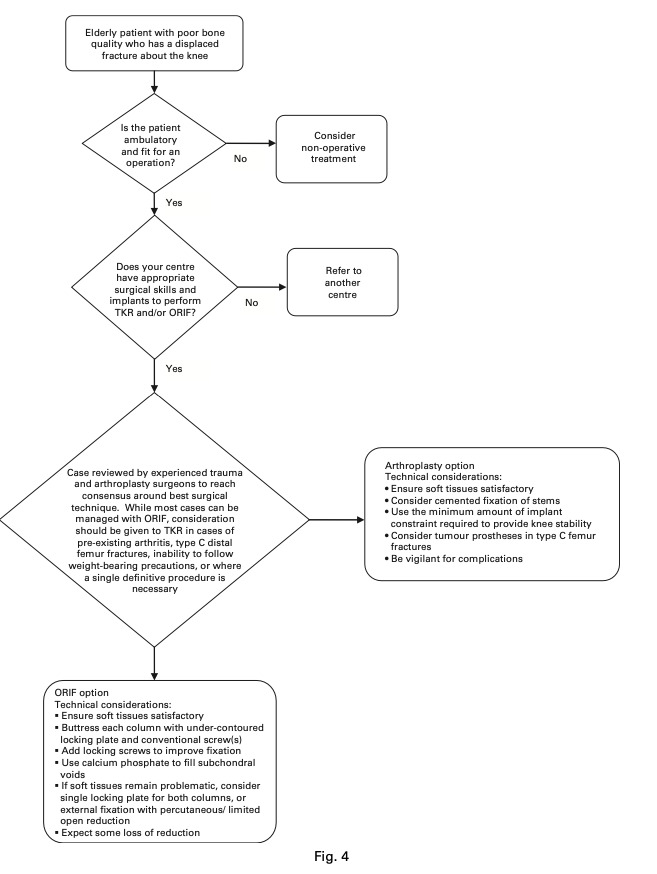
Knee arthroplasty following TPF begins with careful fracture assessment and determination of appropriateness for arthroplasty based on pre-existing patient attributes. The essential considerations include fracture pattern, baseline functionality and comorbidities, hospital resources, surgeon comfort, and previous knee pathology.35 Bohm et al suggested several relative indications, including pre-existing arthritis, inability to follow weight-bearing precautions, or heightened need for a single definitive procedure.36 The authors developed an algorithmic approach to treatment decision-making with consideration for essential hospital resources and recommending transfer if unable to accommodate the complexity of the case (Figure 2).36 A comminuted TPF in the active elderly osteoporotic patient with a history of symptomatic degenerative joint disease is the prime indication favoring acute TKA over ORIF.35 Relative contraindications to acute TKA include active infection, gross extensor mechanism compromise, and open fracture.
Acute Perioperative Optimization
Once acute TKA is indicated as an appropriate treatment option, the goal shifts to expedited perioperative optimization. Assessing modifiable risk factors and optimizing chronic diseases, while paramount prior to elective TKA, has also demonstrated success in the acute setting. Preoperative education, including in-person classes and care partner involvement, have undoubtedly optimized the patient experience, reinforced patient expectations, and reduced readmissions in elective arthroplasty.37 When planning acute TKA for a TPF, expedited patient and family education should be provided, detailing the procedure and typical convalescence. A multidisciplinary approach can safely and expeditiously address key risk-factors including blood glucose, anemia, nutritional status, and cardiopulmonary health. Standard PJI prevention strategies such as diligent aseptic technique, appropriate timing of perioperative antibiotics, and intraoperative hemostasis should be followed. Finally, timely coordination with hospital therapists and care coordinators will help develop a patient-appropriate discharge plan.
Implant Options
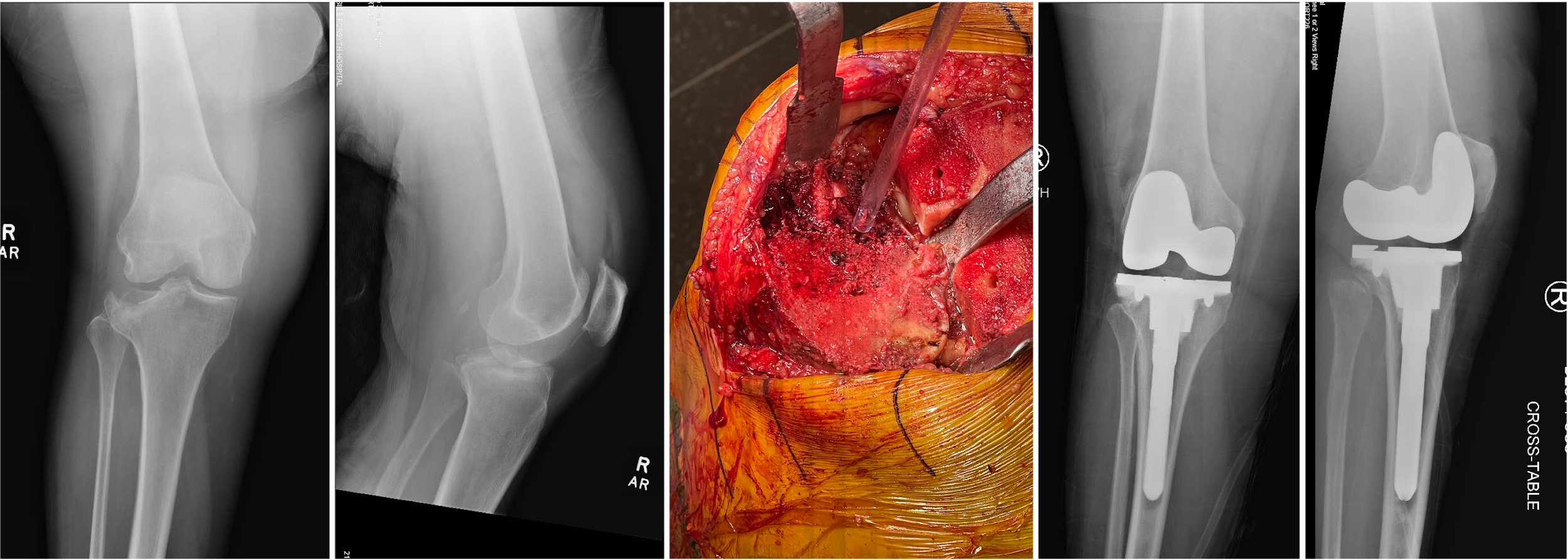
Most modern TKA implants follow a limited set of philosophical principles and biomechanical classifications. However, cemented and hybrid fixation is recommended for acute TKA due to the tibial bone disruption.38 Additionally, while posterior cruciate ligament retention remains a popular technique in elective TKA, the authors advocate for a cruciate-sacrificing approach, which allows for increasing levels of constraint as needed. Revision-style tibia implants are recommended for the same reason; however, primary components can be considered for the femur when minimal constraint is indicated (Figure 3).
Implant Position
Appropriate implant positioning requires a multiplanar assessment, including the transverse plane, proximal/distal placement, and rotational alignment. In addition to adequate medial/lateral implant-bone conformity, avoiding both overhang and impingement, the transverse plane also brings attention to the anteroposterior position. Reestablishing the posterior condylar offset remains critical for flexion stability. Conversely, notching the femur or “overstuffing” the patellofemoral compartment should be avoided.39
Maintaining appropriate position during reconstruction also requires reestablishing the joint line. The joint line is important for optimizing both sagittal kinematics and patellofemoral tracking.40 Raising or lowering the joint line results in relative patella baja or alta, respectively. Additionally, joint line deviation can lead to instability, quadriceps malfunction, anterior knee pain, and decreased ROM.41 Important intraoperative references to reestablish the joint line include the meniscal rim, 2.5-3 cm distal to the medial epicondyle, and/or 1-1.5 cm proximal to the fibular styloid among others.42
Finally, appropriate component rotation will optimize ROM, stability, and patellofemoral mechanics. Internal rotation of the tibial or femoral component, for example, can result in patellar maltracking with possible subluxation or dislocation.43 The medial third of the tibial tubercle, or “floating the tibia”, are useful intraoperative references to help achieve tibial positioning, whereas the posterior condyles and/or the transepicondylar axis provide a useful landmark for femoral rotation.44
Implant Fixation
The second technical consideration is implant fixation. Most revision implants are fully cemented or secured through “hybrid” fixation (the epiphyseal interface is cemented and the attached stem remains cementless).38 Cementless stems require thorough reamer preparation and adequate cortical engagement. Varying offset couplers or stems are readily available to maintain appropriate tray positioning in the transverse plane while achieving favorable diaphyseal stem engagement. Modular tibia step-augments, affixed to the main component, may reconstitute large defects in the medial or lateral tibial plateau. Utilization of augments is typically advised when the defect is 5 mm or greater from the anticipated tray position.45
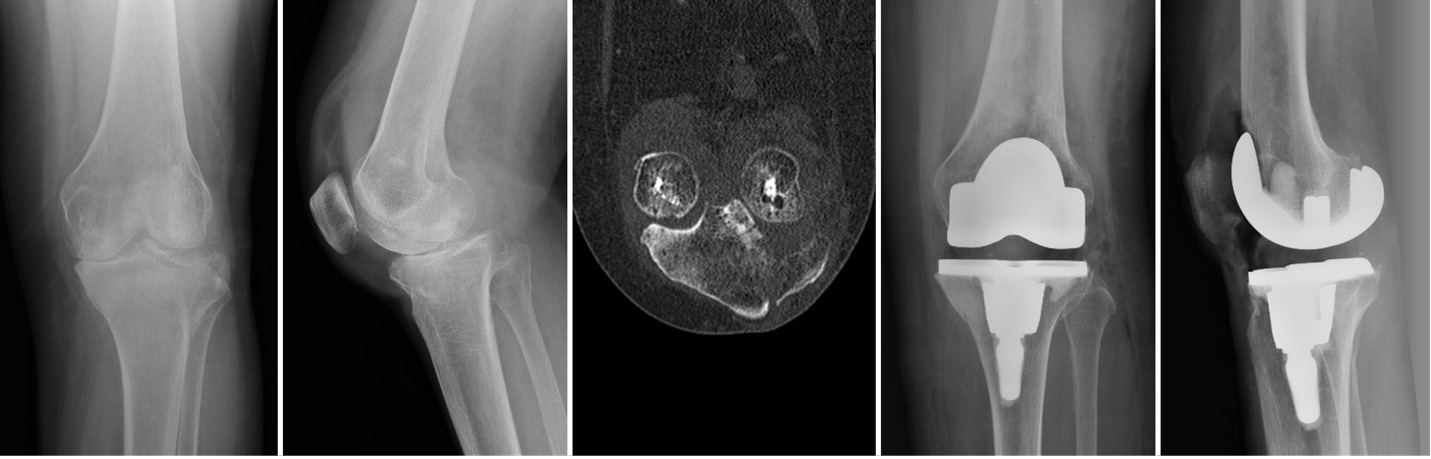
Zonal fixation has gained significant popularity in the last decade, which highlighted the anatomically available, yet structurally underutilized, metaphyseal region. Morgan-Jones et al illustrated the importance of obtaining adequate revision component fixation in at least 2 of 3 tibial zones (epiphyseal, metaphyseal, and diaphyseal) (Figure 4).46 By definition, the epiphyseal zone has been compromised in a TPF, requiring fixation in the remaining two zones (Figures 5, 6). Sleeves and cones offer surgeons a useful option to achieve zone 2 (metaphyseal) biologic implant fixation (Figure 7). Sleeves are traditionally secured to the main implant by a taper fit, while cones are affixed to the implant using cement. Metaphyseal fixation provides important structural support to bridge or bypass the bony compromise and remains a key component in addressing TPFs with TKA.
Stability
The final technical consideration involves achieving implant stability. Stability has traditionally been defined as condylar liftoff of no greater than 2-3 mm throughout ROM with applied coronal forces, and anterior/posterior drawer translation less than 5 mm.47,48 In revision TKA, adequate soft tissue balancing often requires competence of numerous soft tissue structures to avoid instability, including the medial collateral ligament (MCL), lateral collateral ligament/tendon complex, posterior capsule, and extensor mechanism.49,50
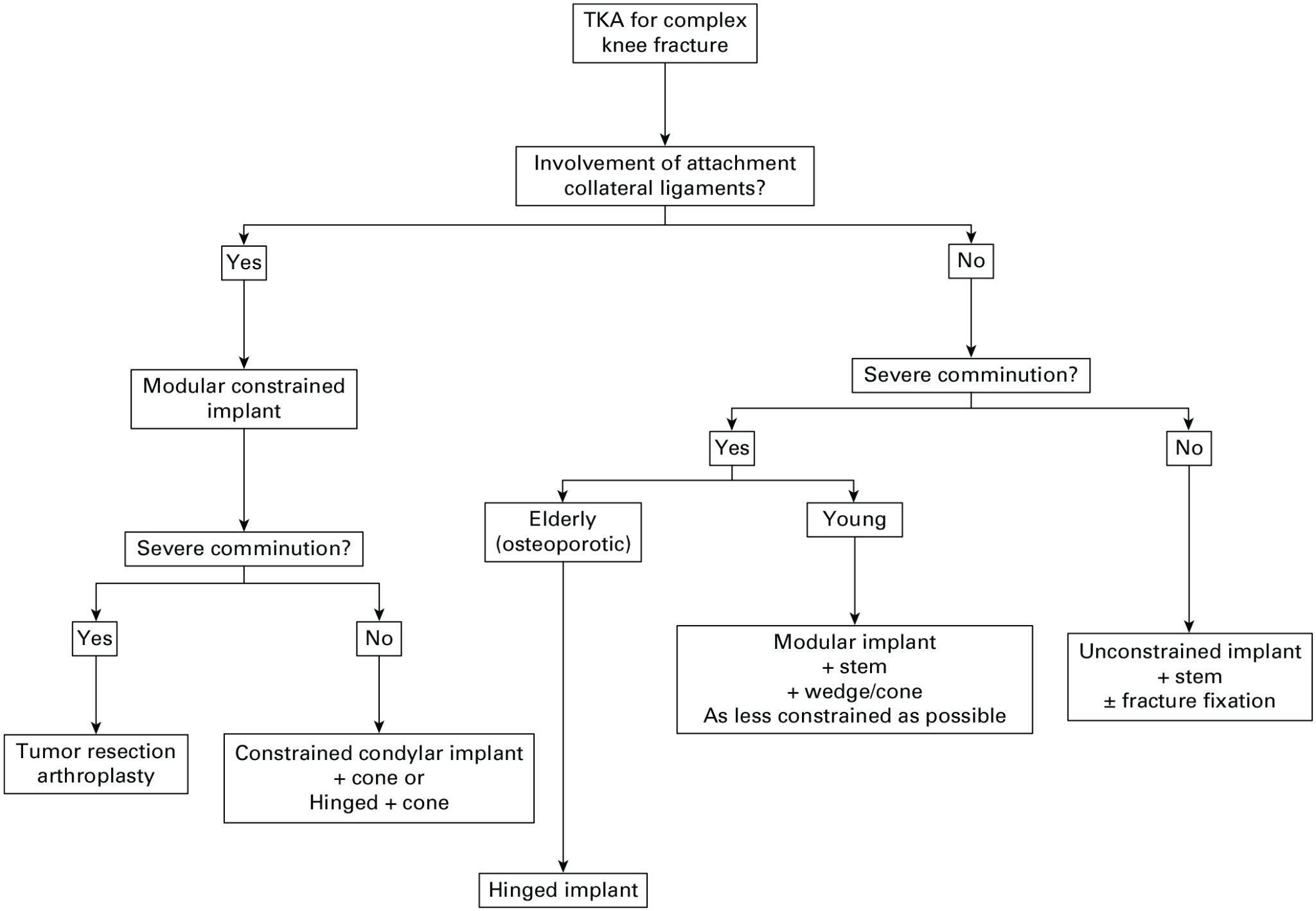
Compromise of the soft tissue envelope often demands additional constraint beyond the traditional posterior-stabilized (PS) design, with consideration for a mid-level coronal constraint or a varus-valgus multiplanar constrained polyethylene.51 These polyethylene options offer varying sized posts engaging the femoral box and cam mechanism. However, in cases of complete ligamentous compromise, notably the MCL, a fully constrained rotating hinge design is necessary. Tampere et al provide a helpful algorithm for choosing appropriate levels of constraint based on specific clinical scenarios (Figure 8).35
Authors Preferred Technique for Acute Arthroplasty in the Setting of TPF
All patients are positioned supine on the operating table using a sliding leg holder, allowing full extension and hyperflexion. A thigh tourniquet is placed and inflated to gravity until cement is cured. A standard medial parapatellar arthrotomy is performed for most cases, however a lateral arthrotomy can be considered when planning supplemental plate fixation for lateral plateau fractures. Following routine knee exposure, provisional fracture reduction with or without supplemental fixation is recommended. Initial reduction, when required, is typically accomplished using a combination of reduction tenaculums, key elevators, and Kirschner wires or Schanz pins. Supplemental screws, plates, and/or staples may help maintain reduction during knee preparation, however they are not typically required. Restoring the bony joint line, thus bringing the fracture to “length,” will provide reference for implant position while also offering improved bony implant coverage.
Following the standard distal femur cut, both the posterior condylar axis and transepicondylar axis are referenced for appropriate rotational position. We have found that performing all femoral cuts first provides improved visualization of the tibia defect for reduction purposes and minimizing retraction forces required to the already compromised bone.
Tibial preparation will set the foundation for the TKA.The proximal tibial cut is made using an intramedullary reamer/guide with the goal of reestablishing the native joint line, with the cut traditionally referenced 2-4 mm from the medial plateau or 8-10 mm from the lateral plateau.52 Preparation for the augments may be performed at this time based on the fracture pattern. Metaphyseal fixation with either cones or sleeves is recommended for all cases and also prepared at this time.
Once tibial preparation is complete, the meniscus and any posterior osteophytes are removed, and the trial components placed. Evaluation of ROM, stability, and patellar tracking is completed using a PS trial. Flexion-extension mismatch typically demands femoral cut adjustment, while symmetric instability or stiffness should focus on tibia adjustment.53 Finally, patella tracking should be critically evaluated, where significant tilt or subluxation likely indicates component malposition which may require adjustment.54 Implants are then assembled and fixed using the hybrid fixation technique. Patients then undergo routine physiotherapy evaluation and are encouraged to begin weight bearing as tolerated using a front-wheeled walker, without restrictions.
Limitations and Future Direction
This is a review article based on retrospective data, case series, and expert opinion. While TKA for acute TPFs holds promise in carefully selected patients, research remains limited to retrospective data and case series reports. Additional research is warranted to further clarify the ideal indications, techniques, and perioperative management. Additionally, larger studies will provide meaningful data quantifying relative risks of infection, loosening, and instability, when compared to primary TKA. These should include prospective studies that investigate long-term outcomes of this approach in clinical practice. However, any prospective randomized-control trial evaluating ORIF vs. acute arthroplasty in this vulnerable elderly and post-traumatic patient population may prove difficult.
Conclusion
In select patients following an acute TPF, TKA may at least warrant consideration of or discussion with the patient about other treatment options such as arthroplasty. The ability to preserve joint function with immediate weight-bearing offers a notable advantage compared to ORIF. Importantly, arthroplasty for the acute TPF can decrease morbidity related to extended hospital admissions and prolonged immobility.8 Acute TPF arthroplasty has the potential to reduce hospital length of stay and healthcare expenditures, increase the likelihood for home discharge, and reduce the need for future conversion TKA. High-level studies are needed to illustrate the ideal indications, surgical techniques, and potential pitfalls when choosing arthroplasty in this patient population.
Conflict of Interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding
None
Conference presentations
None



_epiphyseal_reconstr.png)




_epiphyseal_reconstr.png)