INTRODUCTION
Background
Left ventricular assist device (LVAD) implantation has allowed for significant survival benefits of patients with heart failure.1,2 Although the LVAD was initially designed to be a temporary solution, it is now used as a final treatment for up to 46% of patients.3 Current uses for LVAD include bridge to recovery, bridge to transplantation, and destination therapy.4 The temporary and final stage uses have expanded the prevalence of LVADs in the medical community.
In addition to offering a significant survival benefit for patients with heart failure by offering mechanical support to cardiac function, their improved design is also essential to note.5 Early designs were bulky, had higher rates of complications, and required patients to remain in the hospital.5 LVAD designs are now smaller, with less mechanical components, and are even capable of adapting during exercise.6–9 These factors helped contribute to increased LVAD utilization and likely encouraged the drive to live a complete life in many domains.
As advancements in LVAD have allowed for greater longevity and quality of life, the management of LVAD-user medical comorbidities has also become increasingly relevant.1,3 LVAD devices have allowed patients the time and flexibility to control chronic medical conditions such as diabetes mellitus and hypothyroidism, for example.10,11 Furthermore, LVAD patients now pursue non-cardiac elective surgery at a greater rate.2
Non-cardiac surgery for LVAD patients is complicated, as there are distinct considerations for anticoagulation, infection risks, perioperative monitoring, comorbidities, and anatomical considerations due to the device.2,12 However, studies have shown that several noncardiac surgeries in LVAD patients are feasible and may be without significant morbidity or mortality.13,14 The orthopaedic surgery field has seen a steady rise in surgical candidates with LVAD and must therefore consider the above considerations.15
Rationale
Our case series study aims to add to the limited existing literature on LVAD patients in orthopaedic surgery. Our hope is to provide awareness of the rising numbers of LVAD patients that may pursue orthopedic procedures.
CASE PRESENTATION
Institutional review board approval was obtained for this study. All patients in this study underwent orthopaedic surgeries at a single institution during a 10-year period. A database query of the electronic medical record using orthopaedic surgeries and LVAD placement current procedural terminology (CPT) codes from 2012 to 2022 were used to find eligible patients. Patients with LVAD placement prior to the surgery were eligible for our study. Furthermore, eligible patients had an LVAD in place during their surgery.
The patient medical records were reviewed for length of stay, discharge disposition, smoking status, type of anesthesia, Elixhauser comorbidity score, ASA score, blood loss, urine output, blood transfusion requirements, thromboembolic events, post-operative and discharge dispositions, readmission rates, and 30 and 90-day mortality rates.
MANAGEMENT AND OUTCOMES
Using these criteria for identifying and excluding ineligible patients, an internal query of our electronic medical record was performed. 40 patients were identified with a total of 47 orthopaedic surgeries. 34 patients underwent one surgery, and 6 patients underwent two or more. The average patient age at the time of surgery was 65, and 85% of patients identified as male. Most patients were white (92.5%). Most patients had an ASA score of 4 and 3 at 53% and 43% respectively. Former smokers and nonsmokers made up 63% and 38% of the patients in this series respectively.
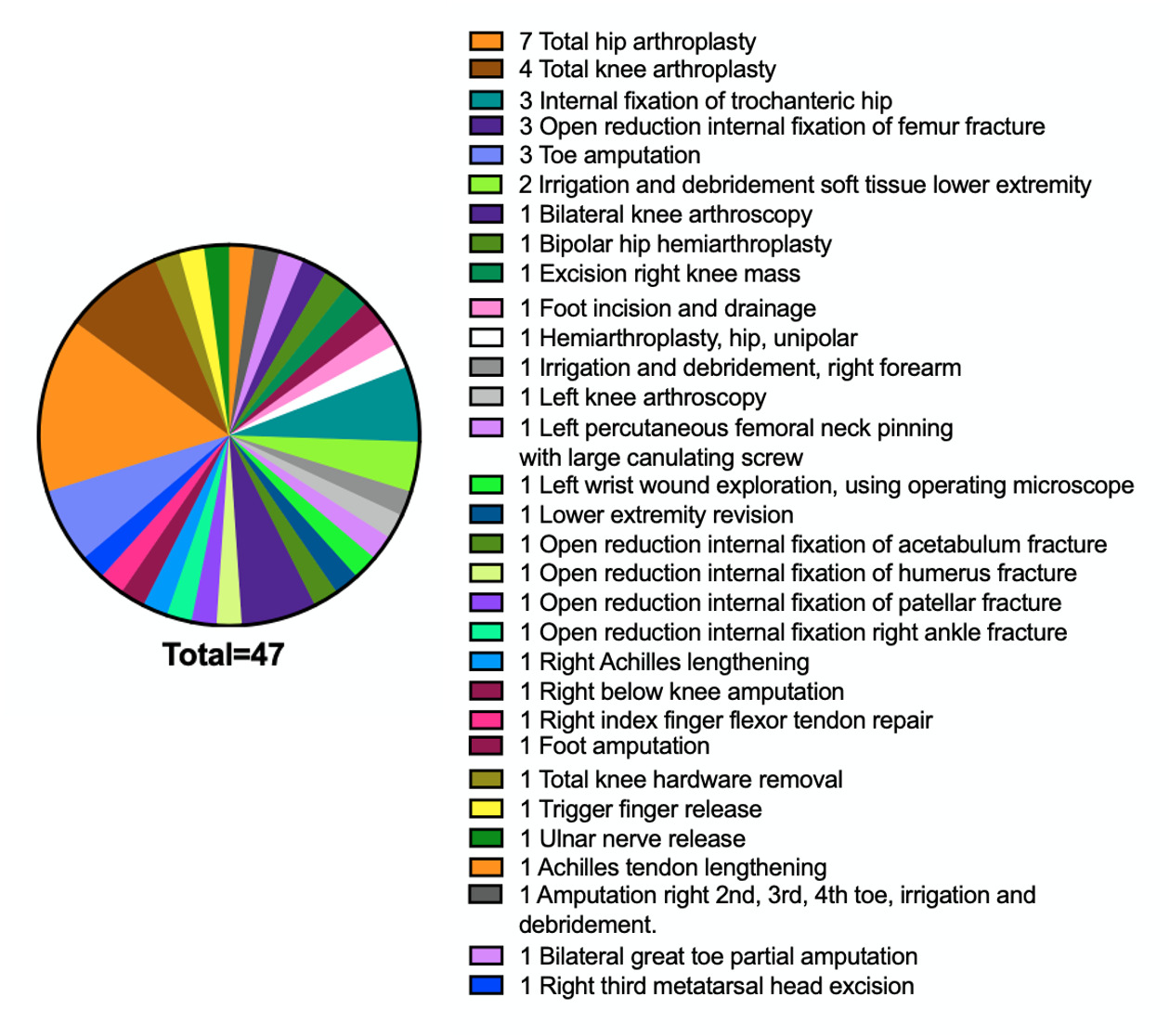
Various types of orthopedic procedures were included and summarized in Figure 1. The average time between LVAD implantation and surgery was 2.5 years (917 days). The mean operation time for total hip arthroplasties and total knee arthroplasties were 163 minutes and 145 minutes respectively. Following orthopedic surgery, the average length of stay in the hospital was 7 days for all procedures as well as for the 11 total joint arthroplasty procedures.
In this series, 57.5% of patients received a transfusion during their admission. The average intraoperative blood loss for the total hip arthroplasty and total knee arthroplasty cases in our series were 226 ml and 125 ml respectively. Among patients who received a transfusion, 46% received more than 4 units of PRBC or FFP. Patients receiving more units of blood were associated with larger operations such as hip arthroplasty. No patients experienced a thromboembolic event within 6 months postoperatively.
Most procedures occurred under general anesthesia (70%) (Table 1). Immediately following surgery, 13% of patients were transferred to the intensive care unit. One patient passed away during their hospitalization. A palliative care consultation occurred for 49% of patients during the hospitalization. The most consulted specialty during their hospital admission was cardiology at 28 consults total. The second and third most consulted specialties were palliative and medicine at 23 and 12 consults respectively.
For all procedures, 47% of patients either visited the emergency department (ED) or were readmitted to the hospital within 7 days. Further follow up information is provided in Table 1. Of the 40 patients included in the study, 34 patients (85%) were deceased by time of data collection. The average time from LVAD installation to death was 5.5 years (2023 days).
CONCLUSION
Our study examined patient outcomes in individuals with implanted LVAD who undergo orthopedic surgery. To the best of our knowledge, this is the largest case series in orthopedic surgery for this patient population. Our study found a low 30 and 90-day morbidity, with patients on average surviving 3.5 years after orthopedic surgery and no thromboembolic events within 6 months postoperatively. However, we did find a higher rate of blood transfusion, readmission, longer length of stay, and discharge to rehab compared to previously reported literature.14,16–18
Rosenberg et al published a retrospective case series in 2023 on total joint arthroplasty (TJA) in patients with LVAD device.14 Their study included 5 patients undergoing 12 surgeries with 7 primary arthroplasties and 5 revisions. Average length of stay was 10.4 days compared to the institution average of 1.8 days. All patients suffered a bleeding or thrombotic event. 75% of surgeries required intraoperative transfusion, compared to the approximately 19% of primary TJA patients in literature. Two patients died from thrombotic events, most likely unrelated to surgery, and three progressed to heart transplantation. They concluded that patients who undergo orthopedic surgery with an LVAD have a longer length of stay, increased transfusion risk, and higher risk of thrombotic events.
Two other case reports exist in the orthopedic literature describing patients with an LVAD. In 2013, Leonard et al published a case report about two patients with LVAD undergoing total knee arthroplasty (TKA).19 One patient was hospitalized after discharge for recurrent GI bleeding related to chronic warfarin usage and developed a LVAD driveline infection 14 months after his TKA, without infection of hardware. The second patient underwent an open reduction internal fixation (ORIF) of left intertrochanteric fracture and TKA 2 weeks later. He was re-admitted twice after discharge for GI bleeding and also developed methicillin-resistant Staphylococcus aureus bacteremia 7 months after TKA. Similarly, in 2014, a case report by Walton et al reported on a total hip arthroplasty performed in a 64-year-old male patient with LVAD.12 The patient underwent an elective total hip and required a postoperative transfusion for acute blood anemia.
More than half of patients in our study required a blood transfusion, despite the relatively low blood loss. This appears to be towards the higher requirement of orthopaedic surgery, as the reported range for blood transfusion in patients undergoing total hip or knee arthroplasty, considered large-scale orthopaedic surgeries, ranged from 19-57%.20 This may be from patients with an LVAD requiring long term anticoagulation, leading to higher rates of acute blood anemia and lower reserve, necessitating blood transfusion. Previous reports have noted a significant variability in blood transfusions among patients due to lack of agreement in triggers for a blood transfusion.21 Tranexamic acid dose, drain use, and operating time have been identified as risk factors for blood transfusion likelihood and may explain the higher percentage of patients receiving blood transfusion in this study.22
Based on the Elixhauser Comorbidity Score and ASA criteria, the patients in our study can be deemed higher risk patients. An Elixhauser Comorbidity Score of >15 was recently linked with a 1-year mortality of 38% and therefore the highest risk tertile of patients.23 Furthermore, our average patient’s ASA score implies severe systemic disease and/or such a disease with a constant threat to life.24 Nonetheless, the vast majority of our patients were able to recover in the PACU immediately after surgery. Additionally, we found a low 30 and 90 morbidity with only 1 patient expiring during admission. The morbidity and mortality rates in our series are important to acknowledge as highest risk patients may be given nonsurgical treatment of a typically surgical diagnosis such as hip fracture if their surgical risk was considered too high. This series demonstrates that patients with LVAD can be considered for necessary surgical treatment when optimized and a risk/benefit analysis is discussed with the patient.
While decreased length of stay has been shown to decrease cost with stable readmission rates in the general population undergoing total joint arthroplasties, our study found a longer operation time and length of stay in patients with LVAD undergoing primary total joint arthroplasties. A previous study of primary total hip arthroplasty reported a mean operation time and intraoperative blood loss of 39 ± 13 minutes and 259 ± 173 ml respectively.25 Moreover, in a 2020 study by Morco et al, the mean operation time for total knee arthroplasties was found to be 92 minutes with operation times greater than 90 minutes associated with higher odds of 30-day complications.26 Length of stay for total joint arthroplasties was reported to be 3 to 4 days with less than 2 days safe for certain patient populations.16 In contrast, our study of patients with LVAD experienced operation time of 163 minutes for total hip arthroplasty and 145 minutes for total knee arthroplasty and an average length of stay of 7 days.
Approximately half of our patients were discharged with assistance including acute rehabilitation, skilled nursing, long term acute care, home healthcare, or short-term hospital stays. This appears to be a sizeable proportion of patients discharged with assistance. In contrast, a recent study reports that 87% of elective total hip arthroplasty patients were discharged home while only 13% were discharged to non-home location.27 This emphasizes the need for these complex patients to have coordinated multidisciplinary care, including with social work and case management. This may also contribute to our finding of longer length of stay, as coordination of placement and bed availability in rehab can lead to longer length of hospital stay.
Emergency department visits and readmissions to the hospital for our study’s patients appears to be higher than the average. A meta-analysis study from 2015 considering 24 separate studies determined that the readmission rate across all orthopaedics is 5.4%, with no significant differences between subspecialties.28 This is an important consideration, especially in procedures such as total joint arthroplasty with bundled care payments, these patients are likely to have readmission and ER visits.
There are several limitations to this study including its retrospective nature, wide variety of procedures, and variation in surgeons. Given the retrospective nature of this study, data was recorded for non-research purposes and thus only captures certain data. Information such as antibiotic, tranexamic acid use, and drain use were not available for all patients in this dataset and record keeping accuracy could not be controlled. Additionally, this study included a wide variety of procedures and surgical approaches, with different surgeons listed, which may limit the comparability and generalizability to other clinical settings.
Our retrospective case series examined 47 orthopaedic surgeries in 40 LVAD patients who underwent their orthopedic procedure between 2012 and 2022. LVAD patients appear to be a higher risk population for orthopedic surgery and have longer hospital length of stay and transfusion requirements. Consistent with the increased risk, these patients appear to have a greater need for post-discharge rehabilitation assistance, more frequent emergency department visits, and more frequent hospital readmission. However, we found low 30 and 90-day morbidity and no thromboembolic events within 6 months postoperatively, showing that with coordinated care and planning, orthopedic surgery can be done safely in this complex patient population.
Author Contribution Statement
A.H. and A.R. conceived of the presented idea. L.Q., V.K., J.M. collected the data and wrote the initial manuscript. A.O. and B.P. completed data abstraction and statistical analysis. A.H. and A.R. supervised the project and edited the manuscript. All authors discussed and contributed to the final manuscript.
Ethical Review Committee Statement
The IRB determined that this study meets the criteria for exemption from IRB review. See exemption determination letter.
Conflicts of Interest Statement
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
Funding Declaration
No funding was received for conducting this study.
Data Availability Statement
The data that support the findings of this study are not openly available due to reasons of privacy and are available from the corresponding author upon reasonable request.
Acknowledgments
We thank CQODE (Clinical Quality, Outcomes, Discovery, and Evaluation Core) for their support with data abstraction for this project.
Investigation performed at the Department of Orthopaedic Surgery, University of Minnesota