INTRODUCTION
Scaphoid proximal pole nonunion treatment is a challenging topic for hand surgeons. The natural evolution will lead to osteoarthritis (OA) and scaphoid nonunion advanced collapse (SNAC).1 Similarly, scapholunate instability leads to carpal malalignment and subsequently to osteoarthritic changes of the radio-carpal joint (scapholunate advanced collapse SLAC).2 When it is not anymore possible to reconstruct the necrotic pole or to correct the carpal malalignment, salvage surgical procedures are indicated; procedures such as proximal row corpectomy (PRC), four corner fusion (4CF), or total wrist fusion (TWF) significantly decrease pain but also reduce the ROM.3
The adaptative proximal scaphoid implant (APSI) is a hydrocarbon ovoid-shaped interpositional implant that allows adaptive mobility during motion.4
The Pyrocarbon has good compatibility with joint cartilage and bone, a modulus of elasticity similar to bone minimizing stress shielding effects and resorption.5,6 The implant is designed with two radii of curvature: in the frontal plane, the smaller radius of curvature corresponds to the scaphoid fossa, and the larger radius of curvature is directed anteroposteriorly to the transverse plane. These two axes of the implant make it adaptable to the kinematics of the wrist.7 The APSI implant is an attractive solution because it is minimally invasive and does not “burn bridges” for salvage procedures such as PRC or 4CF. The implant can avoid a proximal row collapse, maintain carpal kinematics, and it is believed to prevent the progression of osteoarthritis.4
A systematic review was conducted to analyze the clinical and radiological outcomes of APSI implants and possible complications for evaluating if it is a safe and reliable alternative for treating SNAC and SLAC wrist.
METHODS
Search strategy and literature search
A systematic review of the literature was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.8 The two investigators (FS, GM) independently performed the literature search. The literature search was conducted in the following databases: Medline (PubMed), Web of Science, and Scopus were accessed on the 30th of October 2020. The following keywords were used in combination: APSI, scaphoid proximal pole, implant, scaphoid avascular necrosis, SLAC, SNAC, pyrocarbon, prosthesis, and spacer with no limitations for the year of publication. Two authors independently assessed the abstract of each publication. Article full-text was accessed for all the relevant abstracts. If the full text was not available, this warranted the exclusion from the study. The bibliography of each full-text article was also retrieved to identify additional studies.
Eligibility criteria
All the studies reported data of patients undergoing the APSI procedure for SNAC and SLAC wrist. According to the authors’ language capabilities, English, Spanish, Italian, and French articles were considered. Either prospective or retrospective clinical studies were considered. Only studies published in a peer-reviewed fashion were eligible.
Methodological quality assessment
The two investigators (FS, GM) independently evaluated each study according to the Coleman Methodological Score (CMS).9–11 The CMS score is highly reliable, and it is widely used to assess the methodological quality of systematic reviews and meta-analyses. With this score, we analyze several characteristics of the included papers: study size, follow-up duration, surgical approach, type of study, description of surgical technique, rehabilitation, and complications. Further outcome criteria assessment, the procedure of assessing outcomes, and the subject selection process were also evaluated. CMS scores ranks from 0 (poor quality) to 100 (excellent quality), with values > 60 considered satisfactory.
Outcomes of interest
Data extraction was performed by two independent authors (FS, GM). The following demographic data were extracted: number of patients, sex, gender, mean age, follow-up duration. The following outcomes of interest were extracted: Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire, a 10-cm Visual Analogical Scale (VAS), the Mayo Wrist Score (MWS), the Patient-Rated Wrist Evaluation (PRWEB), grip strength and Range of Motion (ROM) (flexion-extension arch), return to work, carpal misalignment, osteoarthritis progression, and complications.
RESULTS
Search results
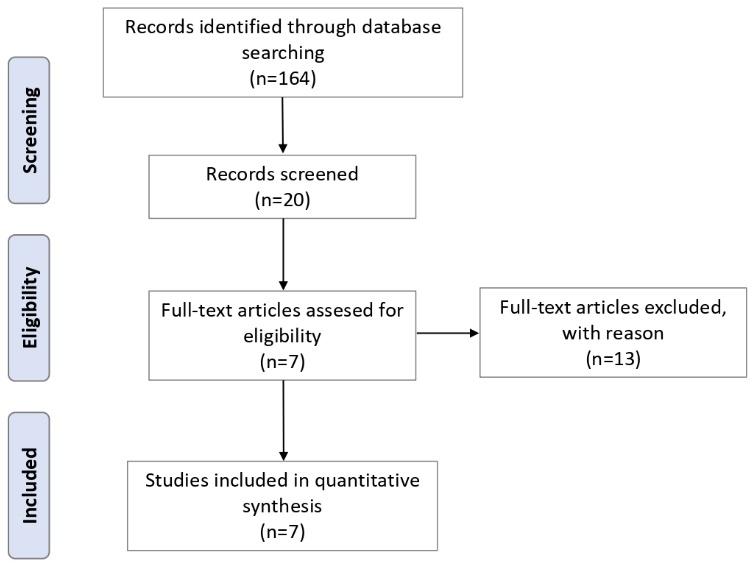
The literature search resulted in 164 articles. Of these, 144 were excluded based on the title because not inherent to our review. A further 13 articles were excluded after the reading of the abstract. Finally, seven studies were considered for the present study (Figure 1).
Methodological quality assessment
The CMS evidenced some limitations and points of strength of the present study. Study size and follow-up duration were poor. The surgical approach, surgical technique, and rehabilitation were well described. Complications were thoroughly discussed in most articles. Outcome measures and related timing of assessment were often defined, reporting moderate reliability. The procedure assessing outcomes and the subject selection processes were often biased and not satisfactorily described. The mean CMS was 60 (52 to 71), indicating a satisfying quality. The CMS is shown in Table 1.
Patient demographic
Data from 156 procedures were retrieved. 88% (126/156) were male. The average age of the patients was 43.7 years (24 to 71). The mean follow-up was 78 months (11 to 276). Demographic data are shown in Table 2.
Surgical technique
All procedures were performed using a dorsal approach4,12–14 except two studies: One used a volar approach in 4/41 cases and lateral in 2/41 cases,15 the second performed arthroscopic scaphoidectomy.7
Associated stiloidectomy was performed in four studies4,12,13,15 for a total of 87/118 (73%) patients; two studies did not perform stiloidectomy,7,16 and one13 performed the stiloidectomy, but the percentage was not reported. A dorsal capsulodesis was performed in two studies: eight of 39 patients (20%)13 and in all patients 36/36.12
Rehabilitation
All studies had their rehabilitation program with a variable lapse of immobilization time before starting mobilization. Five studies recommended three weeks wearing full time a spica splint before beginning rehabilitation of the wrist.4,12,14–16 Aribert suggested a shorter immobilization of 2 weeks, while Gras et al. suggested an immediate ROM at home.
Outcomes of interest
Subjective and objective outcomes
All subjective and objective outcomes are reported in Table 3. Four studies7,13,14,16 described postoperative pain using the VAS (Table 3). Daruwalla reported a median preoperative VAS of 81, improving to 19 at eighteen months. The other three studies reported only the postoperative value with an average of 13.6 (range 7-22.3).
The Disability of Arm, Shoulder, and Hand score (DASH) or QDASH was evaluated in five studies.7,12–14,16 The median postoperative DASH was 19.6 (range 7.6-26). The Mayo wrist score was evaluated in four studies7,12,13,16 with a median value of 74 (range 67,5-80).
All the studies measured the flexion-extension arch with an average value of 114° (range 71°-136°). The grip strength was evaluated in six studies.4,7,12–15
Return to work
Daruwalla et al. reported a return to work at an average of eleven weeks; Aribert et al. reported that 23/24 returned to their previous job at an average time of 2.1 months. Santos et al. reported that all patients returned to their previous job. Pequignot et al. reported that 22/25 (88%) patients returned to their previous job. Three studies did not report any information regarding return to work: Grandis et al., Poumellec et al., and Gras et al. (Table 3)
Carpal misalignments
One study13 reported the presence of DISI in 46.3% of patients. One study4 did not report any changes in the SL angle. One study12 reported changes in the SL angle in 9/19 patients (47%). Gras et al. reported a correction of the dorsal intercalated segmental instability (DISI) in 5/8 patients (62.5%) after surgery. (Table 4)
Progression of Osteoarthritis
One study13 reported a progression of osteoarthritis in 6/33 patients (18%). Poumellec et al. report a progression of the OA in 6/19 of patients (32%). Gras et al. reported a radial stiloidectomy 2-3 years after the APSI procedure in 3/14 patients (21%) for radio-scaphoid arthritis progression. Santos et al. reported OA progression in all the cases (12/12). Three studies4,14,15 did not report any OA progression. The percentage of patients who reported progression of OA was 17.3% (27/156; Table 4).
Complications
Four studies reported no complication,4,14–16 Gras et al. reported two mobilizations of the implant treated with a 4CF. Poumellec et al. reported two cases of early implant dislocations due to a lack of compliance to the postoperative immobilization required.
Aribert et al. described 6/33 complications (18%). One case of early sepsis required implant removal, four instances of dislocation, and one patient complained about persistent pain caused by radio-scaphoid impingement and was treated with a 4CF. The total amount of mobilization of the implant was 5.1% (8/156; Table 4).
DISCUSSION
Some of the most widely used treatment options for wrist pain include PRC and 4CF. A systematic review in 20093 compared these two techniques and found no differences in terms of pain, grip strength, and subjective outcome. These data suggest that PRC has fewer potential complications and better ROM than 4CF but a higher risk of progression of OA. Some researchers have tried to replace the scaphoid with interposition of autologous material,17,18 silicon,19 or metal,20 but the results were not satisfactory.
The average quality of the studies included in the present investigation is moderate, with an average CMS of 60 points; only one study13 had good CMS values. The most common surgical approach was from the dorsal wrist except for two studies that adopted an arthroscopic approach.7,15 Arthroscopy is an attractive option for its minimally invasive procedure and consequent preservation of soft tissues, including ligaments and capsules.
Stiloidectomy is widely performed4,12–15 (73% of all patients) and is advisable in the case of a stylo-carpal impingement. Two papers12,13 performed a dorsal capsulodesis with no improvement in implant stability. There were six dislocations of the implant out of eight in these studies. All studies reported a postoperative immobilization of 2-3 weeks except for one,7 which allowed an early ROM probably due to the low invasiveness of the arthroscopic procedure.
All the studies described a reduction in grip strength and the flexion-extension arch compared to the contralateral wrist but with improvement versus preoperative values. The highest value in flexion-extension arch (136° vs. an average value of 92°) and grip strength (44.1 kg vs. an average value of 34 kg) were reported by Gras et al., who performed the replacement arthroscopically and with an early rehabilitation protocol. The same study7 reported the best score in subjective outcomes such as DASH and VAS. We hypothesize that this is due to less scar tissue and a more aggressive rehabilitation protocol.
Gras et al. reported a correction of the dorsal intercalated segmental instability (DISI) in 5/8 patients (62.5%) after surgery. The role of the APSI is controversial in its impact on the DISI deformity: two studies12,13 reported an increased SL angle in 46% of patients despite the use of capsulodesis. We speculated that the arthroscopic approach preserves the secondary stabilizer versus the open technique.
The percentage of patients who reported progression of OA with APSI was 17.3%, the average increases to 26% (27/103) if we consider only studies with more than five years in the follow-up: Aribert et al., Poumellec et al. Pequignot et al., Gras et al. Santos et al. The APSI slowed the progression of OA but did not stop it. The implant mobilization has a rate of 5.1% (8/156). The surgical approach and postoperative immobilization does not correlate with this value. In one series,7 the use of the implant for a nonunion of the body of the scaphoid leads to mobilization.
All procedures were performed using a dorsal approach4,12–14,16 except two studies: One used a volar approach in 4/41 cases and lateral in 2/41 cases,15 the second performed arthroscopic scaphoidectomy.7 Associated stiloidectomy was performed in four studies4,12,13,15 for a total of 87/118 (73%) patients; two studies did not perform stiloidectomy,7,16 and one14 performed the stiloidectomy, but the percentage was not reported. A dorsal capsulodesis was performed in two studies—eight of 39 patients (20%)13 and all patients 36/36.12
All studies had their rehabilitation program with a variable lapse of immobilization time before starting mobilization. Five studies recommended three weeks wearing full time a spica splint before beginning rehabilitation of the wrist.4,12,14–16 Aribert suggested a shorter immobilization of 2 weeks, while Gras et al. suggested an immediate ROM at home.
The study has several limitations. For example, we grouped different cohorts of patients in terms of demographics, surgical indication, surgical technique, outcome measurements, and follow-up.
The main endpoint of this systematic review is that the APSI implant is a reliable alternative for treating SNAC wrist and SLAC wrist. Its indications are limited: The cartilage of the scaphoid fossa and the capitolunate joint must be intact. However, the implants require less surgical dissection compared to 4CF and PRC. This procedure is more expensive than 4CF and PRC due to the high cost of the spacer, but further surgeries are possible in case of failure.