Introduction
According to WHO reports, 10% of men and 18% of women aged over 60 years old have symptomatic osteoarthritis1 and OECD indicators revealed increasing joint replacement rates of about 22% for hip arthroplasty and of about 35% for knee replacement2 between 2009 and 2019.
Due to the limited durability of implants, revision surgery may eventually be necessary, but this procedure poses a significant burden on affected patients.3 Beyond “accidental” indications for revision, such as fracture, dislocation, or infection, implant durability is largely determined by the quality of the bone-metal interface and the progression of osteolysis, which ultimately leads to implant loosening through debris wear mechanisms—the “final event”.4 Therefore, maintaining high standards in implantation techniques is crucial for delaying the need for revision surgery as much as possible. In this context, the importance of joint replacement data collection and analysis becomes evident.
To ensure comparability between studies assessing revision rates, an international committee later developed a set of standardized indicators.5 The primary outcome indicator, as defined in the EUPHORIC project in 2008, was revision for any reason.
Using revision rates for investigating the durability of joint implants, Evans et al. found an overall 15-years survival rate for hip prostheses of 88% while the 25-year rate was 58%.6 They also reported that the selection of articles reporting revision rates longer than 15 years was difficult because of the poor quality and discontinuous follow-up.
Most of the studies investigating implant revision rates focused on long-term durability, whereas no clear definition for early revision is available at the moment. Previous studies investigating early revision surgery used timeframes between 1 month and 5 years7–10 and proposed qualitative definitions of early revision.
Given the significant physical and mental burden of undergoing a second procedure much earlier than expected, it is crucial for all involved caregivers to thoroughly understand the causes behind any “early-than-expected” revision. Therefore, the aim of this review is to summarize the various definitions and underlying reasons for early revisions in the commonly performed total knee and hip arthroplasty procedures.
In particular, we investigated:
-
How frequent is early revision surgery and what is the trend of early revision surgery frequency?
-
What are the indications and reasons for early revision surgery?
-
What are the risk factors for early revision surgery?
Methods
Search strategy
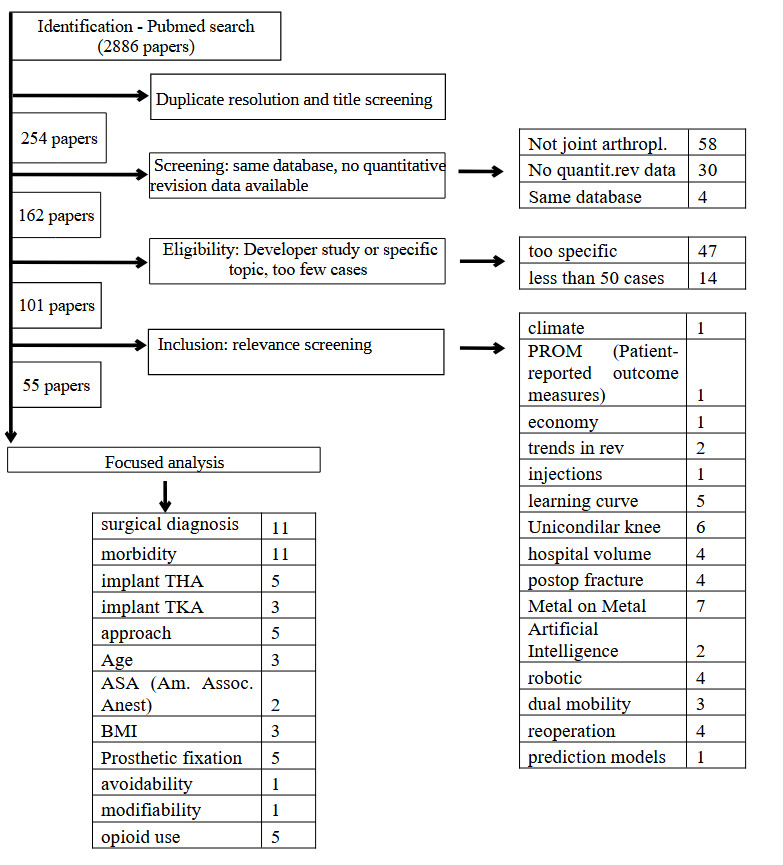
For this review we searched the Medline database using the search terms “early revision” and arthroplasty; “early revision” and “arthroplasty register”, “short term revision” and “arthroplasty”. The search resulted in 2886 references (Table 1). This research was limited between the years 2010 and 2023.
Eligibility criteria
From the 2886 references, only 254 were eligible after a title screening. From these, n=153 were excluded, because of the following reasons:
-
the articles were not related to hip or knee arthroplasty (e.g., other joints, arthroscopy) (n=58);
-
they did not provide quantitative revision data (n=30);
-
they focused on implant system development or specific technical issues (e.g., trunniosis) (n=47);
-
or comprised to few cases (less than 50 cases) (n=14)
Of the remaining n=101 articles, a further quality screening excluded 46 paper, so to not divert away from the primary focus of this narrative review (see Tab.1)
Data extraction
From each of the 55 eligible articles, we extracted its main purpose and evaluated its relevance for our study. From those studies fulfilling these criteria, we extracted quantitative data of revision rates, number of patients, region or registry source, years of primary operation, early revision cut offs, and reasons for revision. Among those, 16 contributions that were more recent and richer in outcome data (e.g., reporting multiple risk factors and/or multiple early revision cut-offs) are summed up in detail in Table 2. Data are summarized from last version online of cited arthroplasty registers. The reported cut-off choices are the typical ones found in literature. They generally reflect the timeframes for outpatients’ postoperative follow-ups.
Data analysis
Data were analysed by comparing overall revision outcome for different reasons. The included articles reported different outcome measures. Those were cumulative rates of revision for majority of contributions. Cumulative revision rates were directly compared, while other forms of result figures could not be harmonized in absence of raw data, but they were presented and discussed (“revisions for 100 component-years”,5 or Odds Ratios11).
Risk factors for early revision included patient- and procedure-related factors. Patient-related factors were divided into “physiological” (e.g., age, weight, sex) and “pathological” ones (e.g., comorbidities or use of drugs) at the time of primary surgery.
In addition, we performed a linear regression analysis of data from six arthroplasty registers in order to compare 10-year vs. 3-months and 1-2-3-5 years cutoff outcomes The sampling period for all register was set in year 2021 (around 6 million THA/TKA cases).
Different revision “cut-off choices” (early, mid, late) were analyzed using data from four articles, which identified time-sequenced outcomes.
This paper does not aim to provide an exhaustive discussion of the complex topic of early, unexpected revisions. Instead, it seeks to systematically present and quantify the intricacies involved. In doing so, we adhere to internationally accepted standards for narrative reviews12
Results
General Trends in revision rates from arthroplasty registers
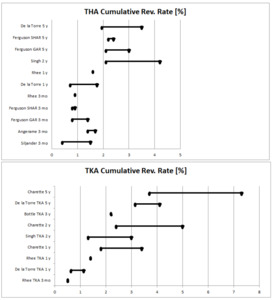
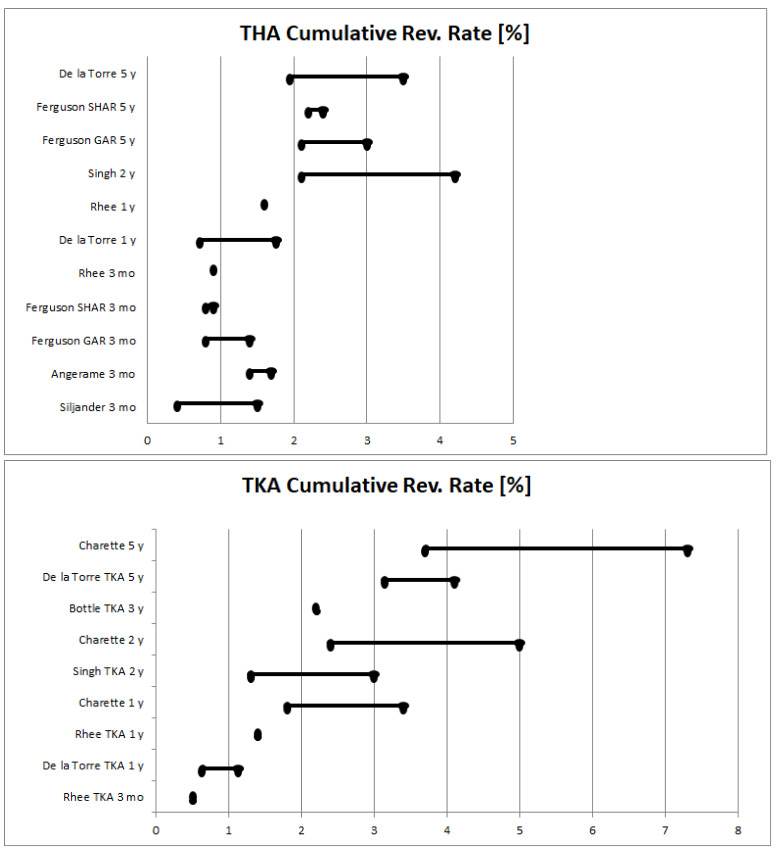
Generally, the reported endpoints for short-term revision procedures are relatively heterogenous ranging from 1 month9 over 3 months9,13–16 and 6 months17 up to 1-year,14,16,18 2-year,7–9,17,19–21 3-year,22 and 5-year7,18,23,24 (Fig.1, Table 2).
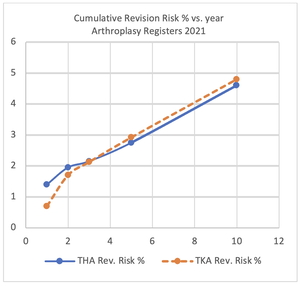
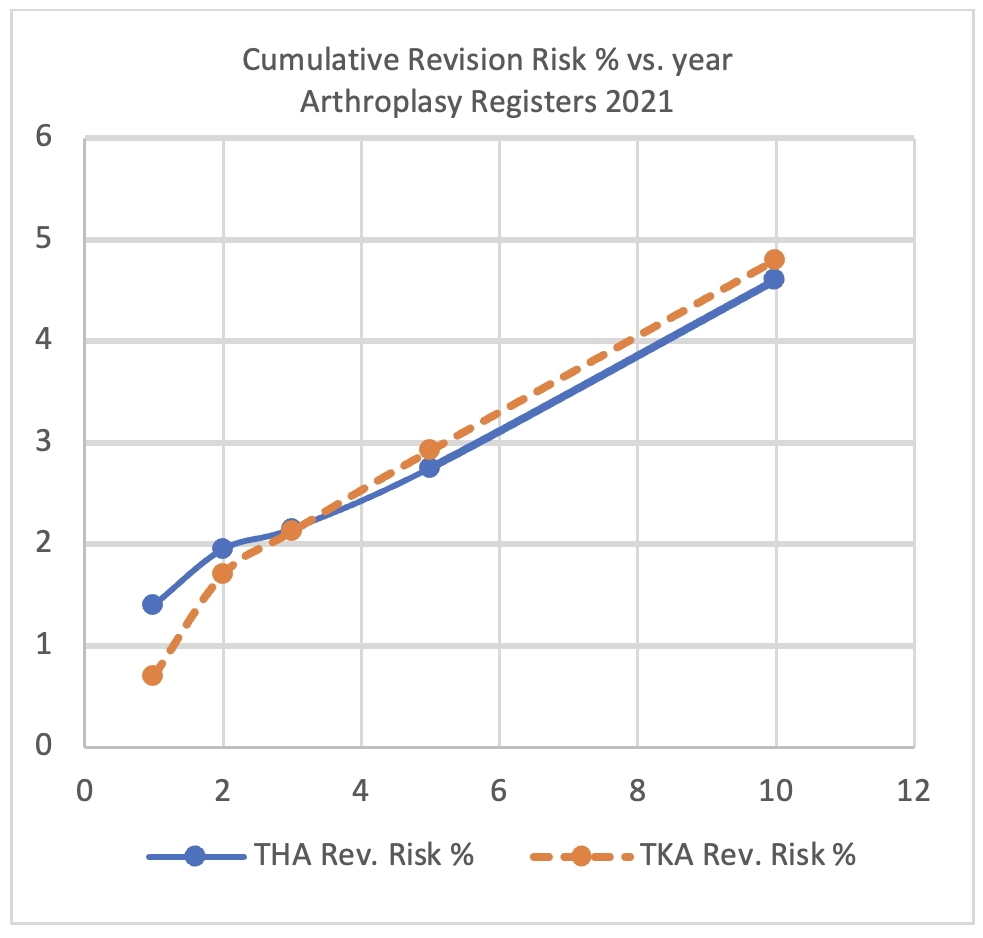
Revision rates evaluated over large data from international registers show a clear change in trends, two years after primary procedure for both THA and TKA (Fig.2).
Arthroplasty registers report revision rates for multiple time frames (1, 3, and 5-year for Australia, New Zealand, UK and Netherlands) while Norway and Sweden report revision rates for 2- and 10-years after arthroplasty (Table 3). As indicated by a steeper slope, the risk of needing revision surgery was greater in the 2 years after arthroplasty than in the following years (Fig. 2). For TKA, the slope estimated from regression analyses decreased from 0.99 (first two years) to 0.38 (time between 2 and 10 years). For THA, the slope decreased from 0.55 (first two years) to 0.35 (time between 2 and 10 years, Fig. 2).
Early revision vs. primary operation year (trend over time)
A total of three studies focussed on trends of early revision over time, covering primary operations performed between 1995 and 2015.
The literature data do not show any consensus about early revision trends over time.
Singh et al.25 reported a decrease in overall 2-year revision rate between 2005 and 2011 from 3.0% to 1.3% for TKA and from 4.2% to 2.1% for THA based on a large Canadian register, while operation volumes increased by about 35 % and 39% (respectively TKA and THA) over the same period of time; Cnudde at Al.9 observed a similar decrease of 2-year revision rates in the Swedish SHAR register between 1999 to 2012 (about 3% to 1.5%). In contrast, Thien et al.17 found on the broader Scandinavian NARA register an increase of early revisions in the years 1995 to 2009; this latter finding was not quantified and refers only to THA femoral periprosthetic revision. The 1-month and 3-month rate showed only a small increase of revision rates in the SHAR database from 2002.9
Indication to early revision
Besides the overall early revision rate, the cause of revision is an important factor too, because revision indications are specific of a particular biological or mechanical event.
Bibliographic contributions show a strong dependence of revision rates on the type of indication and the time at which the revision occurred.
Six of the studies provided data on this issue.8,11,26–29 Of these, three studies on THA focused on 3-months revision rates based on large arthroplasty registers. Cnudde et al.9 reported that 30- and 90-days reoperations are mostly due to infections and that this latter rate, together with the fracture rate, is increasing, while the dislocation rate is decreasing. Ferguson et al.26 reported re-operation and revision data at 3 months and 5-years for each ASA (American Society of Anesthesiology) group. Infection, dislocation and periprosthetic fracture were the main indications for revision while infection, fracture and hematoma were the main indication for re-operation. After adjusting for age, sex and diagnosis, infection was the main 3-months-indication for both re-operation (0.3% of all ASA II procedures, 0.5% ASA II/IV) and revision (0.3% of all ASA I procedures, 0.3% of all ASA II, 1% ASA II/IV).
Singh et al.8 considered not only THA revision indications, but also TKA revisions. Outcomes were grouped as early (2-years), mid (2-10 years) and late (>10 years). This study did not observe a change in the distribution of revision reasons over a period of six years and reported the four most frequent causes for revision. For TKA, these were infections, instability, stiffness, and patella maltracking. For THA, these were infections, aseptic loosening, instability, and fractures. Infections were identified as the main reason for 2-year revisions for both THA and TKA (32% and 39% respectively), with a decreasing trend in mid (2-10) and long term (>10 years).
Procedure-related early revision issues
Implant-related revision risk
Seven studies focused specifically on implant-related reasons. Five of these reported data related to THA17,20,21,30,31 and 2 related to TKA.32,33
Research has evaluated the influence of material combinations and bone fixation methods on early revision rates. Although no particular type of total hip arthroplasty (THA) coupling has shown a definitive advantage, there is strong evidence supporting the use of cemented fixation in elderly patients, where it significantly improves outcomes.
Van Loon et al.20 found an about 50% higher 2-year cup revision rate for press-fit Ceramic on Ceramic (CoC, 0.67%) than for Ceramic on Polyethylene (CoPE, 0.44%) based on the arthroplasty register of the Netherlands. The authors suggested that the reduced quality of bones due to age could result in a higher rate of patients affected from cup migration for the material combination ceramic on ceramic, which precludes sufficient primary stability.
Wyles et al.21 performed a meta-analysis investigating the influence of bearing types implanted in patients younger than 65 years after the year 2000. They found no significant differences between 2-years revision risks for CoC and CoPE (risk ratio for revision=0.65, p=0.5), and between CoC and Metal on Polyethylene (MoPE) (risk ratio for revision=0.40, p=0.34).
Tanzer et al.31 found from the Australian register that 1-month revision rates were about nine times higher for the three best performing cementless stems than for the three best performing cemented stems (HR=5.5 vs 15.1, 95% CI, p=0.001).
Fixation methods are an important factor associated with early revision surgery.34–36 According to the large NARA database (Nordic Arthroplasty Register) database,9 the surgical choice of uncemented fixation increased for THA over the period 1998-2012. Thien et al.17 studied cemented stems in the NARA statistics and reported lower 6-month (0.04 % vs 0.42%) and 2-year revision rates (0.07% vs. 0.47%) for cemented fixation when compared to uncemented fixation.
Khanuja et al.34 recommended cemented fixation in patients aged over 70, for women, for femur form type Dorr C (femur channel type with thinner cortical), and for individuals with osteoporosis. Rationale for that was poorer outcomes of uncemented implants (stem revision rate due to periprosthetic fracture 17% for uncemented vs. 6% for cemented stems).
Springer et al.35 reviewed 10,277 THA procedures in the American Joint Replacement Register (AJRR) and identified 628 early periprosthetic postoperative femoral fractures 3 months after primary surgery. Females over 70 years old are considered at risk, and cementless femoral fixation was associated with a 2.6 times higher revision rate than cemented fixation. This difference was, however, not statistically significant.
Wangen et al.36 also reviewed the NARA (Nordic Arthroplasty Register Association) register and reported that reversed hybrid fixation had a higher revision rate (relative risk of revision=1.4 adjusted for sex, age, diagnosis and time to revision, Cox Analysis) than cemented fixation for patients older than 55 years, three years after primary operation (relative revision risk=3.1 p=0.001).
Revision rates for total knee arthroplasty (TKA) are closely linked to fixation methods. In the study by Papas et al.,37 the authors highlighted that early attempt with uncemented TKA were initially disappointing. However, with a decrease in the average age of patients receiving primary implants and advancements in implant design, uncemented procedures became more favourable. Their research reported a 96.8% survival rate for TKA after 20 years of follow-up, and general better short-term results, with a 99.6% survival rate at the 4-year mark.
Surgery-related revision risks
Seven studies focused on surgery related features for both THA and TKA.15,38–43
This section summarizes the surgical approaches for primary procedures. Although different contributions show statistically significant results, in summary there are no clear advantages of any approach in terms of the number of early revisions.
Silijander et al.15 reviewed different THA surgical approaches. The highest 3-month revision rate was observed for the direct superior approach (1.5%), the lowest for the posterolateral approach (0.4%). The length of hospital stay was found to be significantly shorter for the superior and the anterior approach when compared to the posterior approach (1.7±0.9 days and 1.8±0.9 days vs. 2.3±1.4 days, p<0.001). The frequency of blood transfusion was also found to be significantly different between these approaches (1.8% and 2.1% vs 4.4% of patients).
Yuasa et al.38 found a significantly shorter length of stay and no dislocation events for patients operated with a direct anterior vs posterior approach (23.4 vs. 28.6 days), and higher patient postoperative score (HSS) for the same group (88 vs. 80).
Angerame et al.39 reviewed seven thousand primary THA operations between 2007-2014 and found no significant revision rate differences between the direct anterior and posterior approach. (direct anterior vs. posterior 1.69% vs. 1.39%, p=0.33).
A study based on the Kaiser Permanente US-Register by Sheth et al.42 found no significant differences in septic or aseptic revision rates at 3 years among different approaches, but lower dislocation rates for the direct anterior and anterolateral approaches (HR=0.44, p=0.017 and 0.29 p=0.002 respectively) when compared to the posterior approach.
Meneghini et al. studied 478 THA revisions 5 years after primary surgery. They reported how the direct anterior approach is a risk factor for failure in cementless fixation (50.9% vs. 34.8% lateral and 14.3% posterior, p=0.001), whereas the posterior approach was associated with a higher instability risk (47.5% of all 5-year revision due to instability).
Ravi et al.44 searched for risks of revision for patients who received an injection in the year preceding THA surgery. They found that this group had an increased risk of infection (Hazard ratio equal to 1.37) and revision (adjusted HR 1.53) within 2 years of the primary surgery.
Patient-related early revision issues
Physiological and pathological issues
A total of 29 articles addressed patient related issues.
Those contributions found a strong dependence of early revision outcomes from both physiological and pathological patient status at the time of primary procedure. Several case-mixes are discussed.
Cnudde et al.9 investigated 2-year THA revision rates considering many covariates as ASA scores (American Society of** **Anesthesiologists), the Elixhauser morbidity index, primary indication, sex, age group, but also the time since primary operation. The findings show decreasing death and revision rates over the period under study, while the BMI, the number of comorbidities and the ASA-score of patients increased over the same period in these patients. Three-month overall revision rates ranged between 0.8 % and 2.0 % in the year 2012. The reoperation-rate decreased from 2.0% at 3 months to 0.5 % at 2 years.
Based on data from the Swedish SHAR database, Ferguson et al.26 reported over the period between 1996 and 2016 a 3-months revision rate of 0.8% and a reoperation rate of 0.4 % THA. Association of revision and reoperation rates was positively associated with ASA scores 3-4 (p<0.001 for comparison among all ASA classes). This finding remains statistically significant after adjustment for age, sex, BMI, and diagnosis adjustment.
Bottle et al.22 reviewed UK administrative data until 2014. They found previous all-cause multiple emergency admission as important predictors for 3-years revisions for both THA and TKA (Odd Ratio=1.85 for more than 3 admissions, p<0.001). They also reported significantly greater odd ratios for polyarthritis (OR=1.15), rheumatoid arthritis (OR=1.44), and femur head fracture (OR=1.77) when compared to OR=1 set for the group of THA-patients between 60-64 years old revised after 3 years. For TKA they found significantly greater ORs for patellofemoral (5.16) or partial joint replacement (2.81), and lower socioeconomic status (OR=1.23). An important finding was the higher revision risk for young males (<60), which was attributed to higher dislocation rates (OR=1.19 for THA, 1.24 for TKA).
The combination of relatively “young age” and “male sex” was also found to be a significant risk factor for early revision in 2 other studies .45,46 Cregar et al. found that male patients under 65 years with a BMI over 30 kg/m2 were at elevated risk of revision over 2 years. Gallo et al. performed a cluster analysis on the base of preoperative parameters. The parameters male sex, smoking, and BMI over 30 were associated with higher 2-years TKA revision rates (males under 66 years=10.9% with respect to the whole cohort of 1885 TKA patients). In addition, a high activity level was found as potential contributor to revision risk, albeit this association did not reach statistical significance.
Based on data from the Catalan register database, De la Torre et al.18 investigated the impact of several comorbidities such as obesity, liver disease, anaemia on early THA and TKA revision rates. At 1 year, the authors found revision rates of 2.5% and 3.6 % for THA and TKA across all patients. Having 1 or 2 comorbidities already resulted in a greater risk for early revision at 1 and 5 years for both THA and TKA. The effect of comorbidities on revision risk was, however, lower after 5 years than after 1 for TKA (e.g., obesity, liver disease, deficiency anemia), indicating that comorbidities are more critical in the early postoperative phase.
Rhee et al.14 investigated 3 months and 1-year THA and TKA rates (revision, infection, death) from a Canadian health database. They found overall rates of 0.9% and 0.5% respectively at 3 months and of 1.6% and 1.4% at 1 year. Several diseases were found to be associated with higher odds ratio for infection and revision at 3 months and 1 year after THA and TKA. Diabetes and heart failure increased the odds of infection (3 months: OR=2.0 / 6.1; 1 year: OR=1.2 / 4.8). Blood transfusions and liver disease were associated with higher infection rates for TKA (but not for THA), with OR=1.6 and 3.9 respectively at 3 months.
Dy et al.47 calculated hazard ratios for 5- and 9-year knee arthroplasty revisions considering sex, age, insurance type, education level and hospital volume based on database comprising data from both New York and California. Overall revision rates were 4% (5 years) and 8.9% (9 years). Again, a higher hazard ratio was found for patients undergoing implant procedure before the age of 50 years.
Meehan et al.48 found among the approximately 120,000 TKAs listed in the Californian database between 2005-2019 a 1.8 times higher 1-year revision rate for patients under the age of 50 years. This was explained with fractures and other mechanical failures.
A large review about arthroplasty revision outcomes on patient with diabetes49 concluded that HbA1c level higher than 6.5% can lead to postoperative hyperglycemia, which results in higher rate of infection, thrombosis and death (OR for death=3.23, OR for 30-days postoperative complication=1.22).
Discussion
The objective of this review was to summarize the literature about the frequency, indications, and risk factors for early total knee and hip arthroplasty revision surgery. This review identified numerous studies that mainly relied on data from arthroplasty registers and provided estimations of risk factors for early revision as well as insights into patient- and procedure-related issues. The frequency of revision surgery within 2 years after arthroplasty was estimated to range from 1.5% to 5% for knee and from 2% to 4% for hip arthroplasty.8,50 The majority of revision surgeries took place in the first 24 months, indicating that the risk is greatest in the 24 months after primary surgery. After 2 years, the slope decreased and was continuous until year 10. One study9 reported slightly increasing 1-month and 3-months reoperation and revision rates in recent years, potentially due to a more “aggressive” attitude to early revision indication, whereas the 2-year revision surgery rate decreased over the last decades most. This may be explained with the more aggressive approach to not delay early revisions (“Do it right away”), as delaying early revisions may be detrimental for patients. Still, a considerable percentage of arthroplasty patients need to undergo early revision surgery and this places a significant burden not only on the affected patients but also on the healthcare systems. Singh e al.8 reported the number of early revision surgeries to be approximately constant between 2005 and 2013 despite an increase by >30% in both THA/TKA procedures. The number of patients expected to undergo hip and/or knee replacement surgery is, however, expected to further increase and this may eventually also translate into an increase of early revision procedures.
Whereas late revision surgery is mainly indicated due to loosening of implants or periprosthetic fracture, early revision surgery is primarily indicated due to infection and instability for both hip and knee arthroplasty. Previous studies investigated and identified numerous risk factors for early revision surgery such as high BMI, smoking, and insufficiently treated diabetes but also interactions between some of these factors, such as younger, physically active males45–47 or cementless fixation in older or osteoporotic patients.34,35 Since some of these patient-related risk factors such as high BMI, smoking, or untreated diabetes are modifiable, a significant number of early revisions may be avoided by addressing such modifiable risk factors before hip or knee arthroplasty.19,24 Since some infections may be (partially) due to patient-associated factors like smoking, poor dental health and insufficiently controlled diabetes, the rate of revisions due to infection may potentially be reduced as well. Kee et al. reported that 40% of the early THA and TKA revision cases (before two years after primary implant), have at least one modifiable risk factor. Delaying the primary arthroplasty may be an option in patients willing to lose weight, to stop smoking, or to improve the treatment of diabetes. On this behalf, the gradual shift towards outcome-related health has pushed towards preoperative management of the patient at risk for complications. Orthopaedic departments adopt nowadays best practice pre-admission criteria referring to different risk factors, and possibly activates optimization procedures before primary surgery. Among those, guidelines agreed over strategic parameters like HbA1c values over 7.5%, hemoglobin level under 12 g/dl for women or 13 g/dl for men, serum albumin level under 3.5 g/dl. In addition, postoperative risk factors such as avoidance of intense physical activity during osseointegration, lack of follow-up, or poor postoperative management need to be taken account, in order to reduce the risk of revision in the first months after the intervention.
The literature search used terms like “early” or short-term in order to identify relevant articles. One limitation of this study is intrinsic to the choice of the narrative format. Systematic review strategies reduce risk of bias and of missing data, therefore in our contribution articles may have been missed. The further limitation that “early revision” is not well-defined makes a systematic review on this topic still a difficult task.
The fact that in the focused analysis (Tab.2) six different registers and other four national or regional discharge repositories are present, indicates the need of solid and large databases to assess revision analysis. We consider this a strength more than a limitation. This latter fact also implies the increasing need of larger datasets to assess the complexity of early figures, as demonstrated here.
The time-frames defined as “early revision” in the included studies varied from up to 3 months to up to 5 years and it would be desirable to have a broadly accepted definition of early revision surgery, potentially based on the definition proposed by Singh at al.,8 who suggested to differentiate between early (<2 years), mid (2-10 years) and late (>10 years) revision. In addition, some arthroplasty registers report only 2-year revision rates whereas others report revision rates for multiple time points (1, 3, and 5 years) but not for 2-year rates, which limits the comparability (see table 4).
To this end, we recommend that future research focuses on refining definitions. Consider, for instance, the loosening mechanism: it represents the ‘natural’ service life through mechanical failure. However, we currently lack biomechanical thresholds to determine whether a loosening revision occurs “prematurely” or within an expected timeframe.
Given the large amount of data available in implant registers, it may also be possible to not only stratify risk factors for revision by time-frame (e.g., early vs late) but additionally also by the indication of revision (e.g., percentage of revisions after 1 year due to infection, loosening or fracture) in future studies. This may provide more detailed insights into which and how risk factors affect revision surgery.
Conclusion
Hip and knee arthroplasty come with a considerable risk of early revision surgery. The annual rate of revision surgery was, however, reported to decrease after the first 2 years. The published studies provided data on indications for early revisions, e.g. periprosthetic infection, instability, for both THA and TKA procedures which differ notably from the indications for later revisions such as aseptic loosening or periprosthetic fractures. Numerous studies also investigated the impact of risk factors for early revisions that provide valuable information for reducing the risk of early revision for arthroplasty patients. Patient-modifiable risk factors such as a high BMI, smoking or insufficiently controlled diabetes may be of particular interest in this regard, as these may allow to significantly reduce the risk for affected patients.