Introduction
Coronal plane fractures of the distal femoral condyle were first described by Friedrich Busch in 1869.1 Later, Albert Hoffa further defined this fracture pattern, using Busch’s illustration.2 Although the fracture historically has been referred to as a ‘Hoffa fracture’, authors now advocate for a more appropriate nomenclature, using the term ‘Busch-Hoffa fracture’.3 Lateral Busch-Hoffa fractures are more frequent than medial. This is believed to be due to the constitutional valgus alignment of the lower limbs.4 Although the mechanism of injury is often high velocity trauma, sports injuries and low velocity trauma have also been reported in children.5–7 A lack of blood supply to the separated fracture fragment in Busch-Hoffa fractures renders the posterior femoral condyle prone to non-union and avascular necrosis. Furthermore, Busch-Hoffa fractures are considered to be inherently unstable.3 Therefore, surgical fixation of the fracture is viewed as the golden standard of treatment.
Busch-Hoffa fractures are uncommon in adults and even more so in the pediatric population, with only 20 cases reported currently in literature.4–23 Several authors who reported on pediatric Busch-Hoffa fractures have attempted to include a literature review.5,12,14,19 However, no systematic review has been done. In addition, we report on a case of pediatric lateral Busch-Hoffa fracture associated with a bucket handle tear of the lateral meniscus and popliteus tendon incarcerated in the fracture, a pattern unique to the literature.
Systematic review
Methods
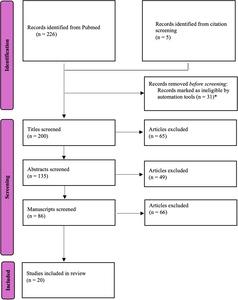
A search of the Pubmed/Medline database was performed in February 2025. The search term used was ‘Hoffa fracture’. Although the scope of the study was pediatric Busch-Hoffa fracture, we intentionally avoided too specific search terms to keep the initial search as broad as possible to prevent unintentional exclusion of relevant articles. This search identified 226 articles. Automation tools to select for full text-articles and articles written in the English language were used and this yielded an exclusion of 31 manuscripts. To increase the likelihood of identifying all relevant studies, the reference lists of all retrieved articles were hand searched. All remaining titles (n=200) and consecutively abstracts (n=135) and manuscripts (n=86) were critically reviewed by the primary author for the following inclusion criteria: coronal fracture of the posterior femoral condyle and patients aged 16 years or younger. Articles were excluded if the diagnosis was a mere osteochondral fracture or if they reported on case series including pediatric patients but without a separate analysis of the pediatric population. A flowchart of the search strategy is depicted in Figure 1. The systematic review of the literature was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA).24
Quality assessment of all eligible papers was performed using the McMaster Critical Review Form for Quantitative Studies and guidelines.25
All included articles were assessed for information on patient characteristics including gender and age, fracture location, mechanism of injury, associated injuries, used treatment method, duration of follow-up and results of treatment at final follow-up. Descriptive statistics were used to synthesize and present the data.
Results
The search yielded 20 articles eligible for inclusion (Table 1). Although three papers were considered for exclusion after quality assessment due to lack of reporting on sample characteristics (gender not specified (n=2) and no information on mechanism of injury (n=1)), no papers were excluded eventually as we believe that gender nor mechanism of injury are critical factors in the assessment and treatment of Busch-Hoffa fractures.
All studies were case reports and therefore level V evidence. Average age of all 20 patients was 11.35 years (range 5-16). Out of 18 patients, 12 were male (66.7%) and six were female (33.3%). The gender was not specified in the two remaining cases. Medial Busch-Hoffa fractures were found in eight patients (40%), lateral fractures were present in seven patients (35%) and bicondylar fractures in five (25%). Six patients sustained a motor vehicle accident (30%); eight were due to a fall on the knee (40%) and three patients suffered a non-contact sports injury (15%). Reported associated osseous injuries were ipsilateral lateral femoral condyle fracture in addition to a conjoint bicondylar Busch-Hoffa fracture, ipsilateral fibular fracture and Salter-Harris type 2 distal femoral fracture. There were two soft tissue injuries (patella tendon rupture and peroneal nerve palsy) and one case of intra-articular patellar dislocation. Three papers reported on missed Busch-Hoffa fractures with late diagnosis.
Nearly all patients were treated with open reduction and internal fixation (ORIF) (85%). Full arthroscopic fixation was performed in two cases (10%) and arthroscopically assisted fixation was used in one patient (5%).
Clinical and radiographic outcomes as described in all papers are depicted in Table 1. No patients required unplanned return to the operating room. Apart from one premature physeal growth arrest resulting in a leg length discrepancy of 15mm and one fixed flexion deformity (FFD) of 5°, all patients are reported to have good results after an average follow-up of 18 months (range 3-40 months).
Case presentation
Ethical considerations
After consulting the Ethical Committee associated with CHI at Crumlin, Dublin, no ethical approval was required as this research paper consists of a single case report. Consent for submission for publication of information of the child was given by the mother.
Case presentation
A 7-year-old girl sustained an injury to the left knee after falling off her bicycle. She described the trauma mechanism as a direct impact to the anterior aspect of the knee with the knee in a semi-flexed position. She experienced immediate swelling of the knee but was able to bear weight. The patient presented to the emergency room five days post injury due to persistent knee swelling and an inability to fully extend her knee.
Clinical examination of the left knee revealed a large knee effusion associated with a restricted range of motion (ROM). There was a FFD of 40° and a flexion of 90°. Straight leg raise was intact, but she had a significant extensor lag. The lateral joint line was tender on palpation. Hip and ankle examination of the ipsilateral side was normal. While she was able to weight bear her gait was severely impacted.
Initial lateral knee plain radiograph confirmed a large joint effusion with what looks like an associated rim of calcification posteriorly, while the anteroposterior (AP) radiograph was essentially normal with only subtle calcification around the lateral femoral condyle. (Fig 2)
Further imaging included a magnetic resonance imaging scan (MRI), followed by a computed tomography (CT) scan to aid pre-operative planning. MRI confirmed a Busch-Hoffa fracture of the lateral femoral condyle with an associated lateral meniscal bucket handle tear. CT scan showed the extent and the orientation of the condylar fragment. (Fig 2)
The patient underwent arthroscopic assisted open reduction and internal fixation of the Busch-Hoffa fracture with concurrent repair of the lateral meniscal bucket handle tear. Prior to incision, examination under anesthesia was performed to assess ligamentous stability which revealed no ligamentous injury. However, there was a FFD of 40° with flexion only to 95°.
Arthroscopy revealed an irreducible bucket handle tear of the lateral meniscus. Visualization of the Busch-Hoffa fracture was not possible at this stage (Fig 3). A lateral approach to the knee was performed utilizing the interval between biceps femoris and the iliotibial band. Care was taken to protect the common peroneal nerve. The posterolateral capsule was exposed and an arthrotomy was performed. Capsular stay sutures aided retraction and exposure (Fig 3). The fracture fragment was identified and it was noted that a partially torn popliteus tendon was incarcerated in the fracture site (Fig 4). The popliteus tendon was removed from the fracture site and the fracture fragments were reduced anatomically. Two 2mm headless compression screws were used to stabilize the fracture. Subsequently, arthroscopy was resumed, and reduction of the lateral meniscal bucket handle tear was now possible. This was repaired with two all-inside sutures.
Arthroscopy also revealed an area of chondral damage, at the level of the fracture line, for which micro-fracturing was performed. Reassessment of the patients ROM revealed flexion to 130° with an FFD of only 20°. Closure was performed in consecutive layers and the patient was placed in a hinged knee brace locked in 30° flexion. Postoperatively, the patient remained non-weight bearing for approximately six weeks with range of motion exercises starting two weeks post procedure. At five-month follow up this patient had full ROM and was mobilizing pain-free. She had returned to all regular daily activities including running and jumping comfortably. On examination there was no leg length discrepancy or angular deformity, and ROM was fully restored (0° to 140°) (Fig 5). Radiographs at 7 months postoperatively showed good alignment with no obvious physeal injury (Fig 5).
Discussion
Busch-Hoffa fractures are rare, especially in the pediatric population. As currently available literature exists only of case reports, we aimed to provide an updated summary of all currently available literature to aid diagnosis and management. Furthermore, we provide a unique addition to existing literature as we are the first to report on a pediatric lateral Busch-Hoffa fracture associated with a lateral meniscus tear and incarcerated popliteal tendon in the fracture site.
Lateral Busch-Hoffa fractures are assumed to be more prevalent than medially located posterior femoral condyle fractures, possibly due to the constitutional valgus alignment of the lower limbs.4 This is confirmed by Neumann-Langen et al in their retrospective review of 56 cases of Busch-Hoffa fractures with a rate of 83% lateral and 16% medial Busch-Hoffa fractures.26 Although this systematic review reports a nearly equal rate of lateral and medial Busch-Hoffa fractures, no conclusions on incidence of fracture location can be made based on a series of case reports alone. Fall, landing directly on the knee, was the main mechanism of injury, closely followed by motor vehicle accidents. However, sports injuries, including non-contact twisting injuries, are also reported as the cause of a Busch-Hoffa fracture in the skeletally immature population.5–7
As Busch-Hoffa fractures are intra-articular fractures in the coronal plane which are subject to shearing forces, they are considered to be inherently unstable.3 Furthermore, the posterior femoral condyle lacks soft tissue attachments, which renders it prone to non-union. Therefore, anatomical reduction and stabilization is typically advised. The available literature indicates that open reduction and internal fixation is still preferred in adults.3,26 This systematic review confirms the same standard of care is used in the pediatric population. We believe arthroscopy can be of additional value in the assessment and treatment of possible concomitant soft tissue injuries, as illustrated by this case. However, the Busch-Hoffa fracture itself is oftentimes difficult to assess or reach with arthroscopy alone and therefore necessitates an open approach. As anatomical reduction and stable fixation of the fracture are critical, we feel this should not be compromised in favor of less invasive techniques.
Although subject to publication bias, the sparse available literature indicates that patients with Busch-Hoffa fracture can expect good short-term outcomes. All papers who included pain as outcome parameter reported pain-free children at final follow-up, apart from one who reported sporadic bilateral knee pain but who was able to return to playing baseball and soccer. Furthermore, reported ROM assessments show adequate range of motions in all patients with only one FFD of 5°. Sixteen papers reported on radiographic outcome parameters with an average follow-up of 18 months. All radiographic outcomes were satisfactory except for one premature physeal arrest which resulted in a leg length difference of 15mm. No patients in the reported literature had an unplanned return to theatre. There are no long-term follow-up studies and thus the eventual prognosis of this injury and the implications of the interruption of blood supply to the femoral condyle remains an open question.
Our case contributes to the existing literature as it is the first to report on a pediatric lateral Busch-Hoffa fracture associated with a bucket handle tear of the lateral meniscus and incarcerated popliteus tendon in the fracture site. Concomitant meniscus tears with a Busch-Hoffa fracture have been reported in the adult population but are rare.26,27 Neumann-Langen reported an incidence rate of 5.4% of these soft tissue injuries in Hoffa fractures in adults.26 However, no similar association has been reported on in the pediatric population.
Conclusion
Pediatric Busch-Hoffa fractures are a rare and sometimes technically challenging entity. We are the first to report on a lateral Busch-Hoffa fracture in a pediatric patient, combined with lateral meniscus tear and popliteus tendon incarcerated in the fracture. The sparse available literature indicates that patients can expect good radiological and functional outcomes, although this perspective must be tempered due to inherent publication bias and the lack of any adequately sized prospective studies. As the pediatric literature is entirely composed of single case reports, further research is required to inform the management and prognosis of this injury.
Corresponding author
Tine De Mulder
tinedemulder@gmail.com
0838052885
- Department of Orthopaedic Surgery, Children’s Health Ireland at Crumlin, Cooley Road, Crumlin, Dublin, D12 N512, Ireland.
- School of Medicine, Trinity College Dublin, 152-160 Pearse Street, Dublin 2, Ireland.
- School of Medicine, University College Dublin, Belfield, Dublin 4, Ireland.
Acknowledgments
We would like to thank the Research & Audit Team from the Orthopaedic Departments in CHI at Crumlin, Ireland, for their contributions to this research project.
Authors’ contributions
Tine De Mulder (author); Adanna Welch-Phillips (author); Muhammad Mosri (author); Jim Kennedy (author); Patrick O’Toole (author)
Disclosures
None
Acknowledgments
We would like to thank the Research & Audit Team from the Orthopaedic Departments in CHI at Crumlin, Ireland, for their contributions to this research project.

_radiographs_at_presentation_of_left_knee_(a)_anteroposterior_view_(b)_lateral_view._2)_.png)
_irreducible_lateral_meniscus_tear_with_the_busch-hoffa_fractu.jpeg)

_clinical_photographs_showing_range_of_motion_eight_months_after_surgery_(a)_knee_extens.jpeg)

_radiographs_at_presentation_of_left_knee_(a)_anteroposterior_view_(b)_lateral_view._2)_.png)
_irreducible_lateral_meniscus_tear_with_the_busch-hoffa_fractu.jpeg)

_clinical_photographs_showing_range_of_motion_eight_months_after_surgery_(a)_knee_extens.jpeg)