Introduction
Femoral Intramedullary Screw Fixation is a surgical procedure designed to stabilize a fractured femur through the insertion of a metal rod, commonly referred to as a nail into the marrow canal of the bone. The rod is subsequently secured with screws to ensure proper stabilization. This procedure is frequently recognized as the standard care for femoral shaft fractures for several reasons. It is characterized as a minimally invasive procedure technique that necessitates a small incision and entails less dissection of adjacent soft tissues in comparison to plate fixation.1 The intramedullary nail provides robust internal stabilization of the fracture, aligning the fractured bone fragments and facilitating early mobilization and weight-bearing, which are critical for muscle function and recovery. Research indicates that intramedullary nailing correlates with an improved range of motion in the hip and knee joints following, thereby enhancing the patient’s long-term quality of life.2 Furthermore, it is associated with lower complication rates when compared to plate osteosynthesis, as it significantly reduces the risks of infection, implant failure, and the need for reoperation.3
The common patient demographics for femoral intramedullary screw fixation predominantly encompass elderly individuals. Femoral intramedullary screw fixation is most common in elderly patients (average age ~77 years, 90% > 65 years), with proximal femur fractures occurring predominantly in females, who are nearly three times more likely to sustain these injuries compared to men.4 Although there exists a broad age spectrum, ranging from adolescents to the elderly, for femoral shaft fractures, the majority of patients undergoing treatment for proximal femur fractures with intramedullary screw fixation are female.5 Comorbid conditions such as hypertension, diabetes, osteoporosis, and chronic lung disease are highly prevalent in this demographic. By contrast, younger male patients, typically in their 20s to 30s (average ~33 years), sustain femoral shaft fractures mainly from high-energy trauma like motor vehicle accidents, and intramedullary fixation remains the standard treatment.6 Intramedullary screw fixation is frequently employed in cases of subtrochanteric, intertrochanteric, and basicervical femoral neck fractures, in addition to serving as the standard treatment for shaft fractures.7 In younger populations suffering from femoral shaft fractures, the mean age approximates thirty-three years, with motor vehicle accidents representing the most prevalent cause of trauma.8 Although demographic profiles vary depending on the specific fracture type, intramedullary fixation is commonly utilized in older predominantly female patients with proximal femur fractures. Nevertheless, it remains a prevalent intervention for shaft fractures, which may occur at a young age, predominantly affecting males due to high-energy trauma.9
Acute kidney injury (AKI) constitutes a sudden loss of excretory renal function. It transpires when the kidneys are incapable of effectively filtering waste products from the bloodstream, resulting in toxins and fluids in the body. The condition may develop within a span of hours or days and necessitates prompt medical intervention to avert serious complications.10
Dialysis constitutes a medical intervention designed to eliminate waste products and excess fluid from the bloodstream in instances where the kidneys are incapable of performing this function. This procedure entails circulating the blood through a machine or filter, which removes these substances, thereby functioning as an artificial kidney. Such a process is instrumental in maintaining the body’s fluid and electrolyte equilibrium, thus preventing the harmful accumulation of toxins and metabolic waste.11
AKI is a serious and frequent complication for hospitalized patients, significantly impacting patient outcomes such as increasing mortality. The risk of mortality rises with the severity of AKI. For example, an analysis of hospitalized children shows in-hospital mortality rates of 8.19% for stage 1, 13.44% for stage 2, and 27.78% for stage 3.12 This also prolongs the hospitalization and correlates with the severity of AKI. Due to extended stays, hospital costs naturally increase.13
Though rare, acute kidney injury (AKI) and dialysis after orthopedic surgery carry significant clinical and cost implications, including increased mortality, longer hospitalization, and higher health care cost.14 Though low, these complications are of interest since they have outcome impact.15 Although acute kidney injury (AKI) is well-defined among patients undergoing general surgery, as well as those with cardiac and critical illnesses, there exists limited information regarding its prevalence following orthopedic procedures such as femoral intramedullary screw fixation. This issue is particularly pertinent, given that orthopedic patients, notably the elderly, are frequently at heightened risk for renal complications.
The National Surgical Quality Improvement Program (NSQIP) database provides a valuable resource to address this knowledge gap. It is a risk-adjusted, validated database based on multiple sclerosis (MS) data collection, which contains complex comprehensive perioperative and postoperative information from various hospitals.
The objective of this study is to ascertain the incidence and identify predictors of AKI and the necessity for dialysis following femoral intramedullary screw fixation, utilizing data from NSQIP to enhance risk stratification and perioperative management strategies.
Methods
The study employed the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database, a highly validated, risk-adjusted, outcomes-oriented clinical registry comprising data from over 700 United States hospitals. The database is de-identified and curated by trained clinical reviewers, ensuring rigorous standards of data quality and completeness.16
A cohort of adult patients aged 18 years and above, who underwent femoral intramedullary screw fixation (Current Procedural Terminology (CPT) code 27506) between January 1, 2018 and December 31, 2022, were selected for analysis. Patients with missing essential preoperative variables or outcome data were excluded to preserve the integrity of the cohort.
The primary outcomes examined were postoperative acute kidney injury (AKI) and the incidence of dialysis within thirty days following surgery. AKI was defined following NSQIP criteria, either as a postoperative increase in serum creatinine levels or the requirement for dialysis.
Independent variables included demographic data such as age, sex, and body mass index (BMI). The study also includes comorbidities such as diabetes, hypertension, smoking status at the time of surgery, pre-existing dialysis, and preoperative AKI. Laboratory findings considered were preoperative serum creatinine blood urea nitrogen, and hematocrit levels. Operative parameters encompassed the American Society of Anesthesiologists (ASA) classification, operative duration, and type of anesthetic administered.
Initially, univariate logistic regression analyses were performed to assess the association between each predictor variable and the outcomes of AKI and new dialysis. Variables with p-values less than or equal to 0.05 were then subsequently included in a multivariable logistic regression model to identify independent predictors.17 This model yielded adjusted odds ratios along with 95% confidence intervals. Variance inflation factors were calculated to detect potential multicollinearity, while model discrimination was evaluated using the c-statistic (area under the curve, AUC) and R2.18 All statistical analyses were conducted with a two-tailed hypothesis, with significance established at α = 0.05.
In accordance with federal guidance (45 CFR 46) and ACS-NSQIP data use policies, our institution (Brown University) reviewed the project and issued a Non-Human Subjects Research determination because no identifiable private information was used. Accordingly, formal IRB approval and informed consent were not required.
Results
Patient Characteristics
Utilizing the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database, we appropriately reviewed 42,644 patients with femoral intramedullary screw fixation from the time 2018 to 2022. Hypertension on therapy, diabetes, obesity, and smoking were the most frequent comorbidities. The majority of patients were ASA class 2 or ASA class 3, and a few were ASA class 4. General anesthesia was the most utilized anesthetic, followed by spinal and regional blocks.
Univariate Analysis
In univariate analysis, several factors were found with increased risk of postoperative AKI or dialysis. The most significant among them was preoperative renal failure. Female sex, hypertension, ASA Class, BMI, and longer operation time were also significantly related to renal complications. Diabetes, smoking, and type of anesthesia were not statistically significantly associated with AKI or dialysis when they were analyzed independently.
Multivariate Analysis
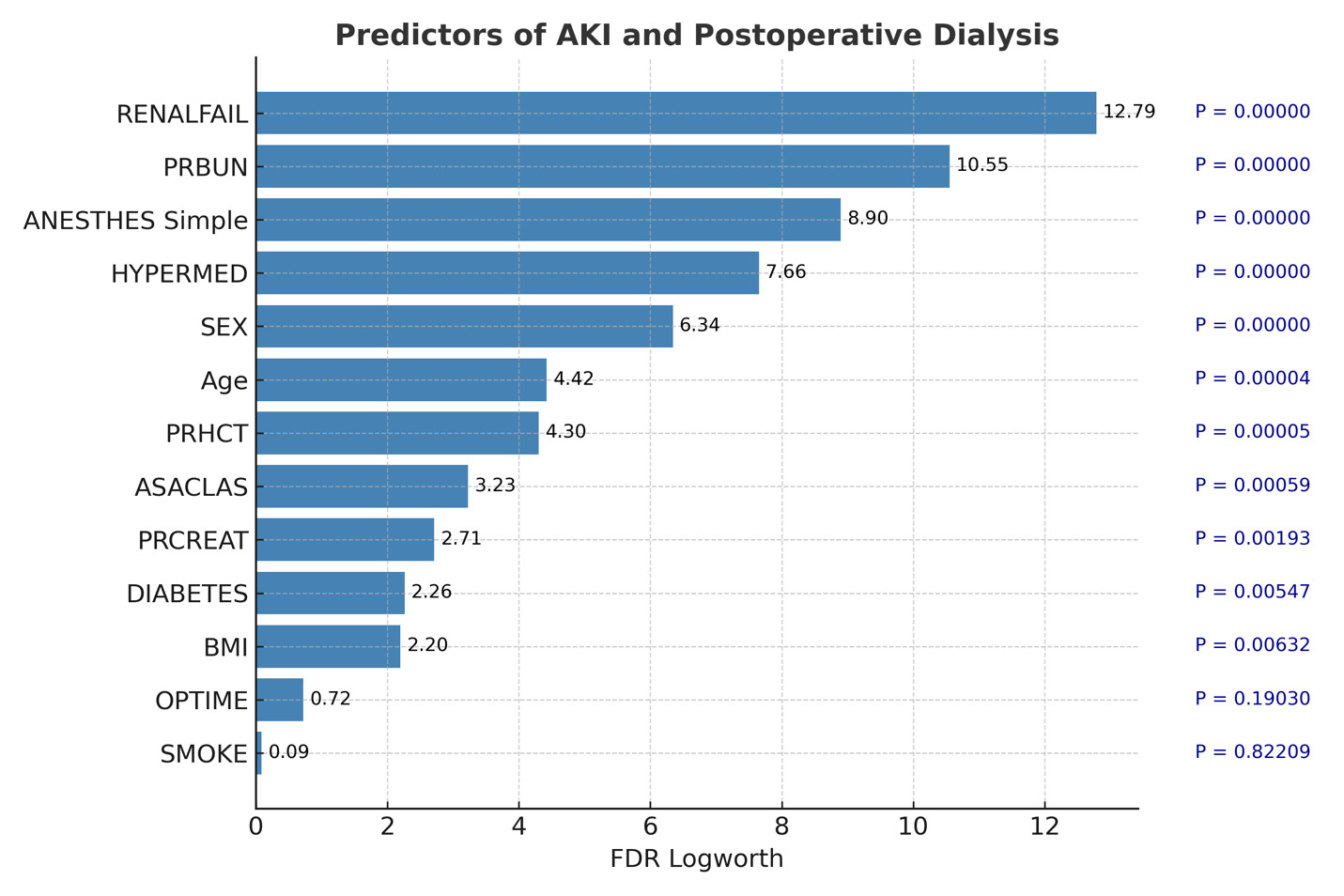
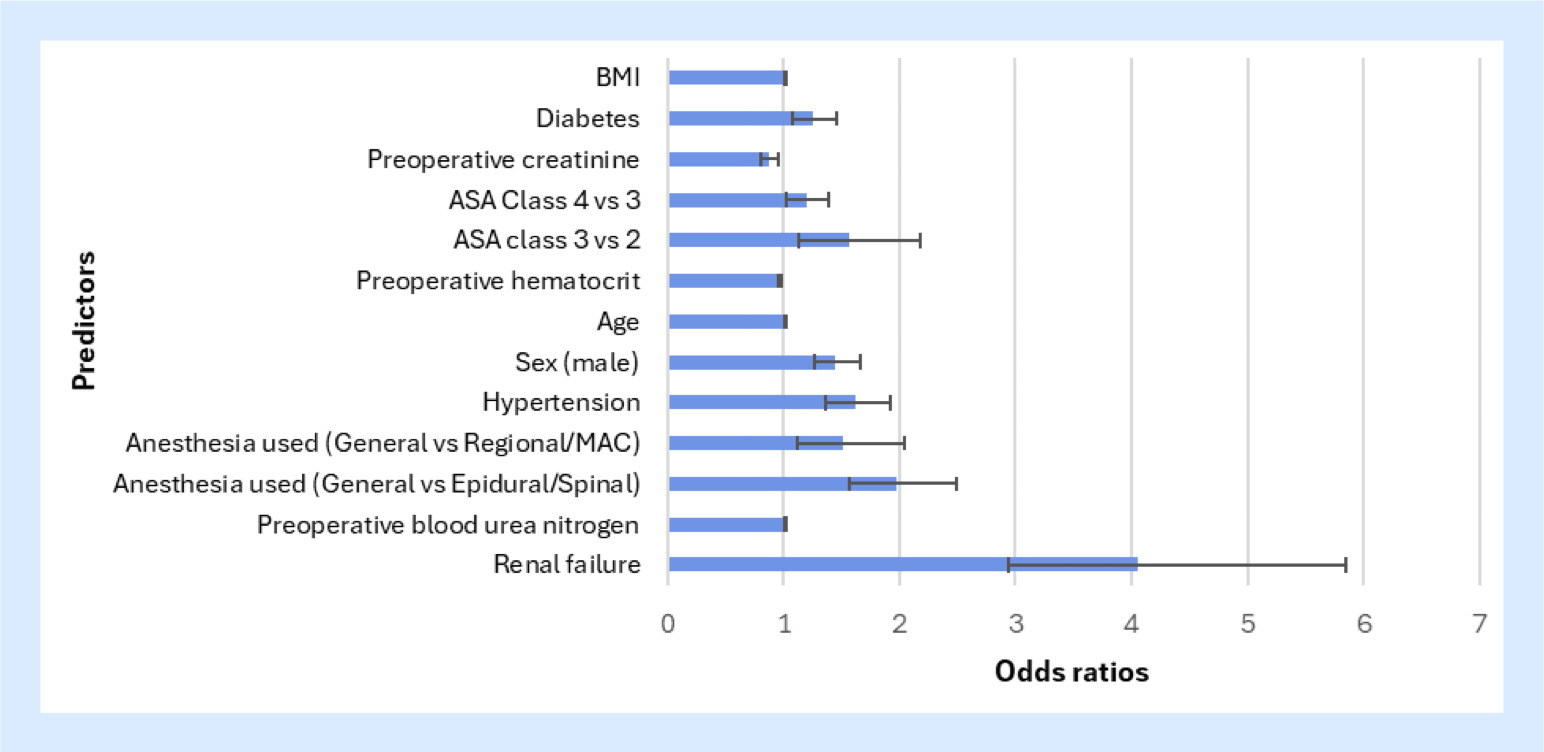
Several categorical predictors independently associated with postoperative renal insufficiency were identified by multivariable logistic regression analysis (Figure 1). Preoperative renal failure was the strongest predictor with an odds ratio (OR) of 4.048 (95% confidence interval (CI) of 2.935-5.584, p<0.0001). ASA classification also produced a dose-response effect: ASA Class 4 patients had an OR of 1.77912 (95% CI: 1.3619–2.3241, p < 0.0001), and ASA Class 3 had an OR of 1.48954 (95% CI: 1.1690–1.8878, p = 0.0013), both compared to ASA Class 2. Figure 2 and Figure 3 provide the raw data collected from the multivariate analysis showing these results.
Hypertension requiring medication had 62% greater odds of developing postoperative renal insufficiency compared to those without, with an odds ratio (OR) of 1.6226 (95% CI: 1.3688-1.9234, p=0.0001). Male patients had 45% higher odds than females (OR=1.4484, 95% CI; 1.2626-1.6615, p=0.0001). The type of anesthesia was also a significant predictor: patients who received general anesthesia had nearly double the odds of renal complications compared to those who received spinal anesthesia (OR=1.9715, 95% CI: 1.5618-2.4886, p=0.0001). Preoperative hematocrit was also a significant factor, with lower hemoglobin levels being significantly associated with postoperative AKI.
Diabetes was also independently associated with a moderate increase in risk (OR=1.2516, 95% CI: 1.0752-1.4569, p=0.0038). In contrast, as seen in Figure 8, smoking status was not statistically significant in this model, (p=0.8225), indicating no meaningful difference in risk between smokers and nonsmokers after adjusting for other variables.
Other factors with a significant impact on the likelihood of postoperative renal insufficiency include BMI and operative time. With each one-unit rise in BMI, there was a 1.56% increase in the odds of renal insufficiency (OR= 1.0156, 95% CI: 1.0049–1.0264, p = 0.0003). Similarly, operative time had an odds ratio of 1.0011 per minute (95% CI: 0.9995-1.0027, p=0.12). While the per-minute effect was modest and did not reach conventional statistical significance, the overall effect on longer procedures remains clinically important. Figure 2 summarizes the unit odds ratios for factors that significantly impact postoperative dialysis and AKI.
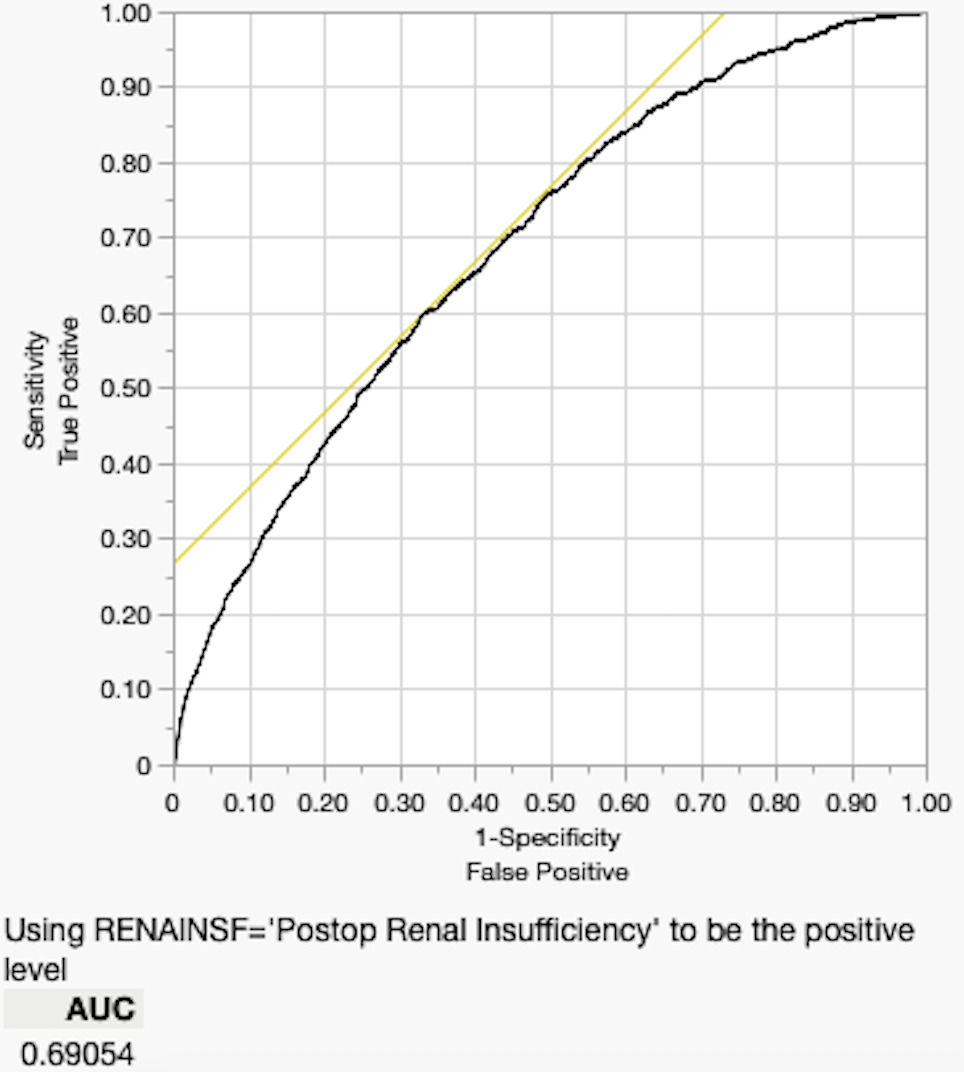
Model discrimination was assessed with the ROC curve, which yielded an area under the curve (AUC) of 0.69054, indicating acceptable predictive accuracy (figure 10). AUC values between 0.7 and 0.8 are considered acceptable for clinical risk modeling. The generalized R² of 0.0512 also suggests the model explains a modest proportion of the variability in renal inefficiency outcomes.18
These findings imply that patients with preoperative renal insufficiency, ASA grade, or hypertensive comorbidity are at greater risk for postoperative AKI or dialysis after femoral intramedullary screw fixation. Preoperative identification of high-risk patients may be beneficial in identification of these patients who would need more intensive renal-monitoring and management plans intraoperatively as well as in the postoperative period to decrease resultant complication rates.
Discussion
The aim of this research was to identify predictors of postoperative renal insufficiency, such as dialysis and acute kidney injury (AKI), in femoral intramedullary screw fixation patients. From a large, multi-institutional database of the American College of Surgeons NSQIP, we found preoperative renal failure to be the most important independent risk factor for postoperative renal compilations. Other significant predictors included higher ASA class, hypertension, use of general anesthesia, higher preoperative BUN, and greater BMI. While longer operative time was approaching significance, it did not achieve the classic cut point in our multivariate model.
The aim highlights the significance of baseline renal function and comorbid burden in predicting postoperative outcome. Patients with preoperative renal failure had over four-fold greater odds of having renal complications compared to patients without renal disease. Altered preoperative BUN also independently predicted AKI or dialysis and suggests that even asymptomatic renal dysfunction may increase vulnerability to perioperative stress. These findings concur with previous literature demonstrating how impaired renal reserve enhances the risk of AKI, particularly in elderly or risk surgical patients.19 However, our study quantifies such correlations in the specific context of orthopedic trauma surgery with intramedullary fixation.
The effect of ASA classification demonstrated a clear dose-response relationship. ASA Class IV and Class III patients had notably higher odds of postoperative renal insufficiency compared to ASA Class II. This reinforces the correlation between physiologic reserve and susceptibility of the kidneys. ASA score, as a generalized indicator for frailty and comorbidity, can be useful in risk stratification and clinical decision-making, particularly when combined with more specific markers like preoperative renal parameters. Prior studies have also emphasized ASA class as a strong predictor of postoperative complications including AKI.20
One of the major and potentially modifiable risk factors identified was the anesthetic type. Those patients receiving general anesthesia have nearly twice the risk of renal complication compared to patients receiving spinal or regional blocks. The etiology of causality is not known, but possible reasons include heterogeneity of hemodynamic stability, renal perfusion pressures, and sympathetic tone during surgery. Earlier studies in non-orthopedic populations have also reported correlations between general anesthesia and AKI risk, but few have done so in the setting of femoral fixation. With such serious renal issues, potentially requiring ICU admissions, dialysis, and extended hospitalization, this finding is worthy of prospective investigation.
Another intriguing finding was the association of male sex with increased risk of renal complications. Men had approximately 45% higher odds of postoperative AKI or dialysis. This aligns with some proof of sex-based variations in renal perfusion, hormonal response, and postoperative inflammatory pathways. However, the literature remains mixed; some studies report male sex as an independent risk factor, while others do not.21
We further discovered that BMI, when handled as a continuous variable, also had a statistically significant effect on renal outcome after surgery. With every increase in BMI by a single unit, there was an increase in the odds of renal insufficiency by about 1.56%. Although the effect per unit is minute, the cumulative effect across the population’s distribution is clinically significant. Obesity has been associated with altered renal hemodynamics, increased oxidative stress, and low-grade chronic inflammation, all of which potentially could enhance risk of AKI. These findings are consistent with recent research showing obesity as a perioperative kidney injury risk factor, independent of overt renal disease.
Surgical duration correlated with renal risk by univariate analysis but failed to do so in multivariate modeling. Nevertheless, the clinical relevance of longer cases cannot be disregarded. Longer cases generally translate to increased complexity, greater blood loss, or greater duration of exposure to anesthesia, all of which may secondarily add to renal stress. Several studies have noted the prolonged operative time may contribute to AKI exposure anesthesia, extended anesthesia exposure and hypotension.22 While the per-minute odds ratio was minimal, the cumulative effect on longer cases could still be clinically relevant in frail or comorbid patients.
From a clinical perspective, these findings highlight the value of preoperative risk stratification and individualized renal-protective practice. In patients with existing renal insufficiency or high-risk profiles (e.g. ASA class IV, hypertension), prompt consultation with nephrology, optimization of renal-protective perioperative medications, and careful fluid management may reduce AKI or postoperative dialysis incidence. Spinal or regional anesthesia may offer a renal-protective benefit. Particularly in patients with borderline kidney function.23 Additionally, whenever feasible, regional or spinal anesthesia consideration may possess a renal-protective benefit, particularly in patients with borderline kidney function.
The analysis has several strengths. Being derived from a large, validated national database creates a high statistical power and generalizability to a broad surgical population. Standardized data definitions and collection protocols reduce measurement bias. Also, the potential to model both categorical and continuous predictors for risk allows for finer understanding of risk gradients.
However, several limitations have to be acknowledged. First, the analysis is retrospective which precludes one from making firm causal inferences. Second, although NSQIP provided great data regarding preoperative and perioperative characteristics, it is not highly specific regarding intraoperative variables such as fluid, vasopressor infusion, urine output, and exposure to nephrotoxic medications, all of which potentially affect renal outcomes. Third, postoperative creatine levels are not always reported, and our outcome definition may not be able to capture less severe stages of AKI. Finally, while our model exhibited good discrimination (AUC= 0.745), pseudo R² suggests the presence of other unmeasured variables that are involved in renal outcomes and have to be evaluated in future research.
Future validation in such findings in trials and additional investigation of variables such as intraoperative hypotension, contrast exposure, and recovery strategies would be valuable. Also of value would be investigation of long-term outcomes of postoperative AKI in such patients, including progression of chronic kidney disease, readmission, and functional impairment. More robust randomized trials comparing anesthetic choices approaches in high-risk orthopedic patients are also needed.24 Randomized pragmatic trials testing different anesthesia approaches among high-risk orthopedic patients can offer evidence about whether anesthetic technique change can avert renal complications.
In conclusion, this study determines independent predictors of renal insufficiency following femoral intramedullary screw fixation, such as modifiable risks such as the nature of anesthesia and BMI. These findings highlight the importance of stringent preoperative assessment and indicate areas of possible advantage for targeted renal-protective interventions in high-risk patients.
Conclusion
This study identifies significant independent predictors of AKI and postoperative dialysis in patients undergoing femoral intramedullary screw fixation. These risk factors include pre-existing renal insufficiency, anesthesia type, hypertension, male sex, older age, anemia, diabetes, and higher BMI. Preoperative risk stratification incorporating these factors may improve perioperative planning and reduce adverse renal outcomes.