Introduction
Physical therapy (PT) has become a foundational component of musculoskeletal injury treatment, particularly for individuals recovering from sports-related trauma.1–3 These injuries, which encompass sprains, strains, dislocations, and fractures, are among the most common causes of temporary disability and healthcare visits among active populations.4 The physical and emotional toll of such injuries can significantly affect quality of life, daily functioning, and athletic performance, making effective and sustainable treatment critical.5,6
PT offers a non-invasive, function-restoring approach that focuses on healing through guided movement, strength training, and mobility enhancement.7 In contrast, many patients rely on pharmacologic options, especially pain medications, for immediate symptom relief. These medications, while effective in managing acute pain, come with known risks, including dependency, tolerance, and adverse side effects.8,9 The growing concern over prescription opioid use has fueled debates about long-term recovery strategies and safe pain management practices.10
Despite the differences between these two approaches, limited data exist comparing their long-term effectiveness from the patient’s point of view. Much of the existing literature focuses on clinical outcomes, often overlooking patient-reported experiences and satisfaction with treatment. However, understanding how individuals perceive the effectiveness of PT versus medication is vital for shaping treatment guidelines, improving rehabilitation adherence, and ultimately enhancing outcomes.11,12
This study aims to bridge that gap by analyzing survey responses from individuals who sustained sports-related injuries and subsequently underwent treatment involving pain medication, PT, or both. By focusing on patient-reported outcomes such as pain relief, recovery duration, and treatment satisfaction, this research adds a crucial perspective to the broader conversation about optimal injury recovery strategies.
Methods
A cross-sectional survey study was conducted with 200 participants who reported having sustained a sports-related injury in the past. Inclusion criteria for the study included being at least 18 years of age, having sustained an injury related to physical activity, and having undergone treatment involving either physical therapy, pain medication, or a combination of both. The survey was administered on a web-based platform. The anonymous survey collected data on injury type, pain levels immediately post-injury (measured using a 5-point Likert scale), treatment types, treatment duration, and perceptions of long-term effectiveness. Responses were statistically analyzed using JMP Pro 15.
Results
A total of 200 individuals responded to the survey. The cohort consisted of 99 males (49.5%) and 101 females (50.5%), with ages ranging from 18 to 88 years. The median age of participants was 36.5 years.
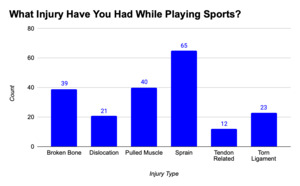
Sprains (33%) were the most frequently reported injury among participants, followed by pulled muscles (20%), broken bones (20%), torn ligaments (12%), dislocations (11%), and tendon injuries (6%). This distribution highlights the high prevalence of soft tissue injuries in sports-related contexts (Figure 1).
Regarding treatment methods, 60.5% of participants reported using both PT and pain medication. Meanwhile, 34.5% used only pain medication, and a smaller portion, 5%, used only PT. This demonstrates that a majority of individuals used a multi-modal approach to injury recovery (Figure 2).
Pain levels immediately following the injury were generally high. Nearly 59% of participants rated their pain as 4 or 5 on a 5-point Likert scale, indicating severe pain at the time of injury. This finding emphasizes the acute discomfort often associated with sports injuries and the urgency for treatment (Figure 3).
The duration of pain medication usage varied. Most participants (61%) used pain medication for up to four weeks: 30.5% for 0–2 weeks and another 30.5% for 2–4 weeks. However, 10.5% of respondents reported using medication for over eight weeks, indicating prolonged usage in some cases (Figure 4).
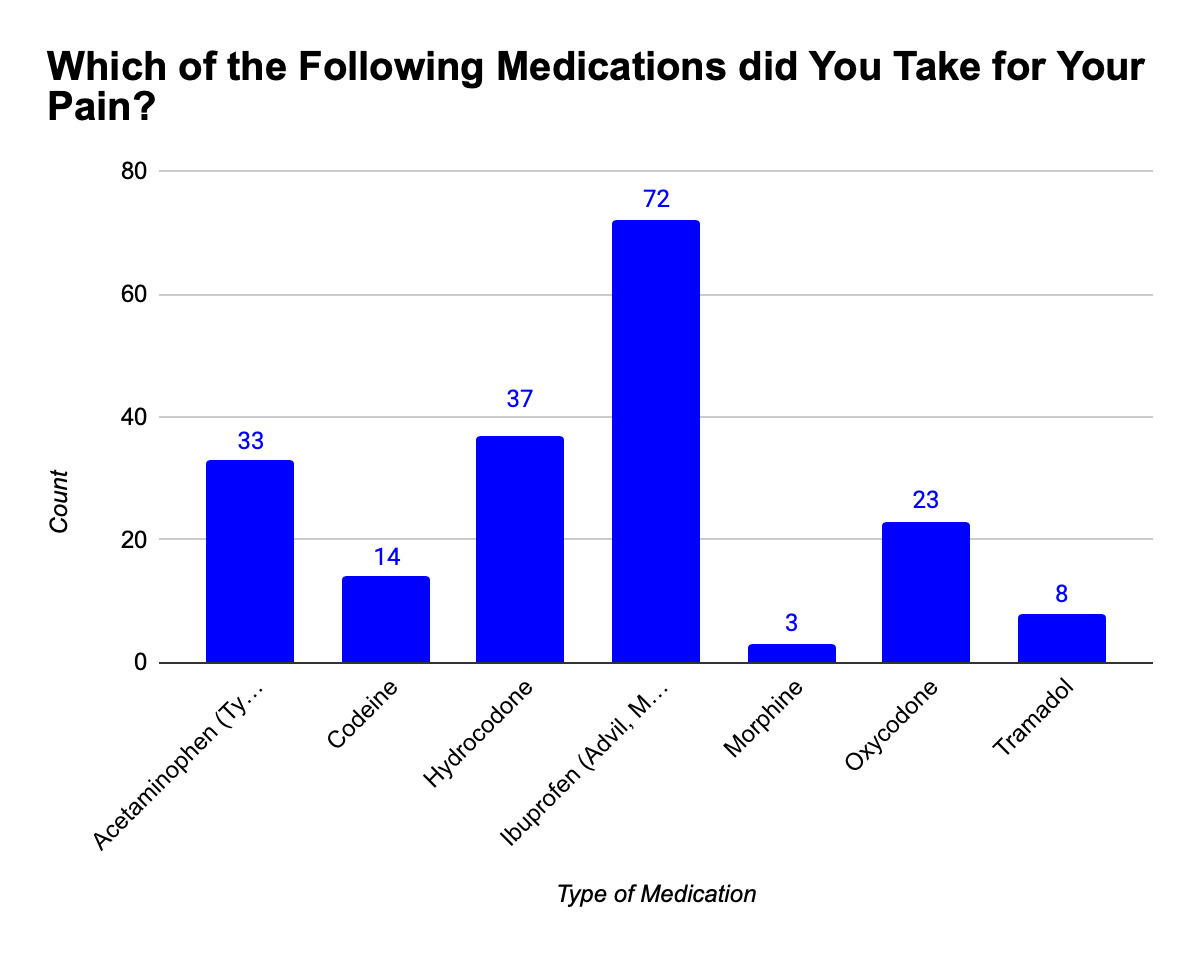
When examining the types of pain medications used, ibuprofen was the most common (37.9%), followed by hydrocodone (19.5%), acetaminophen (17.4%), oxycodone (12%), and others such as codeine, morphine, and tramadol. This reflects a mix of non-prescription and prescription-strength drugs (Figure 5).
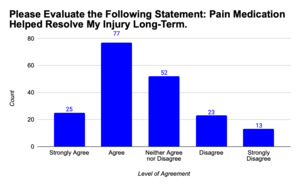
Participants were asked about their perceptions of pain medication’s long-term effectiveness. Only 13.2% strongly agreed that pain medication resolved their injury, while 40.5% agreed, 27.4% were neutral, and the remaining expressed doubt or disagreement. This suggests limited perceived long-term benefits of medication alone (Figure 6).
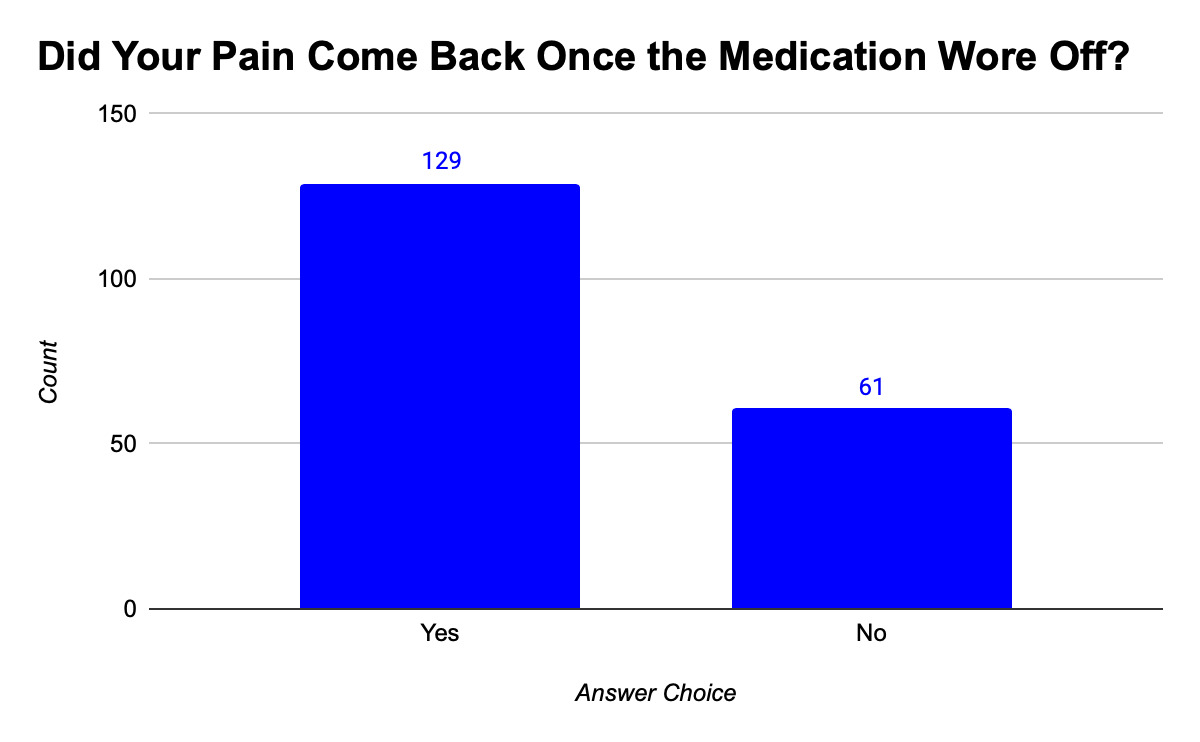
In support of that finding, 67.9% of pain medication users reported that their pain returned once the medication wore off. Only 32.1% experienced sustained relief, indicating that for most, medication provided only temporary symptom management (Figure 7).
Of the entire cohort, 65.5% of participants reported attending PT sessions during their recovery. This reveals a broad acceptance of PT as part of treatment, especially when combined with or following medication (Figure 8).
Regarding the length of PT treatment, 61.1% of participants engaged in PT for four to ten weeks. This relatively extended treatment period reflects a sustained effort toward physical rehabilitation and long-term healing (Figure 9).
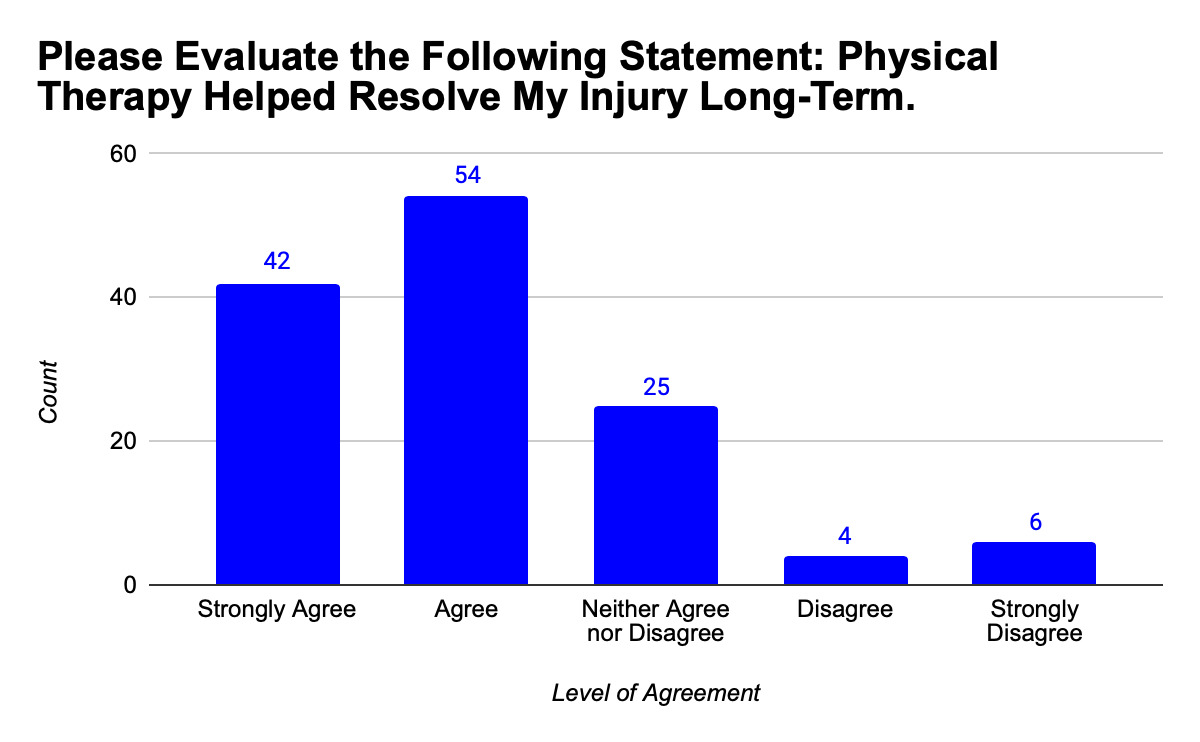
Participant perceptions of PT were largely favorable. Among those who underwent PT, 73% agreed or strongly agreed that it resolved their injuries in the long term. Only a small fraction disagreed or strongly disagreed, demonstrating overall satisfaction with PT outcomes (Figure 10).
Among those who received both PT and pain medication, 68.2% believed that PT was more effective for long-term recovery, compared to 31.8% who favored pain medication. This suggests that when directly compared by individuals who experienced both, PT emerged as the more beneficial treatment (Figure 11).
Discussion
This study contributes to the growing body of evidence supporting PT as a more sustainable and effective treatment modality for sports-related injuries.13 While pain medication offers immediate relief and may be easier to access, it appears insufficient for addressing the root causes of musculoskeletal issues. The high percentage of participants reporting pain recurrence after medication use reinforces this concern.14,15
The study showed participants using PT reported more favorable long-term outcomes. This is primarily due to PT’s ability to target the specific mechanics of injury, improve muscle function, and reduce reinjury risk makes it particularly effective.16 It also avoids the pitfalls of pharmacological treatments, such as side effects and dependency.17,18 Notably, 73% of PT users agreed or strongly agreed that their treatment led to long-term injury resolution, and 68.2% of individuals who used both PT and medication believed that PT was the more effective component.
An interesting finding is the widespread use of multi-modal treatment strategies, with 60.5% of participants utilizing both PT and pain medication. This may reflect a practical approach among patients and providers, especially given the high pain intensity reported immediately post-injury, nearly 59% rated their pain as 4 or 5 on the Likert scale. In such cases, pain medication may play a critical short-term role in facilitating initial comfort and mobility, allowing patients to engage more effectively in physical therapy. However, the prolonged use of medication reported by 10.5% of participants (over 8 weeks) raises concerns about dependency and the need for clear clinical guidelines that prioritize non-pharmacologic strategies once acute symptoms subside.19,20
The specific injury profile observed, dominated by sprains (33%) and muscle strains (20%), aligns with common soft tissue injuries in recreational and competitive sports. These conditions are particularly well-suited to physical rehabilitation, which may explain the high satisfaction rates among PT users. Additionally, the duration of PT engagement, most commonly between four to ten weeks, reflects the long-term investment often required for structural healing and functional restoration.21 These findings suggest that patients are generally willing to commit to extended rehabilitation timelines when they perceive lasting benefits.22
Nonetheless, the study does have limitations. Self-reported data may be prone to recall bias, especially concerning injury severity or treatment duration [24]. The study also did not account for injury severity, comorbidities, or treatment access, which could influence outcomes. Future research should investigate how PT protocols vary in effectiveness by injury type and explore disparities in PT access. Moreover, qualitative research could add depth to these findings by exploring patient motivations, barriers, and decision-making processes around treatment choices.
Conclusion
This study highlights significant differences in perceived long-term effectiveness between PT and pain medication in the treatment of sports-related injuries. While medication provides fast-acting relief, its benefits are often temporary. PT, by contrast, is widely viewed as a more durable and comprehensive solution for restoring function and minimizing pain recurrence.
The findings advocate for increased patient education on the long-term benefits of PT and stronger policy efforts to make PT more accessible, particularly in communities with limited healthcare resources. Encouraging early PT intervention and reducing dependency on medication could not only improve recovery outcomes but also help mitigate the risks associated with opioid use.
In summary, PT emerges from this study as a critical component of effective injury management. Integrating PT more fully into standard care protocols could enhance both individual recovery trajectories and broader public health outcomes.


.png)









.png)