Introduction
Avulsion of the anterior cruciate ligament (ACL) is defined as a bony detachment at the ligament’s tibial insertion site.1–3 These injuries occur more frequently in children with open physes than in adults, as the incompletely ossified tibial eminence is more prone to fracture than ligament rupture when subjected to traumatic forces.4,5
The optimal treatment strategy for pediatric ACL avulsions remains controversial, often lying at the borderline between conservative and surgical management.6
To guide clinical decision-making, Meyers and McKeever proposed a widely used radiographic classification system in 1959, which categorizes fractures into four types based on fragment displacement and rotation.7 However, management of intermediate (Type II) lesions is still debated, and each reported case contributes to refining treatment strategies, which rely heavily on clinical evaluation, imaging findings, and accumulated experience.
We present the case of a five-year-old girl with an ACL avulsion fracture successfully treated with conservative management, highlighting the potential role of non-operative treatment in carefully selected young patients.
Case Report
We present the case of a five-year-old girl who was referred to our orthopaedic department after sustaining a fall while playing at school. Following the injury, she was unable to walk and reported acute knee pain.
On clinical examination, diffuse tenderness was noted over the patella, with associated ecchymosis. The patient had difficulty bearing weight and exhibited a limited range of knee motion due to pain. Stability tests could not be performed because of poor cooperation.
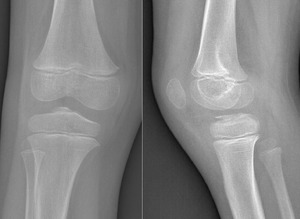
Plain anteroposterior and lateral radiographs demonstrated a bony fragment detached from the tibial plateau at the level of the tibial spine, consistent with a partially displaced, but not rotated, ACL avulsion fracture (Figure 1). The fracture was classified as a Type II Meyers and McKeever lesion based on radiographic features. Magnetic resonance imaging (MRI) confirmed the diagnosis, showing avulsion of the tibial spine with a fragment arising from the tibial eminence, associated bone marrow edema, and soft-tissue swelling. No meniscal tear or intermeniscal ligament entrapment, chondral lesion, collateral ligament injury, was detected (Figure 2).
After multidisciplinary discussion, and considering the absence of concomitant soft-tissue pathology on MRI, a conservative approach was selected. Treatment consisted of immobilization with a long-leg cast in full extension for 30 days with strict non-weight bearing (Figure 3).
At the 30-day follow-up, clinical evaluation showed resolution of pain and a stable knee on examination. Radiographs performed at the same time confirmed satisfactory healing of the avulsion fracture (Figure 4).
The patient was subsequently enrolled in a structured rehabilitation program aimed at restoring knee mobility, reducing post-immobilization stiffness. The program included progressive passive range-of-motion exercises, quadriceps strengthening, proprioceptive training to facilitate joint mobilization and early functional recovery. Improved knee mobility was observed, and the patient was able to walk without assistance.
At the two-year follow-up, clinical examination revealed a stable knee with negative Lachman, anterior drawer, and pivot-shift tests. The patient demonstrated full recovery from the injury.
Discussion
Anterior cruciate ligament (ACL) avulsions, also referred to as tibial spine fractures, tibial eminence fractures, or intercondylar eminence fractures, are rare injuries characterized by a bony detachment at the tibial insertion of the ACL.1
These fractures occur predominantly in children, especially between the ages of 8 and 14, owing to the incomplete ossification of the tibial eminence, which is more prone to fracture than ligament rupture under tensile stress.4
Common mechanisms include forced knee flexion with external tibial rotation, uncontrolled external tibial rotation with the foot fixed, and knee hyperextension associated with valgus or rotational forces.8,9
Because of their rarity, these injuries require careful clinical and imaging evaluation. Meniscal entrapment, chondral damage, or associated tibial plateau fractures are important to identify, as they often necessitate surgical treatment and may compromise healing if left unrecognized.10
Plain radiographs, particularly in the lateral view, are usually diagnostic, but MRI is essential to detect soft-tissue involvement and to better characterize fracture morphology.11
The Meyers and McKeever classification, introduced in 1959, remains the most widely used system to guide treatment decisions. It distinguishes nondisplaced (Type I), hinged (Type II), and completely displaced (Type III) fractures, with Zaricznyj later adding a comminuted Type IV.12
There is general agreement that Type I fractures should be managed conservatively, while Type III and IV fractures usually require surgical fixation.1,3,4,9
The optimal management of Type II fractures, however, is still debated. Many surgeons attempt closed reduction and immobilization first, reserving surgery for cases where anatomic reduction cannot be achieved or maintained.
Differential diagnosis is broad and includes traumatic conditions such as ACL tears, meniscal injuries, tibial plateau fractures, patellar dislocations, and Segond fractures, as well as non-traumatic disorders including osteochondritis dissecans, discoid meniscus, and inflammatory or infectious arthritis.13 Clinical history, physical examination, radiography, MRI, and, in selected cases, laboratory tests are crucial to rule out alternative diagnoses.
Non-operative treatment of nondisplaced or partially displaced tibial spine fractures generally consists of immobilization in extension, which facilitates reduction of the fragment and promotes healing.
For Type II fractures without concomitant soft-tissue injuries, conservative treatment is considered safe and effective, though surgical fixation remains the treatment of choice if displacement progresses.
Type III and IV fractures usually require operative fixation, either open or arthroscopic, with various techniques including screws, sutures, or bone tunnels. Arthroscopy is increasingly favored because it allows simultaneous management of meniscal injuries, accelerates rehabilitation, and reduces stiffness.14–17
Complications may occur with either approach. Malunion, non-union, persistent laxity, and growth disturbances have been reported. Arthrofibrosis is the most common complication following surgical fixation.14–17
In our case, the patient was only five years old, considerably younger than the typical age group for this injury.
The fracture was partially displaced but not rotated, and no associated soft-tissue lesions were detected on MRI.
On this basis, conservative management with casting in extension was chosen. The decision was guided not only by the degree and geometry of the fracture displacement but also by the absence of associated soft-tissue injuries on MRI, which represented a critical element in the treatment strategy. The patient achieved full recovery with no complications, reinforcing the evidence that, in carefully selected Type II injuries, a thorough assessment of both fracture morphology and soft-tissue status can justify a non-operative approach and lead to excellent outcomes, even in very young children.
Conclusion
In conclusion, our case of a five-year-old child with a Type II Meyers and McKeever ACL avulsion fracture achieved full recovery after conservative treatment. The decision was based on careful analysis of fracture morphology and the absence of soft-tissue involvement on MRI, supporting the notion that non-operative management can be a safe and effective option in selected pediatric patients, even at very young ages. This report represents an additional step in refining the surgical versus conservative decision-making process.
Author Contributions
Conceptualization, H.Z. and M.D.; methodology, V.M. and H.Z.; software, V.M.; validation, F.P..; resources, M.D; data curation, M.D.; writing—original draft preparation, V.M. and H.Z. and R.G.; writing—review and editing, I.A.; supervision, F.P. All authors have read and agreed to the published version of the manuscript.
Funding and Conflicts of interest statements
There was no funding source for the manuscript. The authors declared no conflict of interest.


_of_the_knee_confirming_the_diagnosis_of_tibial_spine_avul.png)


_of_the_knee_confirming_the_diagnosis_of_tibial_spine_avul.png)

