1. Introduction
Developmental dysplasia of the hip (DDH) significantly increases the risk of osteoarthritis and accounts for up to 30% of total hip arthroplasty (THA) cases in patients under 40 years of age.1–3 In its most severe form, Crowe type IV DDH is characterized by complete dislocation of the femoral head and proximal migration exceeding 100%,4,5 often accompanied by pseudoacetabulum formation, limb length discrepancy greater than 4 cm, gait abnormalities, and chronic hip pain.6–9 THA in these patients remains technically demanding due to the need to restore the true hip center and correct severe femoral deformities while addressing soft tissue contractures.9–13
Historical studies have indicated that, without appropriate surgical management, relocating a chronically dislocated femoral head into the true acetabulum may result in acute limb lengthening exceeding 4 cm, which significantly increases the risk of neurovascular complications — particularly stretch-induced neuropraxia and sciatic nerve palsy.14–18 Therefore, to prevent excessive limb lengthening and facilitate safe reduction of the femoral head into the true acetabulum, a femoral subtrochanteric shortening osteotomy (SSO) is frequently indicated in total hip arthroplasty for Crowe type IV developmental dysplasia.19–23
SSO can be performed in various configurations (transverse, oblique, chevron, step-cut), with the transverse technique remaining the most commonly used due to its simplicity and reproducibility, despite offering less rotational stability and a smaller bone contact surface compared to other methods such as chevron or step-cut osteotomies, which provide more favorable conditions for consolidation, provided stable fixation is achieved.24–28 Ensuring stable osteotomy fixation is essential for promoting bone union and enabling early mobilization.16 In the context of THA, this task is complicated by the presence of a femoral stem occupying the medullary canal, leaving limited room for additional hardware. Cerclage cables, with or without cortical strut grafts,29,30 are often employed due to their technical simplicity. However, they provide limited resistance to torsional forces31 and have been reported to be associated with nonunion rates of up to approximately 5% in recent studies.32 Plate-and-screw constructs offer superior mechanical rigidity, especially when multiple locking screws are used, and have demonstrated higher union rates.33 Moreover, large or bulky implants not only increase the risk of soft tissue irritation,33 but may also contribute to stress shielding at the bone–implant interface, particularly when there is suboptimal contact or mismatch in mechanical properties between the implant and the surrounding bone.34 Therefore, the ideal stabilization method must ensure sufficient biomechanical support while minimizing surgical trauma and implant-related complications.
A derotational plate with angular stability has been developed for fixation during subtrochanteric osteotomy in patients with Crowe type IV dysplastic coxarthrosis. This construct provides more uniform load distribution, high stability, and strength under physiological stresses, surpassing traditional fixation methods in these parameters.35 In addition, it represents a solution adapted to local anatomical and economic conditions, offering high efficiency at an acceptable cost. However, despite the expanding use of this implant, the scientific literature still lacks sufficient data on its clinical effectiveness, safety, and practical applicability. The present study aims to address this gap by evaluating surgical techniques and early postoperative outcomes in patients with Crowe type IV hip dysplasia who underwent surgery with the use of a domestically produced derotational plate over a three-year period.
2. Materials and Methods
2.1. Study Design and Setting
This prospective cohort study was conducted at the National Scientific Center of Traumatology and Orthopedics named after Academician N.D. Batpenov (Astana, Kazakhstan), in collaboration with the Department of Traumatology and Orthopedics of Astana Medical University.
2.2. Ethical Considerations
All procedures involving human participants were performed in accordance with the ethical standards of the institutional and national research committees and with the principles outlined in the Declaration of Helsinki (2013 revision). The study protocol was reviewed and approved by the Local Ethics Committee for Biomedical Research (protocol No. 4, November 9, 2022). Written informed consent was obtained from all patients prior to enrollment. All patient data were anonymized, and confidentiality was strictly maintained in compliance with national legal and ethical standards
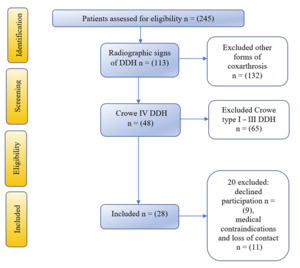
2.3. Patient Screening and Inclusion
Between December 2022 and January 2024, a total of 245 patients with symptomatic hip osteoarthritis were screened for eligibility according to the inclusion criteria. At the initial stage, all patients underwent standard anteroposterior pelvic radiography. In 132 patients, other forms of coxarthrosis not associated with developmental dysplasia of the hip (DDH) were identified, and therefore they were excluded from further analysis. The remaining 113 patients demonstrated radiographic signs of DDH. Among them, 65 patients were diagnosed with Crowe type I–III dysplasia, which also did not meet the inclusion criteria. In 48 patients, Crowe type IV DDH was confirmed, defined as complete proximal displacement of the femoral head by ≥100% of the height of the pelvis on the affected side. The diagnosis was established according to the original classification of Crowe et al.36 For a detailed assessment of individual anatomical characteristics and preoperative planning, additional standing radiographs of the lower limbs and computed tomography (CT) scans of the pelvic ring with the proximal femur were performed. These data were used to analyze femoral canal morphology and to determine the parameters of individualized osteotomy. Among the 48 patients with confirmed Crowe type IV dysplasia, 9 declined participation after receiving complete information regarding the study objectives, protocol, and potential risks. Another 11 patients were excluded due to identified medical contraindications (including acute inflammatory conditions, severe anemia, coagulation disorders), as well as loss of follow-up contact with the research team. Ultimately, the final cohort included 28 patients who fully met the eligibility criteria and provided written informed consent to participate in the study.
2.4. Implant Design and Manufacturing
A derotational plate with angular stability was used for osteotomy fixation. The implant was designed based on CT data and anatomical characteristics of patients with Crowe type IV developmental dysplasia of the hip, allowing the development of a universal construct. It was manufactured from medical-grade titanium alloy using computer numerical control (CNC) milling. The detailed methodology for the design and fabrication of this construct has been described in a previously published study.35
2.5. Preoperative Management
All patients underwent comprehensive clinical, laboratory, and radiological evaluation to confirm surgical eligibility and ensure precise preoperative planning. Radiological assessment included standard anteroposterior pelvic radiography, standing radiographs of the lower limbs to analyze limb length discrepancy and mechanical axis, as well as CT scans of the pelvis and proximal femur to evaluate individual anatomical features and plan the osteotomy. Preoperative functional status and symptom severity were assessed using the Harris Hip Score (HHS), Oxford Hip Score (OHS), and the Visual Analogue Scale (VAS) for pain. In accordance with national and international guidelines for the prevention of surgical site infections, all patients received antibiotic prophylaxis 30 minutes prior to skin incision.
2.6. Surgical Technique
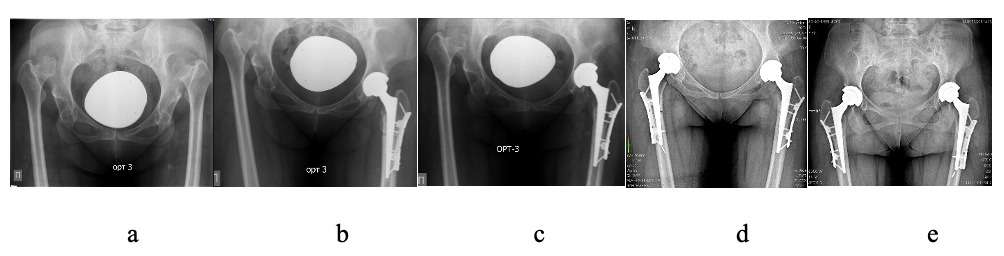
All surgeries were performed between December 2022 and January 2024 by the same experienced surgical team at the Republican Center for Large Joint Arthroplasty. Patients were positioned in the lateral decubitus position. A standard direct lateral (Hardinge) approach was utilized in all cases. Anesthesia was administered as either combined spinal-epidural or general anesthesia, depending on the patient’s preoperative condition and anesthesiologist’s evaluation. Following standard antiseptic preparation, a lateral skin incision approximately 16 cm in length (range, 15–18 cm) was made over the proximal femur. Layered dissection of soft tissues was performed to expose the hip joint. A hypertrophied joint capsule was identified, incised, and partially excised. The femoral head was dislocated, and femoral neck osteotomy was carried out, followed by complete removal of the head. A transverse femoral SSO was then performed approximately 1 cm distal to the lesser trochanter. The true acetabulum was sequentially reamed to the appropriate diameter, most commonly 44 mm. A press-fit, cementless hemispherical acetabular cup was inserted with 95–100% native bone coverage. In cases of deficient bone stock, one or two screws were placed through the cup for supplemental fixation. A polyethylene liner was inserted thereafter. Preparation of the femoral canal was initiated using dedicated rasps, beginning with the distal fragment to facilitate proper alignment of the proximal segment with the true acetabular center. After determining the appropriate implant diameter, the canal was sequentially reamed proximally. The overlapping bone segment was marked, and a second transverse osteotomy was performed to resect 2.5–6.5 cm of bone, based on intraoperative overlap measurement. A conical, cementless modular femoral stem was inserted via press-fit. After trial reduction and intraoperative assessment, patients with axial or rotational instability at the osteotomy site underwent plate osteosynthesis using a derotational plate. The plate was positioned on the lateral surface of the femur and secured using multiple angular stable locking screws in both the proximal and distal fragments to ensure stable fixation. The plate’s geometry provided controlled femoral anteversion and enhanced rotational stability. Final implantation of the femoral stem bridging the osteotomy was performed, followed by modular neck attachment and impaction of a cobalt-chromium femoral head. The femoral head was then reduced into the acetabular liner. The surgical site was irrigated, and wound closure was completed in layers without the use of bone grafts. Final intraoperative radiography confirmed optimal alignment, osteotomy compression, and appropriate implant positioning.
All 28 patients included in the study underwent the same standardized surgical technique, which consisted of a transverse subtrochanteric shortening osteotomy, implantation of a cementless conical femoral stem, and fixation of the osteotomy site with a derotational plate with angular stability. Postoperative management and rehabilitation protocols were also identical across the cohort. Variations in acetabular cup size, femoral head offset, or stem dimensions reflected individual anatomical differences rather than methodological differences in the surgical approach or fixation technique, thereby ensuring the internal consistency and comparability of the study results.
2.7. Postoperative Management and Follow-Up
During the first 24 hours after surgery, all patients were monitored in the intensive care unit (ICU) to ensure adequate pain control and surveillance of vital parameters. Intravenous antibiotic therapy was administered postoperatively in accordance with the institution’s internal infection control protocols. From the second postoperative day, patients began mechanotherapy and mobilization under the supervision of rehabilitation specialists, using walkers or crutches. Weight-bearing on the operated limb was restricted for the first six weeks, followed by a gradual transition to partial and then full weight-bearing, depending on radiographic evidence of osteotomy union.
Scheduled follow-up evaluations were performed at discharge and subsequently at 6 weeks, 3 months, 6 months, and 12 months after surgery. Functional outcomes were assessed using the Harris Hip Score (HHS), Oxford Hip Score (OHS), and the Visual Analogue Scale (VAS) for pain. Radiographic evaluations, including anteroposterior pelvic radiographs and lateral hip views, were performed to assess implant positioning and osteotomy healing. Radiographic assessments were conducted jointly by the operating surgeons and independent radiologists to ensure objective and accurate evaluation.
2.8. Data Analyses
Statistical analysis was performed using SPSS Statistics software. Quantitative variables were assessed for normality using the Shapiro–Wilk test. For variables with a normal distribution, data were described as mean (M) and standard deviation (SD), with 95% confidence intervals (95% CI) reported as a measure of representativeness. In cases of non-normal distribution, data were presented as median (Me) and interquartile range (Q1–Q3). Categorical variables were presented as absolute numbers and percentages. The 95% confidence intervals for proportions were calculated using the Clopper–Pearson method. For comparisons of three or more related samples with non-normal distributions, the Friedman nonparametric test was applied, followed by post hoc pairwise comparisons using the Conover–Iman test with Holm correction. For binary outcomes across more than two related groups, Cochran’s Q test was used, with post hoc analysis performed using McNemar’s test with Holm correction. Differences were considered statistically significant at p < 0.05.
3. Results
3.1. Patient Demographics
A total of 28 patients (30 hips) with Crowe type IV developmental dysplasia of the hip (DDH) were included in the study. The study population consisted of 22 women (78.6%) and 6 men (21.4%), with a mean age of 39.2 ± 11.6 years (range, 19–60 years). In 13 cases (43.3%) the involvement was bilateral, in 12 cases (40%) the left hip was affected, and in 5 cases (16.7%) the right hip was affected. All patients presented with high congenital hip dislocation and clinically evident limb length discrepancy. The mean preoperative limb shortening was 3.2 ± 1.9 cm (range, 0–6 cm), which corresponded to the degree of femoral shortening required during surgery. The mean body mass index (BMI) was 26.1 ± 3.7 kg/m² (range, 20.4–33.3), with most patients classified as overweight. All patients were classified as ASA physical status class I or II and had no significant systemic comorbidities. Radiographic evaluation confirmed complete proximal displacement of the femoral head (≥100% of pelvic height), consistent with the criteria for Crowe type IV dysplasia. Demographic and baseline clinical characteristics are presented in Table 1.
3.2. Surgical and Intraoperative Parameters
All surgical procedures were performed strictly in accordance with the preoperative plan, without intraoperative deviations. Each patient underwent one-stage total hip arthroplasty (THA) combined with transverse subtrochanteric femoral osteotomy using a standard anterolateral (Harding) approach in the lateral decubitus position. The mean operative time was 101.17 ± 19.68 minutes, and the mean estimated intraoperative blood loss was 424.67 ± 151.95 ml. The osteotomy was performed approximately 1 cm below the lesser trochanter, with a mean resection length of 4.23 ± 1.02 cm, depending on the degree of preoperative limb shortening. In all cases, uncemented conical femoral stems were used. The Wagner Cone implant was applied in 27 cases, while custom-designed conical stems developed at KazNIITO were used in 3 cases. Osteotomy fixation was achieved with a derotational plate designed according to typical femoral morphology based on CT analysis. On average, the plate was secured with 6.4 ± 0.7 locking screws, typically three in the proximal and three in the distal fragment, ensuring axial stability and rotational control. In all patients, the acetabular component was implanted in the true anatomical acetabulum. In 9 cases (30%), supplemental acetabular screws were used to enhance cup stability in the presence of minor superolateral bone deficiency. The mean diameter of the implanted cup was 44.5 ± 2.1 mm, with >90% native bone coverage achieved in all cases. Surgical characteristics and intraoperative implant-related parameters are presented in Table 2.
3.3. Radiographic Outcomes
Radiographic assessment of osteotomy healing was performed at 6 weeks, and at 3, 6, and 12 months postoperatively using standard anteroposterior pelvic radiographs. Healing was classified as complete, partial, or absent. At six weeks postoperatively, no signs of union were observed in 12 cases (40%), while 18 cases (60%) demonstrated early callus formation with incomplete bridging across the osteotomy site (weak consolidation), indicating initial stages of bone healing without full cortical continuity. By the three-month follow-up, complete union had been achieved in 15 cases (50%), with the remaining 15 cases (50%) still showing partial healing. At six months, radiographic examination confirmed complete union in all 30 patients (100%), and this outcome persisted throughout the one-year follow-up period. Statistical analysis revealed that the differences in union rates across follow-up stages were significant (p = 0.006; Friedman test), indicating consistent progression of osteotomy healing. No cases of nonunion, fixation failure, or implant-related complications were observed. These findings highlight the reliability and clinical effectiveness of the derotational plate in providing stable fixation and ensuring complete osteotomy consolidation by six months postoperatively.
Analysis demonstrated that changes in union rates were statistically significant (p = 0.006) (method used: Friedman test).
3.4. Functional Outcomes
Functional recovery was assessed using the Harris Hip Score (HHS), Oxford Hip Score (OHS), and Visual Analogue Scale (VAS) for pain at six time points: preoperatively, at discharge, and at 1.5, 3, 6, and 12 months postoperatively. The results for each scale are presented in Figure 4a–c. The mean HHS significantly improved from 66.3 ± 5.6 preoperatively to 90.3 ± 1.3 at 12 months (p < 0.001), with the greatest improvement observed during the first three months (Fig. 4a). A similar trend was noted for the OHS, which increased from 22.8 ± 2.9 to 40.2 ± 1.2 over the same period (p < 0.001), indicating substantial improvement in patient-reported functional outcomes (Fig. 4b). VAS scores decreased markedly from 6.9 ± 1.1 preoperatively to 1.9 ± 0.7 at one year of follow-up (p < 0.001), with the most pronounced reduction in pain observed within the first six weeks (Fig. 4c). These results confirm consistent and statistically significant improvements in functional outcomes, pain reduction, and patient-reported quality of life during the first postoperative year.
3.5. Complications
Throughout the perioperative period and the one-year follow-up, no major complications were recorded. There were no cases of infection, dislocation, implant migration, neurovascular injury, or nonunion of the osteotomy. The only intraoperative complication occurred in one patient (3.3%) — a fissure of the proximal femur during femoral component implantation. The complication was immediately managed with cerclage fixation, after which the postoperative course was uneventful: the osteotomy successfully healed, and no revision surgery was required. All patients completed the 12-month follow-up period.
4. Discussion
Crowe type IV DDH represents a significant surgical challenge due to pronounced anatomical deformities.14,37 The femoral head is completely dislocated, the acetabulum is hypoplastic or malformed, and the proximal femur is narrowed and excessively anteverted.9,38–41 Soft-tissue contractures and considerable leg length discrepancy further complicate anatomical reduction. In many cases, extensive soft tissue releases or staged procedures such as preoperative traction are required.9,10,18 Attempting reduction without femoral shortening may necessitate limb lengthening of more than 4–5 cm, increasing the risk of sciatic nerve injury.15,42 These factors demand meticulous preoperative planning and the use of advanced surgical techniques in Crowe IV cases.
Anatomic placement of the acetabular component in Crowe type IV DDH is a critical step in total hip arthroplasty, as it enables precise restoration of the hip center of rotation.9,37,43 This is particularly important when performing a femoral SSO required for safe reduction of the dislocated hip. However, reconstruction of the true acetabulum remains challenging due to limited bone stock,23,40 which may further necessitate compensatory procedures such as femoral osteotomy.
Various osteotomy techniques have been described in the literature for managing Crowe type IV DDH, including transverse, oblique, step-cut (Z-shaped), and chevron configurations.19,26,31,37,44 Although complex geometries theoretically offer advantages such as increased bone contact area and enhanced rotational stability, biomechanical and clinical studies have not demonstrated clear superiority over the simple transverse osteotomy in terms of union rates, initial mechanical strength, or clinical outcomes.25,45–47 Due to its technical simplicity, reproducibility, and the ability to achieve precise intraoperative correction of femoral anteversion, the transverse SSO remains the preferred method in most cases.48 In our study, this technique was performed in all patients to allow for safe reduction of the femoral head and correction of excessive anteversion. Stable fixation was achieved using cementless conical femoral stems that bypassed the osteotomy site and provided axial and rotational stability. In all cases, fixation was further reinforced with a custom-designed 3D anatomical derotational plate based on patient-specific CT data. This combination allowed for precise rotational correction and rigid stabilization across the osteotomy, promoting early union and implant stability in the context of complex anatomical deformities encountered in Crowe type IV THA.
The functional improvement observed in our cohort further supports the efficacy of anatomical reconstruction combined with stable fixation in Crowe type IV DDH. At one year postoperatively, mean HHS exceeded 90 points, while pain levels, as assessed by the VAS, decreased to an average of 2/7. These outcomes are consistent with those reported by Caylak et al., who demonstrated an increase in HHS from 23 to 94 following transverse subtrochanteric osteotomy and cementless THA in Crowe IV patients.29 Similarly, Sofu et al. reported a five-year postoperative HHS improvement from 39 to 84, underscoring the long-term functional gains achievable in this patient population.28 In addition, the mean OHS in our series improved to 40.2 ± 1.2 at one year, which compares favorably with the findings of Sebastian et al. (2023), who reported an increase in OHS from 13.81 ± 1.79 to 36.25 ± 2.59 at midterm follow-up after THA in DDH patients (including Crowe IV cases).49
According to the data reported by Kawai et al., radiographic union at the osteotomy site was achieved in only 81.5% of patients by 12 months, while 18.5% experienced delayed healing, including one case that required revision surgery with the use of allogeneic strut bone plates.48 In contrast, our series – employing an anatomical derotational plate in conjunction with a cementless conical femoral stem–achieved complete osteotomy union in all patients by the sixth postoperative month, with no cases of fixation failure. These findings highlight the reliability of the proposed fixation construct and its potential to reduce the risk of nonunion in patients with severe hip dysplasia.This is further supported by the radiographic observation that, by one year postoperatively, all implants remained stable with no signs of nonunion. The combined use of an anatomical derotational plate and a cementless conical femoral stem resulted in predictable osteotomy healing and early mechanical stability. Due to its design, the plate provided improved rotational control and additional extramedullary support, effectively addressing the limitations associated with stem-only fixation. In the setting of severe anatomical deformity characteristic of Crowe type IV dysplasia, achieving robust fixation is crucial both for osteotomy healing and for the overall success of THA.37 Although a single intraoperative complication occurred—a proximal femoral fissure during stem insertion in one patient (3.3%)—it was immediately stabilized with cerclage wiring,50 and postoperative recovery was uneventful, with full osteotomy union and no requirement for revision surgery. Importantly, no cases of greater trochanter fracture, gluteus medius detachment, or need for bone grafting, reoperation, or prolonged weight-bearing restrictions were observed. These results reflect both the preservation of abductor integrity achieved through the direct lateral approach and the biomechanical stability afforded by the fixation construct.
Restoring normal gait after THA in Crowe type IV DDH remains a clinical challenge due to long-standing abductor insufficiency and altered biomechanics.51 Although anatomical reconstruction lowers the hip center and improves the abductor lever arm, muscle strength recovery is often delayed.52 In our series, most patients demonstrated significant improvement in gait pattern over the first postoperative year. Early initiation of physiotherapy focused on gluteal strengthening contributed to functional recovery. By one year, the majority achieved a stable, non-lurching gait, though a few patients with severe preoperative muscle atrophy exhibited mild residual abductor lag. Minimal residual leg length discrepancy and bilateral reconstruction in selected cases further contributed to favorable outcomes. These findings highlight the importance of dedicated postoperative rehabilitation in optimizing functional recovery following anatomical hip reconstruction.
Beyond the clinical and radiographic outcomes, the broader implications of this study are noteworthy. The obtained data highlight the importance of developing implants tailored to the anatomical characteristics of the local population and the organizational realities of the national healthcare system. Such approaches are increasingly recognized in international practice and may complement existing solutions by offering potential cost-effective alternatives that could enhance access to surgical care in resource-limited settings without compromising quality. Although a detailed economic analysis was beyond the scope of this study, our findings suggest that localized technology has the potential to be successfully integrated within a healthcare system and serve as an additional option alongside established fixation methods.
4.1. Limitations
This study has several limitations that should be acknowledged. First, the absence of a control group limits the ability to directly compare the outcomes of derotational plate fixation with those of other conventional fixation methods. Second, the relatively small sample size (30 hips) reflects the rarity of Crowe type IV developmental dysplasia of the hip treated at a single institution and may limit the statistical power and generalizability of the findings. Additionally, approximately 40% of initially identified patients were not included in the final analysis due to refusal to participate, medical contraindications, or loss of follow-up, which may further affect the representativeness of the results. Furthermore, all 28 patients underwent the same standardized surgical technique, which ensures internal consistency but limits direct comparison with alternative fixation strategies. Finally, the follow-up period was restricted to 12 months, allowing for the assessment of early functional and radiographic outcomes but not providing information on long-term implant survival, wear, or delayed complications. Future multicenter studies with larger cohorts, comparative groups, and extended follow-up periods are needed to validate these findings, assess reproducibility, and evaluate the long-term effectiveness and durability of this fixation approach.
5. Conclusion
The conducted analysis demonstrated that the use of the domestically developed derotational plate for transverse subtrochanteric femoral shortening osteotomy in patients with Crowe type IV hip dysplasia provided stable fixation, reliable osteotomy union achieved by 6 months, and favorable functional outcomes maintained throughout the 12-month follow-up period. However, longer-term studies are needed to confirm the durability of the implant, assess potential late complications, and evaluate functional recovery beyond the first postoperative year.
Acknowledgements
The authors would like to thank the clinical and technical staff of the National Scientific Center of Traumatology and Orthopedics named after Academician N.D. Batpenov for their assistance and support during patient data collection and surgical procedures.
Corresponding Author
Durdana Oktyabrova, MD, PhD candidate
Astana Medical University, National Scientific Center of Traumatology and Orthopedics named after Academician N.D. Batpenov
Astana, Kazakhstan, 010000
Phone: +7 747 989 4746
E-mail: oktyabrovadana@gmail.com
Authors’ Contributions
Conceptualization – D.O. and K.A.; methodology – B.G. and D.Y.; data analysis – Y.I. and A.B.; investigation – B.S. and T.B.; data curation – D.O., Z.R., and D.Y.; funding – A.B. and T.B.; writing – original draft preparation – D.O., K.A., and D.Y.; formal analysis – T.B. and Z.R.; writing – review and editing – D.O., B.G., and D.Y. All authors have read and agreed to the published version of the manuscript.
Disclosures
The authors declare that they have no conflicts of interest related to the content of this article.
Funding
This work was funded by grant funding for scientific and/or scientific-technical projects for the years 2023-2025 under the topic: AP19678825 “Improvement of surgical treatment of dysplastic coxarthrosis using a new derotational device”.
Availability of Data and Materials
The datasets generated during the current study are available from the corresponding author upon reasonable request and subject to institutional approval.
Ethical Considerations
This study was approved by the local ethics committee of the National Scientific Center of Traumatology and Orthopedics named after Academician N.D. Batpenov, Ministry of Health of the Republic of Kazakhstan (approval No. 4, dated November 9, 2022), in accordance with the principles of the Declaration of Helsinki. Written informed consent to participate was obtained from the patient prior to inclusion in the study. All patient data were anonymized and handled confidentially throughout the research process.
Consent for Publication
Written informed consent for publication of patient data and accompanying images was obtained from all participants. A copy of the signed consent form can be provided to the Editor-in-Chief upon request.



_progression.png)
_progression.png)
_for_pain_progression.png)


_progression.png)
_progression.png)
_for_pain_progression.png)