Introduction
Persistent pain following spine surgery is a well-recognized clinical challenge. Many patients continue to experience chronic neuropathic pain despite appropriate surgical intervention and conservative management, often resulting in long-term disability and reduced quality of life.1 Conventional treatment options including medications and consideration of repeat surgery frequently offer limited benefit, and prolonged opioid use carries its own risks.
Spinal cord stimulation (SCS) has become an important option for patients with refractory pain despite corrective spine surgery.2–4 By placing electrodes in the epidural space to modulate dorsal column and dorsal horn signaling, SCS can lessen neuropathic pain and improve overall function. Multiple studies have shown that SCS provides meaningful and durable pain relief and may reduce reliance on opioid therapy in patients with prior lumbar surgery.3–8
Here, we present the case of a patient with severe pain and functional impairment after lumbar surgery who experienced substantial improvement in both pain and mobility following treatment with the Prospera SCS system with multiphase stimulation [BIOTRONIK Inc, Oregon USA].
Case Presentation
A 39-year-old female with a history of lumbar degenerative disc disease and multilevel disc bulges contributing to spinal stenosis presented with chronic low back pain and left-sided lumbar radiculopathy. Her symptoms began several years earlier and persisted despite a lumbar decompression surgery in 2023. Following surgery, the patient continued to experience severe neuropathic pain radiating down the left leg. She had failed multiple medication regimens, including neuropathic agents and opioid analgesics, as well as multiple epidural steroid injections, none of which provided lasting benefit. She was evaluated again by spine surgery, where repeat surgical intervention was not recommended.
At the time of her initial pain management evaluation, the patient was wheelchair bound due to pain and exhibited significant weakness in the left lower extremity, severely limiting her mobility and daily functioning. Given her refractory symptoms and substantial functional decline, she was counseled and consented for a SCS trial using the Prospera SCS system with multiphase stimulation.
During the SCS trial, the patient experienced greater than 65% improvement in pain intensity. Notably, she was able to get out of her wheelchair and ambulate with a cane, marking a significant improvement in functional status. Due to her strong response, she proceeded with permanent SCS implantation.
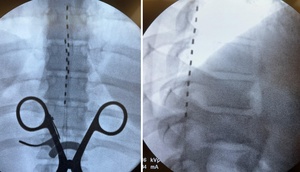
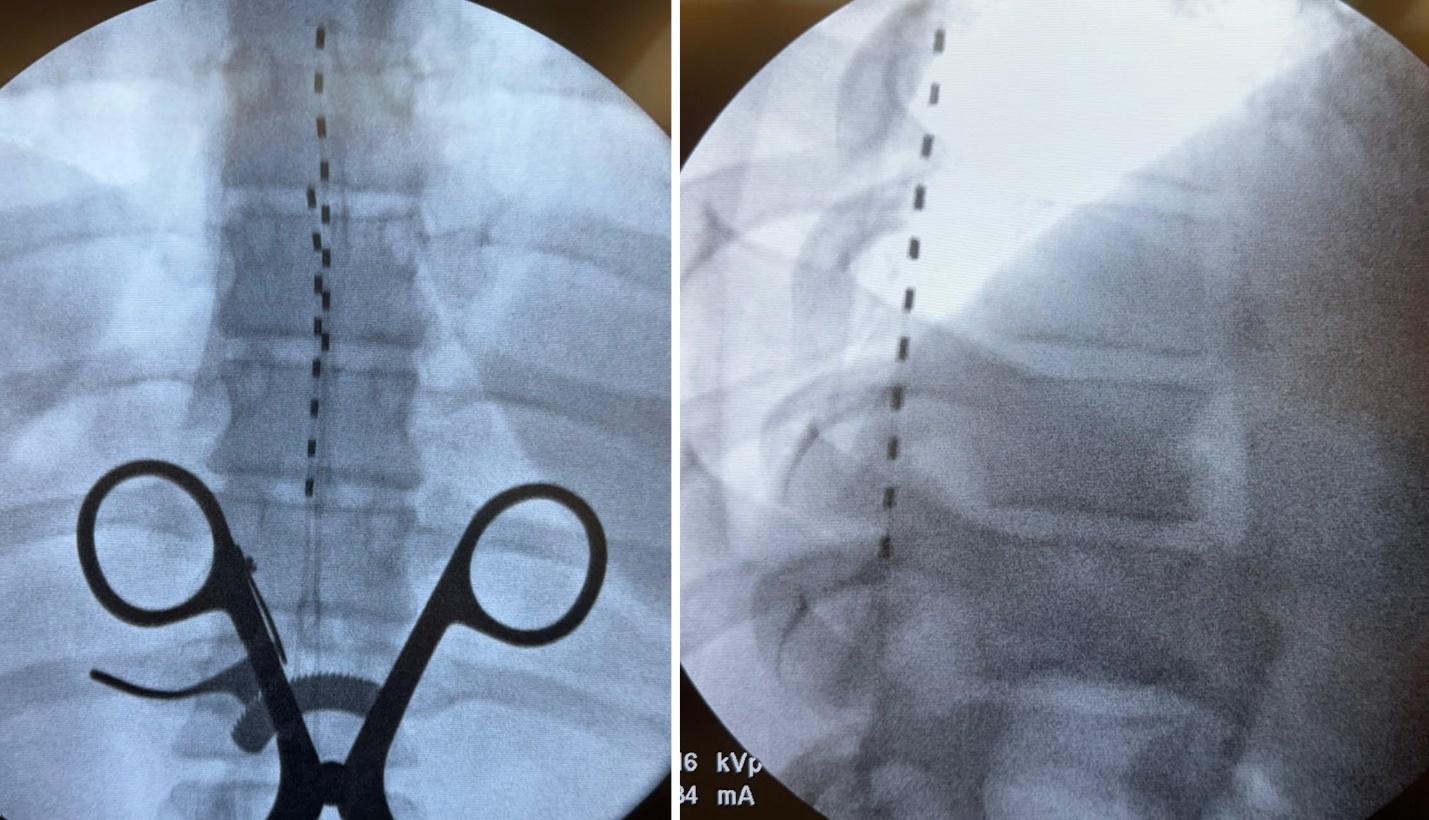
At follow-up after implantation, the patient continued to report >70% improvement in pain, further reduction in radicular symptoms, and enhanced functional mobility. She remained able to ambulate with a cane and had begun to walk independently for short distances. Her quality of life, mood, and overall activity level improved substantially. Images of the implant are shown below with one lead placed at the top of T7 with the second lead placed at the top of T8 slightly left of midline given her pain complaints (Figure 1).
Discussion
This case highlights the potential for substantial functional improvement in a patient with chronic lumbar radiculopathy who had exhausted both conservative therapy and surgical options. Although SCS is traditionally viewed as a treatment aimed at reducing neuropathic pain, this case illustrates that its benefits may extend well beyond analgesia. The patient experienced not only marked pain reduction but also meaningful gains in mobility, strength, and independence, transitioning from wheelchair dependence to ambulating with a cane and eventually walking short distances independently. This underscores the broader therapeutic value of SCS in restoring function and improving overall quality of life.
SCS is well established in the management of persistent pain after spine surgery, often termed failed back surgery syndrome. However, its indications have expanded in recent years to include a wider range of neuropathic and mixed pain conditions, such as complex regional pain syndrome, painful peripheral neuropathies, radiculopathy without prior surgery, and selected cases of axial low back pain.9–12 Despite this broadening scope, most published clinical studies continue to emphasize pain reduction as the primary outcome measure. Functional improvement, while clinically and personally meaningful to patients, is less frequently highlighted in the literature.
Although spinal cord stimulation offers meaningful pain relief and functional improvement for many patients, it is not without risks. Physicians should remain aware of potential device-related complications as well as biologic complications such as lead migration, dural puncture, infection, and the need for revision surgery as some examples.13–17 Given these considerations, it is essential to provide thorough informed counseling so patients understand both the potential benefits and the limitations and risks prior to proceeding with SCS therapy. Proper patient selection and education remain critical to optimizing outcomes and minimizing adverse events.
This case is of particular interest because it demonstrates the clinical utility of the Prospera SCS system with multiphase stimulation. This platform uses proprietary stimulation patterns designed to deliver therapeutic benefit at lower electrical doses, potentially improving comfort and reducing habituation.18 Although real-world data on this system remain limited, the patient in this report achieved greater than 70% pain relief along with a striking improvement in daily functioning. These observations suggest that newer SCS technologies, including multiphase stimulation, may offer advantages for certain patients, especially those with complex postoperative neuropathic pain.
Conclusion
This case demonstrates that spinal cord stimulation can provide not only substantial pain relief but also meaningful improvements in mobility and overall function for patients with chronic radiculopathy who have failed conservative and surgical treatments. The patient’s transition from wheelchair dependence to independent ambulation highlights the broader therapeutic potential of neuromodulation beyond pain control alone. While SCS is not without risks and requires careful patient counseling and selection, newer technologies—such as the Prospera system with multiphase stimulation—may offer enhanced outcomes in appropriately selected individuals. This case adds to the growing body of evidence supporting SCS as a valuable option for restoring quality of life in patients with refractory neuropathic pain.