1. Introduction
Femoral and tibial shaft fractures are among the most common long bone fractures, often resulting from high-energy trauma such as road traffic accidents or falls from height in the younger population, in the older population these injuries usually occur through low energy mechanisms.1
Surgical fixation with intramedullary nails is widely considered the gold standard treatment of femoral and tibial shaft fractures, given its biomechanical advantages, allowing for early weight-bearing and rehab potential, reduced soft tissue iatrogenic trauma and also high union rates.2
However, the financial burden of stocking an orthopaedic theatre with IM nails can be substantial, stocks must be maintained and in house inventory is influenced by various nail sizes, specialized instrumentation required and also by sterilization protocols.3
Recently, innovative locking rod systems have been introduced as alternative fixation methods for shaft fractures, offering potential advantages in surgical efficiency and also cost-effectiveness. Some of these devices incorporate advanced locking mechanisms and offer intraoperative customizable lengths options which may reduce the need for stocking multiple nail sizes and extensive surgical instrumentation, while maintaining comparable clinical outcomes.4
Despite all the promising attributes of innovative locking rod systems, there is still limited comparative research that analyzes the financial implications of stocking an orthopedic theatre with IM nails versus stocking with innovative locking rods, particularly in high-income settings such as Europe and the United States.
This study aims to assess and compare the economic impact of these two approaches by evaluating: direct costs (implant pricing, instrumentation and operating room expenses) and indirect costs (complication rates and reoperation expenses). By analyzing the financial feasibility of each system, this research seeks to provide evidence-based recommendations for hospital procurement decisions and cost optimization in orthopedic trauma care.
The importance of this study comes from the high impact given by the high volumes of shaft fractures treated in a Level 1 Trauma Centre. A retrospective study in Finland over 6 years (2014 - 2020) treated a total of 1182 patients with femoral fractures by IM nailing, amounting on average yearly to 197 femoral fractures treated by IM nailing. Another retrospective study from Qatar over a period of 4 years treated 454 femoral fractures by IM nailing, averaging yearly to 114 patients treated by IM nailing. On average it can be considered that a Level 1 Trauma Centre would treat 150 patients by IM nailing.5,6
2. Methods
Ethical consideration
This study doesn’t involve human participants, patient data or clinical interventions, because of that it is considered exempt for patient consent requirements. All financial data is anonymized to ensure confidentiality.The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Victor Babes University of Medicine and Pharmacy Timisoara (number 84/01.10.2021 rev 2024).
Study design
This study is a comparative cost-analysis study aimed at evaluating the financial burden of stocking an orthopaedic theatre with IM nails versus locking rods used for the treatment of femoral and tibial shaft fractures. The analysis will focus on the costs associated with the procurement; storage and utilization of these implant systems, using publicly available data, manufacturer pricing and relevant industry reports.
This study is a non-patient-centered retrospective study which used financial data gathered from published cost reports, healthcare procurement databases and data gathered from implant suppliers.
Data collection
Data was gathered from publicly available sources, including national and international procurement databases (such as hospital supply catalogs and public tender documents), public pricing reports and manufacturer published implant cost sheets. This included various sizes and configurations, along with the costs of the supplementary fixation components like locking screws, instruments and guides. Additionally, price variability across different suppliers and manufacturers were considered to reflect market diversity.
Additional data were extracted from peer-reviewed studies including cost metrics for orthopedic implants and operating room expenditures. All sources were selected to reflect generalizable and openly accessible financial information applicable to high-income healthcare systems.
Instrumentation and surgical tool expenses were evaluated by reviewing the average cost of specialized tools required for each implant system, including both reusable and disposable components. Where applicable, tool depreciation and usage, frequency were considered to assess the economic impact of reusable instrumentation.
Operating room costs were analyzed based on the average duration of procedures utilizing each implant system. Staffing expenses were determined by standard hourly compensation rates for surgeons, anesthetists, and nursing personnel, derived from healthcare industry reports.
Storage and sterilization costs were assessed through a review of logistical demands such as inventory space, stock maintenance, and sterilization protocols. The analysis incorporated costs associated with managing both implant systems and reusable surgical instruments.
Lastly, data regarding complications and reoperation costs were derived from existing clinical literature. This included the financial impact of infections, bone nonunion, and the hospital resources required for managing postoperative complications related to each implant type.
The inclusion criteria for data were: publicly accessible reports published between 2018 and 2024, pricing data specifically related to femoral and tibial shaft fracture fixation using intramedullary nails or universal locking rod systems and financial figures related to implant procurement, instrumentation, operating room time, sterilization costs and reoperation costs.
Exclusion criteria included: internal hospital pricing data not publicly disclosed, non-English cost reports, financial data pertaining exclusively to paediatric or upper limb fractures and cost data outside high-income countries, as defined by the World Bank.
Cost Analysis Methodology
The study adopted a cost-analysis approach aimed at quantifying direct expenditures associated with the procurement, surgical application, and post-operative management of orthopedic implants. The direct costs of implants and instrumentation were calculated using average market prices for femoral and tibial IM nails and locking rods, along with related fixation components. Both single-use and reusable items were reconsidered, factoring in depreciation and the frequency of use in a clinical setting.
Operating room and staffing costs were estimated by combining standardized per-minute operational costs of running surgical theaters with average hourly wages for relevant healthcare staff, including surgeons, anesthesiologists, and sterilization cycles.
To evaluate complications and reoperation costs, the study referenced average cost data for managing implant-related adverse outcomes. These included rates of infection, nonunion and subsequent hospital interventions or surgical revisions, all of which have implications for long-term financial burden.
Specific implant considerations
Intramedullary nails are anatomically specific implants, requiring careful selection based on parameters such as diameter, length, and locking configuration. The nail must correspond precisely to the patient’s intramedullary canal and fracture characteristics. This necessity for precision results in the requirements for hospital to maintain large inventories of various implants sizes and types to accommodate diverse patient needs.
Conversely, the universal locking rod system introduces a modular and flexible design that can be adjusted intraoperatively. These systems typically allow for length customization during surgery – often within a range of 250 mm to 400 mm for femoral fractures – and rely on a fixed or semi-adjustable diameter. Locking screw configurations can be adapted based on the patient’s anatomy, making these systems more versatile than traditional pre-sized implants.
Although the term “universal” may suggest a one-size-fits-all approach, these rods are not singular in dimensions. Instead, they offer intraoperative adaptability that significantly reduces the variety of implant stock required. This design not only enhances inventory efficiency but also minimizes the risk of delays caused by mismatched or unavailable implant sizes during surgery. Ultimately, this contributes to smoother surgical workflows and may lower the incidence of implant-related complications.
Statistical analysis
Descriptive statistics were used to present cost-related findings for both implant systems. This included the calculation of mean values, standard deviations, and cost ranges for each major category – implant pricing, instrumentation, operating room costs, sterilization, and storage. Comparative analysis was performed to evaluate total procedural costs using paired t-results for data sets with normal distribution. In instances where normality could not be assumed the Mann-Whitney U test was applied.
For each cost category, independent statistical comparisons were conducted between intramedullary nails and universal locking rods using simulated datasets. Midpoints were calculated as the arithmetic mean of the reported minimum and maximum values for each implant type. Around each midpoint, synthetic datasets were generated assuming a normal distribution with a standard deviation equal to ±20% of the midpoint value, reflecting estimated real world cost variability.
A total of 30 data points per group were generated for each category independently This approach ensured that each cost component , such as implant cost, instrumentation, operating room time, sterilization and complications, was analyzed using a distinct dataset reflecting its specific cost structure. Independent samples t-tests were applied to compare group means. To account for potential abnormal distribution, Mann-Whitney U tests were also performed for each category.
3. Results
Implant and Instrumentation Costs
The cost per implant for IM nails was found to be between $800– $1,500 for IM nails used to treat femoral shaft or tibial shaft fractures with additional costs per surgery for locking screws and single use instrumentation being in the range of $200– $500. In comparison, a universal size locking rod system used to treat femoral shaft or tibial shaft fractures is priced in the range of $1,200– $1,800, with additional costs for screws being reported to be in the range $150– $400.
Operating room and staff costs
Operating room time was measured for each procedure. IM nailing of tibial and femoral shaft fractures ranges in duration between 90–120 minutes, leading to operating room costs of approximately $5,400– $12,000 per procedure (including anesthesia and staffing of the operating theatre). In contrast, the universal locking rod implant procedure for femoral or tibial shaft fractures takes 75–110 min, this resulted in an operating theatre cost amounting approximately $4,500– $11,000 per procedure.
Sterilization and storage costs
Sterilization and storage costs were evaluated for the necessary tools and implants used in each procedure. For IM nails sterilization costs were on average calculated at ~ $5,000– $15,000 for annual sterilization and storage cost per implant type, based on the number of reusable instruments involved and stock quantity. On the other hand, the locking rod system, with a more simplified set of instruments and adjustable design, incurred sterilization and storage costs calculated at $3,000– $8,000 annually per implant type.
In a clinical setting a Level 1 Trauma Centre is expected to treat on average 150 femoral shaft fractures yearly by IM nailing. In regards to this it can be calculated that the price for storage and sterilization per surgical procedure for IM nail ranges between $34 and $100 while on the other hand for locking rods the price per procedure for sterilization and storage would be approximately in a range between $20 and $54.
Complication and reoperation costs
The complication rates for IM nails used to treat femoral and tibial shaft fractures is estimated to range from 5% to 10% for the need of reoperation, with the managing complications cost averaging $15,000 to $30,000 per event. For the universal locking rod system, the complication rate was slightly lower between 3% to 7% for femoral or tibial shaft fractures, with associated costs for managing complications estimated to range between $12,000 and $25,000, this reflects the slightly higher intervention requirements of the IM nails compared to the surgical requirements of the universal rod systems.
Total procedure costs comparison
The total cost for each implant, considering all the categories taken in account (implant cost, instrumentation, operating room time, sterilization, storage and complications management), is summarized below (Table 1):
Cost summary
The average total cost per procedure for surgical treatment of femoral shaft and tibial fractures using IM nails ranges between $21,343 and $44,100. For the treatment of tibial shaft of femoral shaft fractures, using the locking rod costs were estimated to range between $17,870 and $38,254.
In this comparison, IM nailing is slightly more expensive than treating the same fractures by universal locking rod systems with the cost difference ranging between $3,473 and $5,846. The main contributors to the cost difference include the slightly higher surgical time for IM nailing, as well as higher staffing and operating room costs in addition to higher complication rates reported.
Cumulative annual cost comparison
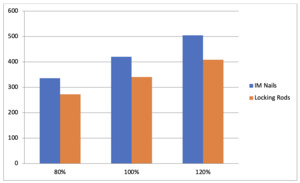
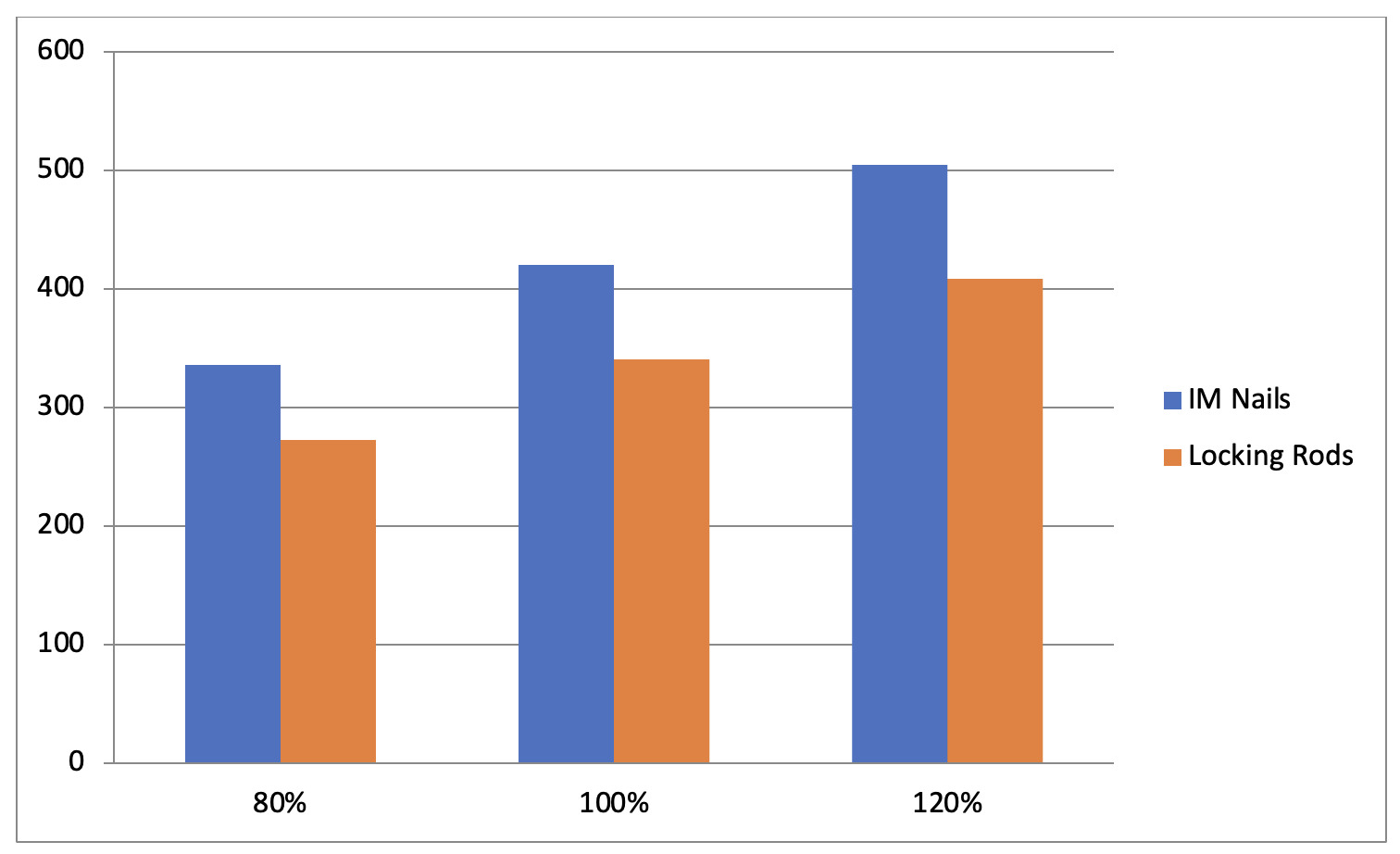
To further illustrate the financial implications, a cumulative annual cost comparison was developed based on an estimate of 150 cases of IM nailing per year. (Figure 1)
The figure highlights an approximate savings of 20% annually with the use of universal locking rods due to the lower operative costs, lower inventory costs and fewer complication costs.
Statistical Analysis
The comparative statistical analysis between intramedullary nails and universal locking rods was performed using independent samples t-tests. For each cost category, datasets were simulated by generating 30 values around the midpoint of the reported cost ranges, applying a ± 20% standard deviation to model realistic economic variability. The analysis revealed statistically significant differences in several key cost categories, including implants, instrumentation, sterilization, complications and total procedure cost. Operating room costs, however, did not show a statistically significant difference (t = 0.84, p= 0.40). (Table 2)
Simulated datasets (n= 30 per group) were generated using midpoint values from reported cost ranges, with ±20% standard deviation applied to model real- word pricing variation. Independent samples t-tests and Mann-Whitney U tests were conducted to compare costs between IM nails and universal locking rods, providing both parametric and non-parametric validation of results.
To validate the robustness of the findings, Mann – Whitney U tests were also performed for each cost category. These non-parametric tests yielded statistically significant differences in all categories, except for operating room costs (U = 560, p = 0.1055), thereby confirming consistency with the t-test results.
Sensitivity Analysis
A sensitivity analysis was also conducted to explore the robustness of the findings. This involved assessing the influence of fluctuations in critical cost components, such as complication rates, sterilization procedures and operating room duration, on the overall cost comparison between IM nails and universal locking rods.
A sensitivity analysis was conducted to test the robustness of these financial findings under fluctuating clinical and operational costs, the results are visualized below. (Figure 2)
Cost scenarios simulate +/- 20% variation in critical financial variables (complication rates, operating room duration and sterilization costs). Universal locking rods consistently exhibit lower total costs across all modeled scenarios.
4. Discussions
IM nails are typically manufactured in multiple lengths and diameters, requiring stocks of a wider range of sizes. This will often result in higher inventory costs, as different patients require different nail lengths for example for femoral nails: 340 mm – 440 mm and for tibial nails: 260mm – 420mm with diameters of nails being typically between 9 mm to 13 mm.
The universal locking rod systems, unlike traditional IM nails, are adjustable in length intraoperatively, reducing the need of stocking multiple sizes for each implant. Universal locking rod systems allow for intraoperative cutting, eliminating entirely the need for any pre-sized implants. The locking mechanisms are design in such a way that they can accommodate different bone diameters, further minimizing the number of implants required to stock.
Because the locking rod systems are designed with adjustable features in order to work across a range of fractures, they typically require fewer inventory variants (different sizes of rods for femoral and tibial fractures). This reduces hospital costs associated with multiple rod sizes and complicates inventory management. The rod systems are generally sold in a range of standardized options, usually based on common rod lengths and diameters.
Another important aspect is that the pre-selection of nail sizes does require additional planning and occasional delays in surgery if the correct size isn’t available at the scheduled time, for this reason due to the universal rod systems intraoperative adjustability, there is no need for multiple pre-sized implants and this might in the end reduce surgical delays and potential misfits.
Given the necessity of bigger stocks for IM nails, hospitals must sterilize and store multiple implant sizes, and this increases the costs of treatment, on the other hand for universal locking rod systems, fewer implants are required to be stocked, sterilized and stored, and this significantly reduces logistical and sterilization costs. Hospital can save between 30% and up to 50% in costs regarding sterilization and storage by reducing implant variety regarding the treatment of the same fractures.
Universal locking rod systems have greater flexibility in fit and because of that they reduce the risk of implant related complications when compared to IM nails in which size mismatches or inventory shortages can lead to delays, complications or even the need for surgical re-intervention.7
The present study highlights a substantial economic advantage in favor of universal locking rod systems over intramedullary nails in treating femoral and tibial shaft fractures. While IM nails remain a widely accepted gold standard due to their biomechanical strength and early mobilization benefits, our findings underscore the long-term cost implications that are often overlooked during implant selection.
Several existing studies confirm that the timing, complexity and technical precision required for IM nailing procedures affect outcomes and resource consumption. Patel et al. reported that delayed IM nailing led to increased complications and extended hospital stays, which contributes significantly to cumulative costs.8
Traditional IM nail systems necessitate extensive preoperative planning and the availability of multiple implant sizes, which leads to greater inventory costs and surgical delays. These logistical constraints are echoed in large-scale orthopaedic references, such as Rockwood and Green’s Fractures in Adults, which discusses how implant variety requirements can burden high-volume trauma centers.9
Beyond procedural efficiency, implant selection also plays a role in the frequency and type of complications. Nonunion, malunion and infection not only increase the clinical burden but also significantly drive up postoperative costs. Morshed emphasized that delayed union or misalignment often leads to reoperations, thereby reinforcing the financial impact of poor implant compatibility.10 Furthermore, Christy et al found that reoperation rates for IM nails in femoral fractures can exceed 10% of cases, which aligns with the complication ranges used in our financial models.11
Sterilization and implant waste also form a major part of the total procedural costs. Studies by Pfefferle et al. have stressed the absence of standardized guidelines in orthopaedic trauma regarding implant waste, noting that unutilized implants contribute to significant financial inefficiencies.12
Our cost comparison aligns with findings by Laurut et al., who conducted a systematic review quantifying surgical waste and linking it to complex instrumentation requirements and lack of intraoperative flexibility.13 The universal locking rod system addresses this issue by allowing intraoperative length adjustments, reducing the need for a variety of pre-sized rods and minimizing the likelihood of surgical delays due to inventory mismatches.
The choice between implant systems becomes even more critical in diverse healthcare environments. Zhang et al compared locking compression plates and IM nails in a cost-effectiveness study conducted in a low-resource setting, noting that intraoperative adaptability can directly improve both cost-efficiency and patient outcomes.14 This further supports our findings that universal rod systems, while potentially more expensive up front, reduce downstream costs and logistical burdens.
In high-income trauma centers, overall cost-efficiency is influenced by both direct implant pricing and indirect variables like staffing, operating room occupancy, and equipment sterilization. Vanderkarr et al. modeled these interactions and found that streamlining surgical workflows via adaptive implants contributed to decreases in cumulative operating costs.15 This reinforces the conclusion that locking rod systems, despite higher pricing per unit, achieve greater financial sustainability in the long run.
Lastly, registry-based studies, such as Wähnert et al. indicate that IM nailing although effective, still caries notable complication rates requiring intervention. This supports the marginally higher complication costs we reported for IM nails and reinforces the clinical viability of switching to more adaptable systems like locking rods.16
In summary, while both implant systems deliver acceptable clinical outcomes, the long-term financial implications and institutional efficiencies achieved with universal locking rods position them as a cost-effective alternative. They minimize procedural variation, reduce logistical costs, and lower the rate of implant-related complications, thereby supporting a shift in procurement strategies for orthopaedic departments in high-volume trauma centers.
Limitations
The study relied on average costs derived from existent market data, which might vary by region, healthcare system and specific supplier agreements.
The study focused primarily on direct costs and did not capture all potential indirect costs, such as a broader institutional resource utilization that could affect financial sustainability.
Variations in implant pricing, instrumentation costs and sterilization procedure from different suppliers or different healthcare systems might have affected the generalizability of the findings.
5. Conclusion
This study highlights the financial impact of implant selection in orthopaedic trauma surgery, demonstrating that universal locking rod systems may offer significant cost advantages over traditional intramedullary nails. These advantages extend beyond implant pricing, encompassing reduced surgical time, simplified inventory management, and potentially lower complication burdens.
For institutions seeking to optimize surgical workflows and reduce overhead costs in high volume trauma care, locking rod systems present a practical and sustainable solution. Their intraoperative flexibility, reduced need for implant variety and ease of sterilization can collectively streamline orthopaedic surgical procedures.
Ultimately, implant procurement decisions should not be based solely on initial purchase costs, but on the broader economic and operational value delivered across the continuum of patient care. This study encourages orthopaedic departments and hospital administrators to critically evaluate how innovation in implant design can contribute to long-term efficiency and cost containment.
Author contributions
L.M.: Methodology; Formal analysis; Investigation; Resources; Data curation; Writing; Review and editing; Visualization; Project administration; Funding acquisition
C.C: Investigation; Visualization; Project administration;
A.L: Conceptualization; Methodology; Formal analysis; Resources; Data curation; Writing; Review and editing; Visualization;
M.S: Software; Statistical analysis;
J.P. Jr.: Validation
S.F: Validation; Statistical analysis;
J.P. Sr.: Validation; Supervision;
All authors have read and agreed to the current manuscript to be published.
Conflict of interests
The authors declare no conflict of interests and the funders had no role in the design of the study, in the collection, analysis or interpretation of data, in the writing of the manuscript or in the decision to publish the results.
Funding
We would like to acknowledge VICTOR BABES UNIVERSITY OF MEDICINE AND PHARMACY TIMISOARA for their support in covering the costs of publication for this research paper.
Data availability statements
Data contained within the article or supplementary material and the original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding authors.