Introduction
Due to its extensive range of motion, the shoulder joint is considered the body’s most mobile. However, due to its flexibility, it lacks stability and is more prone to injury. The humerus and scapula are the two primary bones that make up the shoulder. Round in shape, the humerus’s end slides into a scapula socket. There is a collection of ligaments and muscles that surround the shoulder. Shoulder bones are joined by ligaments and tendons join the shoulder muscle to the bones.1
Shoulder injuries may occur as a result of direct or indirect causes. A fall onto the arm could injure the shoulder. Falling on an extended hand when the upper limb is twisted at an angle to the trunk or when the arm remains motionless while the trunk is forcefully distorted are examples of indirect mechanisms. Shoulder trauma may lead to a variety of pathologies, including simple dislocations (anterior, posterior, or inferior), proximal humerus fractures, or fracture dislocations. Among the many kinds of bone breaks experienced by the elderly, a proximal humerus fracture ranks high. Dislocations tend to manifest in two age groups: younger men and women over the age of 50.2 Shoulder injuries accounted for 17% of all injuries, with yearly rates ranging from 2% to 34%. The majority of shoulder injuries, especially locking (30%), were incurred by forwards (63%). The AC joint was the most frequently affected joint (47%), and the most frequent type of damaged tissue was the ligament/joint capsule (65%).3
Traumatic events often result in shoulder injuries, more especially those affecting the glenohumeral articulation. Factors including age, bone density, muscular strength, and the biomechanics of the traumatic event might influence the types of injuries that can occur. In order to effectively treat shoulder diseases, it is essential to understand how various injuries impact the functional architecture of the shoulder. Therefore, by understanding these systems, which allow them to foresee certain patterns of injury, medical experts may appropriately diagnose and treat shoulder diseases.4
Minimally invasive (MIS) procedures are increasingly being used instead of traditional open approaches for several surgical purposes. Compared to open techniques, MIS approaches have a smaller incision size and need less tissue dissection, which contributes to their growing popularity. Reducing surgical stress to the surrounding tissues is thought to lower the inflammatory response, reduce morbidity, and result in earlier functional recovery and fewer difficulties with wound healing. MIS’s restricted surgical exposure, however, may raise the chance of harming structures that are not immediately visible.5
Among the most important technical developments in orthopedic surgery throughout the 20th century was arthroscopy, a less intrusive substitute for open surgery that is now among the most prevalent orthopedic surgical procedures. Arthroscopy has progressed from its original use as a diagnostic tool to its current position as a possible therapy for a wide variety of diseases and injuries. Thanks to advances in arthroscopy, many injuries may now be treated, facilitating a quicker return to full function.6 Among orthopedic operations, the second most common is shoulder arthroscopy, followed by knee arthroscopy for partial meniscectomy. When other imaging studies have failed to diagnose the cause of your unusual shoulder pain, osteoarthritis, frozen shoulder, synovitis, adhesive capjualitis, subacromial impingement, acromioclavicular joint disorders, or atypical shoulder pathology, your doctor may recommend a shoulder arthroscopy.6
Even while overall morbidity has decreased with arthroscopy as compared to open procedures, the treatment is still invasive and carries inherent hazards. There have not been many literatures discussing arthroscopy as a MIS procedure that can be used as a consideration for choosing this technique in treating shoulder trauma. Therefore, researchers are interested in discussing the literature review regarding the role of arthroscopy as minimal invasive for shoulder trauma.
Methods
The authors conducted a literature search by manually scanning the PubMed database from 2015 to 2024 using the following keywords: “arthroscopy”, “minimal invasive”, “minimally invasive procedures”, “shoulder trauma”, “shoulder injury”, “shoulder arthroscopy”, “arthroscopic shoulder”, “therapy,” “therapeutic approach,” and “treatment” (when combined with the Boolean operators “OR” and “AND”). This review only includes full-text articles that were published in English. In all, nine primary articles were located that were relevant to the subject of this study.
Result
Shoulder Trauma
1. Incidence
The majority of shoulder dislocations happen to men. Patients who are young and active exhibit the highest incidence, peaking in the 16–20 age range. After age 50, the frequency rises in females, peaking in patients between the ages of 61 and 70. If an orthopedic surgeon conducted the initial reduction or if it was connected to a larger tuberosity fracture, the chance of recurrence is decreased. Higher medical comorbidity scores and older ages also reduce the risk of recurrence.7 In clinical settings for musculoskeletal and sports medicine, shoulder trauma are frequently treated. The most typical site of a throwing-related injury is the shoulder. Over 2.1 million American high school athletes who play baseball, softball, volleyball, and American football are susceptible to shoulder trauma due to their activity.8
Roughly 95% of shoulder dislocations occur in the front of the shoulder. Subglenoid, anterior/axillary, and subcoracoid displacements are the three possible locations for the humeral head. A posterior glenohumeral dislocation accounts for around 2-5% of all dislocations in the shoulder caused by trauma. It is still difficult to get a reliable incidence estimate because of the high prevalence of undetected dislocations. Proximal humerus fractures make up around 6% of all fractures in Western countries. After spinal and distal radius fractures, it is the third most common osteoporotic fracture. There is a 70:30 gender ratio, the highest occurrence is between the ages of 60 and 90, and adults over the age of 50 make up around 85% of these fractures. B1.1 is the most prevalent fracture type according to the Arbeitsgemeinschaft für Osteosynthesefragen’s (AO) categorization system. Twenty percent of valgus instances include this group of people. Of all proximal humeral fractures, more than half are of types B1.1, A2.2, A3.2, or A1.2 AO, whereas only 6% are of type C.4
2. Mechanism
Shoulder Dislocation
Because the mechanisms that produce glenohumeral articulation dislocations and larger tuberosity fracture dislocations are similar, we may choose to investigate them together. The glenoid fossa and larger tuberosity connect at the back during extension, external rotation, and abduction. When held in this position, the subscapularis muscle is tightened to its maximum. The subscapularis muscle had to be strained or partly ruptured to make dislocation easier. At the same time, the rear margin of the glenoid touched the greater tuberosity, thus it had to be scraped. Based on these findings, a new kind of shoulder fracture known as dislocation with increased tuberosity was developed. The most common method of injury causing anterior dislocation is the application of an external rotational force to an extended and abducted limb. A back dislocation occurs when the internally rotated arm experiences axial tension after taking a blow to the front shoulder. The majority of inferior dislocations occur as a result of hyperabduction, which is when the abducted arm experiences axial stress.4,9
Hill-Sachs lesions were first described as situations in which the humeral head, which is housed in a small pocket, contacts the posterior aspect of the glenoid fossa, leading to an impression fracture on the side that is visible from the outside. Occasionally, a more significant tuberosity fracture develops. The humerus, subscapularis muscle, anterior glenoid labrum, and cartilage may be injured when the force is given without shattering bones, but it does strike the front parts of the joints. However, there is some disagreement about where exactly in the glenoid fossa the humeral head makes contact. While some writers point to the back, others to the front.4,9
Proximal Humerus Fractures
Few details on the pathobiomechanics of fractures in the proximal humerus are known. One or more of the following may be to blame: the arm’s position in relation to the body at the time of impact; fractures that spread along the epiphyseal lines of the proximal humerus; or deforming stresses applied to the fracture fragments by the rotator cuff muscles. Proximal humerus fractures may occur due to either direct or indirect sources. 11 A fall is a known direct cause of shoulder fractures. The characteristic manifestation of this high-energy injury is the humeral head directly impacting the scapula without any axial arm force. When a person slips and falls onto an outstretched hand, rather than hitting the exact location of the break, it might lead to an indirect fracture. Flexion and abduction are two possible positions for the hand, while abduction and external rotation are two more. The indirect mechanism is more prevalent than the direct one because it places a smaller but still substantial energy burden on the arm. One of the rarest ways a bone might break is if the muscles around the shoulder tighten too much, as happens during convulsions or electric shock.4,10
An attempt to stop an uncontrolled sliding forwards or sideways causes the fracture in the indirect process. Most of the time, when someone falls onto an extended hand, the trunk will twist around that point, which will cause the proximal humerus to move in an abducted or adducted manner. Although a correlation between posterior dislocations and anatomical neck fractures has been noted in a few articles, the exact process remains unknown. Hill-Sachs lesions and larger tuberosity fractures are possible causes of anterior dislocation.11
Research into Hill-Sachs lesions and larger tuberosity fractures suggests they may have an origin. The glenoid fossa and larger tuberosity connect at the back during extension, external rotation, and abduction. More serious fractures, such as those of the posterolateral humeral tuberosity or impaction, may result from this. The ligaments that stabilize the joint determine the degree of damage; hyperabduction, which presses the humeral head on the acromion, may cause an inferior dislocation or a valgus impacted two-part proximal humeral fracture. Few studies have examined the underlying mechanisms that lead to glenoid impaction, two-part proximal humeral fractures, and humeral head split fractures.4,11
Shoulder trauma in sports
Shoulder injuries are common in contact sports with a lot of physical contact, such as hockey and rugby. Researchers have spent a lot of time trying to figure out how certain sports cause injuries to various parts of the body, particularly the soft tissue around the shoulder joint. There are three common movements that can cause shoulder injuries: the “Tackler” (when an unsteady hand is forced to abduct and extend during tackling), the “Try-Scorer” (when an athlete falls while their arm is outstretched and hyperflexed), or the “Direct Impact” (when the arm is adducted, representing the direct impact of the humeral head on the scapula without axial load to the arm). The “Try-Scorer” and “Tackler” mechanisms, Bankart, reverse Bankart, tears in the anterior and posterior labrum, and shoulder dislocations were all too common. Most rotator cuff injuries occur as a result of “Try-Scorer” mechanisms. The only mechanism that might dislocate the acromioclavicular joint and fracture the scapula was the “Direct Impact” mechanism, which often causes labral damage and glenohumeral dislocation.12,13
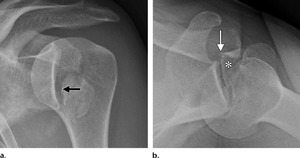
3. Imaging
Shoulder Dislocation
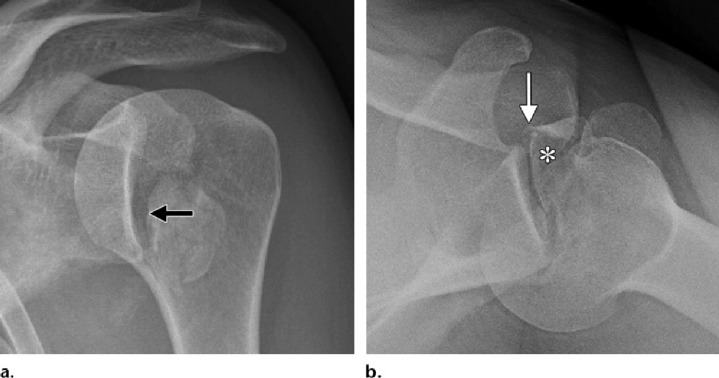
It is standard procedure to take simple anteroposterior radiographs both before and after a dislocation. Anteroposterior radiographs are the only imaging tests often performed during an emergency. Doctor usually perform axillary and/or transcapular projection if they suspect a posterior dislocation, even they don’t know which way the force is coming from. There is a 50% chance that anteroposterior radiography will overlook posterior dislocations. In the absence of other perspectives, a multitude of frontal indicators may be used to identify posterior dislocation. At the location of the impact fracture on the anterior humeral head, a sclerotic line may be seen in the axillary view. Reason being, a 6 mm or greater rise in the articular distance indicates either the trough indication or the rim sign.14
When the direction of the force cannot be determined, CT imaging is the suggested method. Dislocation in conjunction with a bony-Bankart lesion and a larger tuberosity fracture are also covered in depth. CT scans, using the best-fit circle method in the sagittal plane, provide the most precise evaluation of glenoid injury. It is crucial to diagnose glenoid bone loss because instability is likely to occur when a defect affects more than 20% of the entire glenoid surface or more than 7 mm in width.15
Patients with a dislocated shoulder are not usually considered to need MRIs or other imaging investigations. An MRI is often required after the early post-traumatic period when there is suspicion of soft tissue injury or the appearance of joint instability. When it comes to diagnosing soft tissue injuries like rotator cuff tears, labral tears, or cartilage damage, magnetic resonance imaging (MRI) is the gold standard.15
Proximal Humerus Fractures
Because the current idea is that the rotator cuff muscles displace independent pieces, the simplest tests are used to image proximal humerus fractures. It has been demonstrated that the axillary view in conjunction with the anteroposterior view improves classification accuracy. Both the intraobserver and interobserver reliability of current categories, including the AO/Orthopedic Trauma Association and Neer, are low, regardless of the imaging modalities utilized. In addition, surgeons often use 3D CT to evaluate complicated fracture patterns, even though some authors claim that these studies show higher intraobserver and interobserver agreement. Because of this, not even shoulder experts can determine the best imaging approach to accurately detect fractures by balancing categorization. In addition, the Neer classification of the four segments is not based on radiographic data. The pathoanatomical categorization that is attained by exact x-ray studies, film interpretation, and sometimes intraoperative results forms its basis.16
Other, more important criteria that are best evaluated with CT scans include articular surface separation, humeral head impaction, and segment rotation. With the identification of valgus rotation of the humeral head among isolated segments of the tuberosities, a new form of valgus-impacted four-part fracture was introduced to the Neer classification in 2002. In these cases, the glenohumeral articular surface is maintained, instead of the usual four-part proximal humerus fracture. The nutritive arteries penetrate the bone and deliver perfusion to the arcuate vessels via an unbroken medial calcar, reducing the risk of post-traumatic avascular necrosis. Surgery is not always necessary to treat this issue.17
Shoulder trauma in sports
Acute or chronic shoulder injuries are common in athletics. Repetitive stress injuries are another common cause. Sports injuries may impact any part of the shoulder, whether it’s the osseous or soft-tissue components. However, recent studies have shed light on the most common patterns of damage to the labrum, biceps pulley, rotator cuff, and humeral head. Magnetic resonance imaging (MRI) provides superior soft-tissue information for pathology evaluation in injured athletes. Magnetic resonance imaging (MR) scans reveal the glenohumeral ligaments, labrum, capsule, and cartilage with remarkable clarity. An MRI may show the range of stress injuries, as well as details about the bone marrow, a stress fracture, or an early stress response. The following Bankart lesions and variants, such as Anterior Labral Periosteal Sleeve Avulsion (ALPSA) lesions, may be documented using an MRI scan; However, the most efficient way to localize these lesions may be by MRI arthrography, which incorporates the Abduction and External Rotation (ABER) view.18,19
4. Treatment
Even though nonoperative treatment was possible for the majority of fractures affecting the shoulder, many of them are now being treated with surgical techniques such endoprosthesis, plating, nailing, and percutaneous wire fixation. There are many treatment options for complex proximal humeral fractures, managing them is still difficult because of a number of issues, including low bone stock, fracture comminution, and related comorbidities in older patients. Surgical complications, including screw cutting and loss of reduction due to varus misalignment, may develop in these fractures. Although locking plate fixation is the treatment of choice for these fractures, it is not without its risks; in fact, revision rates may reach 25%. Therefore, it is prudent to choose the right treatment for the right patient. Several surgical procedures, such as anatomical reduction, calcar screw insertion, and fracture augmentation with bone graft and cement, may provide satisfactory outcomes. Proper prosthesis implantation and anatomic correction of tuberosities during arthroscopy require similar considerations. Fracture complexity is a major factor in determining the optimum fixing method, however patient factors and surgeon expertise also play a role.20
Shoulder Arthroscopy
Arthroscopic shoulder surgeries are among the most common minimally invasive procedures (MIS) used to restore shoulder function. Shoulder arthroscopy and arthroscopic rotator cuff repair rates, broken down by geographic location, ranged from 64.96 to 623.6 per 100,000 persons in more recent research.23 The most frequent orthopedic operation for partial meniscectomy is knee arthroscopy, followed by shoulder arthroscopy. Shoulder arthroscopy is a common method for treating pathologic shoulder conditions including adhesive capelusitis, subacromial impingement, illnesses affecting the proximal biceps, rotator cuff tears, labral tears, loose bodies, and degenerative arthritis. Management of shoulder instability and rotator cuff pathology are the two most prevalent reasons for arthroscopic shoulder surgery. There are many advantages of arthroscopy over open surgery. Some of them include a better ability to see intra-articular disease, less complications, shorter recovery times, and less time away from work.6
1. Brief History
Burman reported the first shoulder arthroscopy on cadavers in 1931. The procedure was not described for the first time in a clinical setting until 35 years later. Since its initial performance by Harvard Ellman in 1985, arthroscopic subacromial decompression has become a standard arthroscopic operation. The differential diagnosis of the aching shoulder has been expanded by the analysis and classification of new lesions that were previously undetected. An example of this is Steve Snyder’s explanation of how overhead athletes might suffer from SLAP (superior labrum anterior and posterior) injuries. The way Walch (1991) characterized the cuff’s internal impingement on the labrum’s posterosuperior part during external rotation and abduction is another. New methods for arthroscopy-assisted fracture repair, bone grafting, and arthroscopic Weaver-Dunn operations have emerged in recent years. One disadvantage of doing more complex surgeries using a scope is the increased risk of complications.21
2. Benefits
Joint surgery needed large incisions and arthrotomies to expose and treat joint pathology before arthroscopy and its specialized equipment were widely used in clinical settings. Comparing arthroscopy to such lengthy open arthrotomies, there are a number of benefits. In contrast to MIS arthroscopic treatments, the longer joint exposure results in increased discomfort and recovery time, as well as an increased risk of consequences like infection and arthrofibrosis. Compared to traditional procedures, MIS operations typically cause less discomfort and swelling after surgery. Patients who have arthroscopic treatment so typically recover more quickly, start their rehabilitation earlier, and are able to resume regular activities and employment sooner.22,23
Another socioeconomic benefit of arthroscopy is that it may be performed in an outpatient setting, which is a huge plus for patients. Some arthroscopists may even work in an office environment, which helps keep costs down even more. Arthroscopy may make use of both local and general anesthesia. Procedure, patient desire, and expert medical opinion all play a role in determining the anesthetic type.24
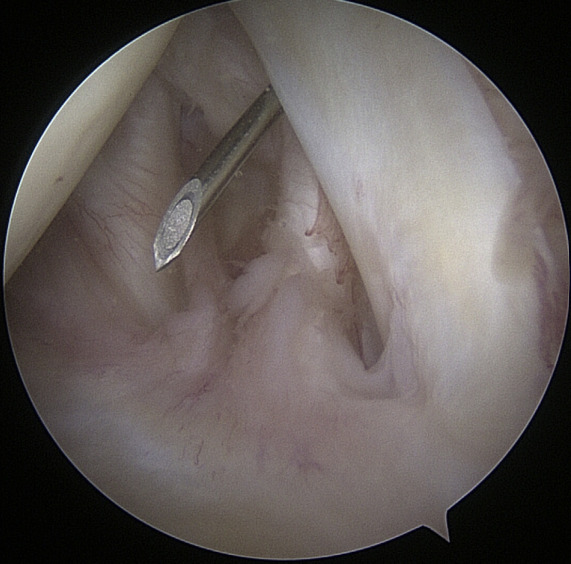
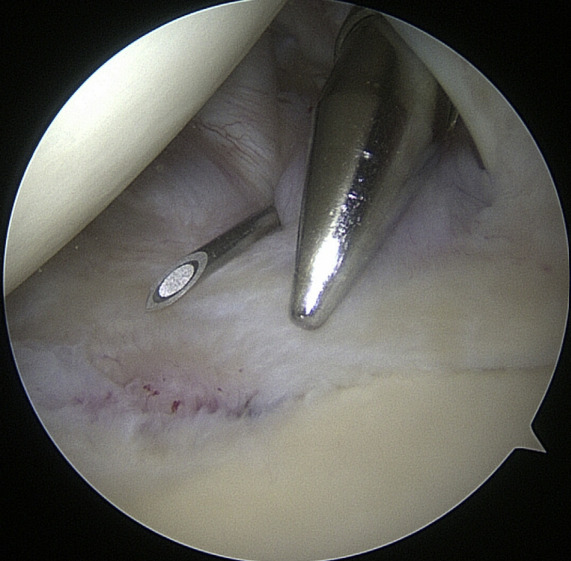
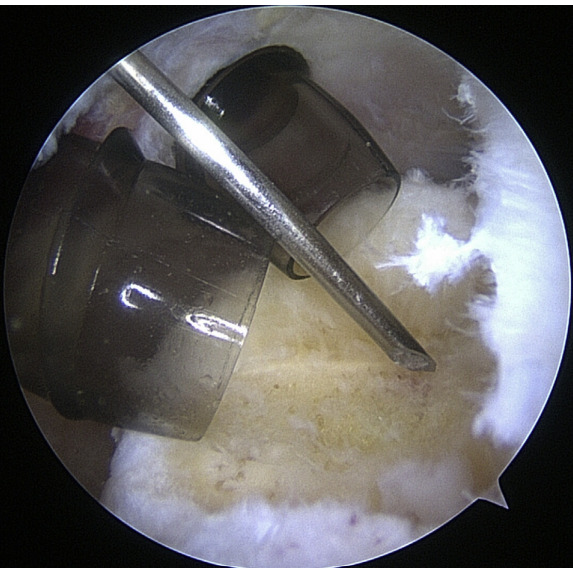
3. Surgical Technique
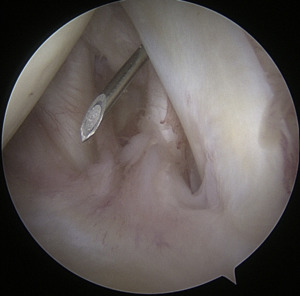
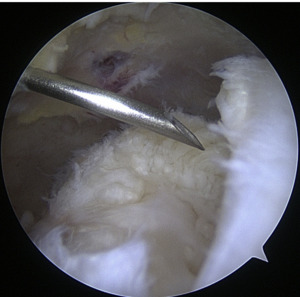
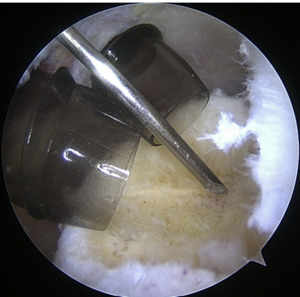
Instrumentation
When it comes to shoulder arthroscopy, the most common arthroscope utilized is the 4.0 mm 30 scope. A 30-magnification scope is sufficient for most situations. An arthroscopic-assisted coracoclavicular reconstruction, subscapularis repairs, Remplissage procedures, glenohumeral ligament lesions, and humeral avulsion can all benefit from the use of a 4.0-mm 70 arthroscope, which should always be on hand. There should be a large selection of cannulas accessible, and they will differ according on the operation being carried out.25
As the principal penetrating instruments, 5.5-mm blunt-tipped cannulas are often used for portal insertion. Blunt tips are preferred to reduce the likelihood of iatrogenic harm, especially to articular cartilage. Because they are easily passable by the majority of arthroscopy passing devices, 8.25-mm cannulas are often employed for “instrumentation” portals. In addition, cannulas of 6.5 mm or less are commonly used in suture management. Cannulas that are threaded or have locking mechanisms are preferable since they are less likely to come free from the joint. In most cases, one of two methods can be employed: gravity or a pump system. Sufficient management of pressures, usually approximately 60 mm Hg, is necessary to avoid significant soft-tissue edema, which can complicate the use of cannulas and instruments.25
Patient positioning
Surgeons are left with few options when it comes to patient placement, since both the beach chair and lateral decubitus postures have been shown to be safe and effective. The lateral decubitus posture helps to reduce intraoperative cerebral hypoperfusion, and the use of balanced suspension allows distraction over the glenohumeral joint, which may increase intra-articular visualization. On the other hand, if the surgeon decides they need to change the arm position during the operation, the beach chair position (BCP) makes it easier to switch to an open surgery (Figure 2). Injuries caused by traction are less likely to occur as well. After a rotator cuff injury, coracoclavicular reconstruction, or biceps tenodesis, a beach chair could be more useful. When dealing with labral disease, lateral decubitus may be more beneficial. Every bony protrusion is cushioned and the head is attached firmly to prevent pressure sores and neuropraxias.6,25
Sterile Patient Preparation
After proper alignment, sterile preparation and draping are carried out. It is our desire that the patient clean the surgical site the night before and the morning of the procedure at home with a hibiclens scrub. Clippers are used in the preoperative holding area to eliminate body hair. After intubating and positioning the patient in the operating room, plastic nonsterile drapes are used to close off the surgical extremities. Starting at the axilla and working our way to the fingertips, we wipe down the entire upper limb with a mixture of chloraprep, benzoyl peroxide, and alcohol. Benzoyl peroxide reduces the bacterial burden of Propionobacter acnes. An impermeable stockinette is wrapped around the hand and forearm, and sterile drapes are used to cover the shoulders and upper extremities.6
Identification of Surface Landmarks
As shown in Figure 3, during the preparation and draping process, surface markers such as the acromion, coracoid, clavicle, acromioclavicular joint, and scapular spine are identified and marked. The posterolateral corner of the acromion may always be visible, even in shoulder circumstances with a rather large soft tissue surround.6
Standard Portal Placement
A traditional posterior portal would be placed at the “soft spot” of the infraspinatus’s raphe. The standard placement is 2 centimeters inferior and 2 centimeters medial to the posterolateral border of the acromion, however this can change according to the patient’s size. It is possible to make a portal incision after inserting an 18-gauge spinal needle into this region to roughly follow the correct course. The posterior capsule is shattered by inserting a blunt trocar into the joint and directing it toward the coracoid.6
Preliminary surgical planning will establish the exact location of the anterior portal. Arthroscopy techniques for rotator cuff or biceps tenodesis usually include positioning the anterior portal centrally in the rotator interval, near the subscapularis tendon. It is common practice to use two anterior portals while performing arthroscopy on labral disease. The anteroinferior portal, which is often the working portal, is typically located around the subscapularis tendon. An extra portal called the anterosuperior portal may be used for suture inspection or shuttletling without damaging the supraspinatus tendon. Its location is directly above the biceps tendon or just slightly ahead of it. A common technique for creating these portals is the “outside-in” approach, which involves inserting a spinal needle under direct arthroscopy view to determine the correct portal location.6
Setup
The coracoid, acromioclavicular joint, clavicle, and acromion are all marked on the skin. If subacromial work is going to be performed, the subacromial bursa may be infiltrated with up to 30 cm3 of a mixture of 0.25% bupivacaine and epinephrine. A standard posterior portal is the typical site of access to the subacromial area and glenohumeral joint. The typical placement of this opening is 2 centimeters medial and 2 centimeters distal to the posterolateral border of the acromion. Palpating the soft tissues of the posterior glenohumeral joint is a common way to confirm the proper position. An anterior portal develops after the joint has been inserted. Figure 4 shows that the surgeon has the option of employing a spinal needle to perform it from the outside in or an inside out approach, depending on his or her choice. The anterosuperior portal is located just off the outside edge of the acromion. You may find the anteroinferior portal directly on the side of the coracoid. One centimeter below the anteroinferior portal is the 5 o’clock portal, which is defined as passing through the subscapularis tendon. Scientists say this entry point is the most common and least invasive as it mimics neurovascular systems. Any anterior portal may be used to conduct basic shoulder arthroscopy. Figure 5 shows the setup of both anterior portals for biceps tenodesis, subscapularis repairs, and labral repairs. For posterior labral repairs, spinal needle localization allows for the creation of an auxiliary posterolateral portal situated immediately distal to the posterolateral limit of the acromion. Anterior positioning of the Wilmington portal, one centimeter laterally to the posterolateral margin of the acromion, is recommended for superior labral repairs. The posterolateral and Wilmington portals are types of trans-rotator cuff tendon access points. Cannulas with the smallest diameters necessary should be used.25
The subacromial region may be accessed via the posterior portal if needed after any intra-articular procedures are finished. Spinal needle localization allows for the creation of a lateral portal, typically 2 cm laterally to the acromion’s lateral border and aligned with the clavicle’s posterior border (Figure 6). For any subacromial surgery, pre-positioned anterior portals may be used (Figure 7). An extra Neviaser portal may be made underneath the spinal needle localization, precisely below the acromioclavicular joint, if that becomes essential. This may be useful for a variety of suture procedures, including those involving the superior labrum, the rotator cuff, and the decompression of the suprascapular nerve (Figure 8).25
4. Complication
Arthroscopy is a technically complex surgery that calls for a variety of equipment, some of which may malfunction or break during the procedure (such as a camera and monitor, surgical instruments, a pump, a tourniquet, etc.). The equipment should only be used for what it was designed for, and the surgeon should be conversant with it. Anesthesia issues are not specific to arthroscopic surgery; they can also arise. Surgeons performing arthroscopic procedures in a clinical environment must be prepared to address any complications relating to anesthesia. Extra hazards include thrombophlebitis, hemarthrosis, vascular injury, nerve damage, compartment syndrome, infection, and metabolic issues in those with metabolic diseases (gout, diabetes, and steroid use). Even today, arthroscopy carries with it the risks of being an intrusive procedure.26,27
Very rarely does shoulder arthroscopy result in infection. One way to reduce the risk is to take antibiotics before surgery and apply chlorhexidine. Typically, cefazolin is sufficient; however, clindamycin may be used by people who are allergic to it or who are worried about getting P. acnes.25
The Role of Shoulder Arthroscopy and What Should Be Considered in Its Implementation
A few studies have contrasted the arthroscopic method with open surgery. The Buess et al. study reported that arthroscopic techniques were comparable or slightly better than open surgery, however Bishop’s study recommended open surgery for big injuries since it reduced the risk of re-tear. Walton and Murrel conducted a second study in which they contrasted 200 arthroscopic and 200 open operations. In this investigation, tears larger than 16 cm2 were not included, and decompression was needed in every open surgery but 76% of arthroscopic procedures. They came to the overall conclusion that when taking into account factors like recuperation time after surgery, rotator cuff muscle integrity and operating time, arthroscopic procedure was superior to open surgery.28
Open surgical treatments are still important, even though arthroscopy seems to be better overall. Perhaps because less acromioplasty is required with open surgery, patients report less postoperative discomfort compared to those who have had arthroscopic procedures. Because less acromioplasty was required in open surgery to enlarge the subacromial area, patients reported less discomfort after the procedure. Open surgery often has better results than arthroscopic surgery when comparing the two methods, particularly for individuals requiring acromioplasty. As a result of more frequent acromioplasty, the arthroscopic group reported higher pain levels, which highlights the importance of this procedure on pain management and recovery after shoulder tear therapies.29
Shoulder arthroscopy is a minimally invasive surgical procedure that may be used to diagnose and treat conditions such as rotator cuff tears, recurring instability of the joint, and disease below the shoulder blade. It is associated with benefits such as faster recovery and reduced postoperative discomfort as compared to open surgery. More than 1.4 million shoulder arthroscopies are carried out every year due to the technique’s widespread use. Recent research, however, has focused mostly on fluid drainage, anesthetic, and patient position as they relate to shoulder arthroscopy. Early detection, avoidance, and effective treatment of these disorders may be achieved by understanding their underlying causes.30
Extreme instances of subcutaneous emphysema, pneumomediastinum, tension pneumothorax, air embolism, airway edema, and tracheal compression might result in the death of the patient due to irrigation fluid extravasation. Risk factors include obesity, excessive pump pressures, large quantities of irrigation fluid, sub-acromial pathology, and long-term surgical treatments. Systemic effects such as weight gain, decreased hemoglobin and hematocrit, and others may result from fluid accumulation. During the 12-hour resorption period, the long-term consequences can be too much for the elderly to handle. Airway edema is more likely to occur in six of the following situations: sub-acromial procedures; lateral decubitus position (LDP); longer surgical periods; loose connective tissue; intraoperative hypertension; and high pump pressures.30
Less time spent in surgery, less risk of complications, shorter operating times, controlled irrigation fluid flow rates (50 to 150 ml/min vs. 40 to 80 mmHg), continuous outflow conduits, and combining general anesthesia (with the airway secured) with hypotensive anesthesia for some patients are all factors that contribute to a safer procedure. You can reduce the chance of airway blockage by looking for signs of it during direct laryngoscopy or bronchoscopy, keeping an eye out for a rise in neck circumference following surgery, being proactive about preventing airway blockage, and, finally, making sure there is no leak by doing a positive cuff leak test with endotracheal cuff deflation when the procedure is over.30
While both the BCP and the lateral decubitus position (LDP) have certain advantages for surgeons, there isn’t enough data to conclude that one position is better than the other in this regard. Nonetheless, traction injuries and direct nerve damage are more frequently linked to LDP. Airway compromise in LDP related to extravasated fluid is partly caused by gravitational pull. Pre-operative head cushioning, periodic head/neck position checks throughout the surgery, and avoiding postures of excessive neck flexion and unintentional cervical extension can all help to reduce morbidity. For arthroscopies in BCP, hemodynamic and cerebral perfusion pressure monitoring is crucial. When administering hypotensive anesthesia in this position to older patients or those with high resting blood pressure, caution should be exercised. Hypotension and bradycardia events (HBE) occur at a rate of 4% to 29% yet go unreported despite the fact that they may have fatal consequences including cardiac arrest. To avoid HBE, it is important to manage fluid deficits and blood loss aggressively, avoid using adrenaline during skin infiltration or interscalene block, and utilize β adrenergic blockers such as metoprolol as a preventive measure.30
The less intrusive nature of arthroscopy and the continuous irrigation of the joint, which minimizes the possibility for wound infection, clearly explains why arthroscopy is associated with fewer complications despite a small minute increase in operating time. The degree of surgical invasion, which is higher in open repair, is a significant determinant that probably adds more to the risk of infection than operating duration, although the two are connected. It is probable that the longer operating periods associated with arthroscopy compared to open surgical procedures are a result of the greater technical complexity of arthroscopic surgery and its capacity to treat extra disease that is sometimes not visible during open repairs.31
Increased versatility and effectiveness in treating shoulder pathology can be attributed in large part to developments in MIS methods. Its advantages have been expanded to include high-risk patients and ambulatory surgery. Before irreversible cerebral ischaemia develops, cerebral oximetry combined with non-invasive, affordable, and continuous monitoring of cerebral perfusion may be possible. Technical success can be increased by the experience of the surgeon, time constraints for the procedure, patient positioning, arthroscopic pump pressure minimization, irrigation fluid limitation, purposeful hypotensive anesthesia for specific patients, and appropriate instruments.30
Conclusion
One of the most groundbreaking advances in orthopedic surgery, shoulder arthroscopy offers a less invasive alternative to open surgical procedures, which sometimes require large incisions to expose enough of the joint. Reducing comorbidity, shortening rehabilitation, and the subsequent socio-economic advantages are all proven benefits. As our knowledge of joint pathology grows and new treatment options for unknown or poorly understood joint diseases become available, arthroscopic surgery will play an increasingly important role in the evolution of orthopedic surgery. Every shoulder arthroscopic treatment will have a better chance of success if the surgeon pays close attention to detail while situating the patient, placing the portal, managing fluids, and other aspects
Author Contributions
The authors confirm contribution to the paper as follows:
-
Study conception and design: Febyan, I Putu Dema Prasetya, I Gusti Ngurah Wien Aryana, I Gusti Ngurah Yuda Bagus Aryana;
-
Data collection: Febyan;
-
Analysis and interpretation of results: Febyan, I Putu Dema Prasetya, I Gusti Ngurah Wien Aryana;
-
Draft manuscript preparation: Febyan, I Putu Dema Prasetya, I Gusti Ngurah Wien Aryana.
All authors reviewed the results and approved the final version of the manuscript.
Conflict of interest
The authors have no conflict of interests related to this publication
Funding
self funded
Conference presentation
This literature review has never been presented at any scientific conference.


__coracoid_process_(cp)__clavicle_(c)__acromioclavicular_joint_(aj)__and_s.jpeg)



__coracoid_process_(cp)__clavicle_(c)__acromioclavicular_joint_(aj)__and_s.jpeg)