Introduction
Abductor pathology presents a wide range of injuries from tendinitis to complete ruptures of the gluteus medius and minimus.1 Degenerative or traumatic tears of the hip abductor tendons, called rotator cuff tears of the hip, occur in patients with intractable lateral hip pain, weakness, and/or limping.2 Direct repair may be performed by arthroscopy3,4 or open surgery via bone anchors or trans-osseous tunnels.5 In general, arthroscopic treatments have shown similar results to open surgery when the direct repair of abductor mechanism rupture is feasible.6 Not all tears are reparable, and in cases of complete tendon rupture with muscle atrophy, the results of primary repair have not been very encouraging.1 Tendon tears with large retraction usually need reinforcement to avoid failure after a direct repair. Several techniques have been described, including augmentation with Achilles allografts,6 advancement of the vastus lateralis,7,8 and transfer of the gluteus maximus.9–11 Whiteside et al.9,11 described a surgical technique to transfer the anterior portion of the gluteus maximus to the greater trochanter to treat chronic, irreparable deficiency of the abductor muscles of the hip.
The aim of this study is to report the outcomes of a new technique addressing irreparable tears. This method combines the attachment of a “V” flap of the upper half of the gluteus maximus to the greater trochanter9 reinforced with a synthetic polyethylene terephthalate mesh (MUTARS system; Implantcast GmbH, Buxtehude, Germany).
Case Report
We conducted a monocentre retrospective study with ethical approval from our institution. We included 3 patients from September 2017 to October 2018 with intractable lateral hip pain and severe abductor deficiency without arthritis of the native hip joint. Patients with a minimum 1 year of follow-up after surgical treatment were included in this study.
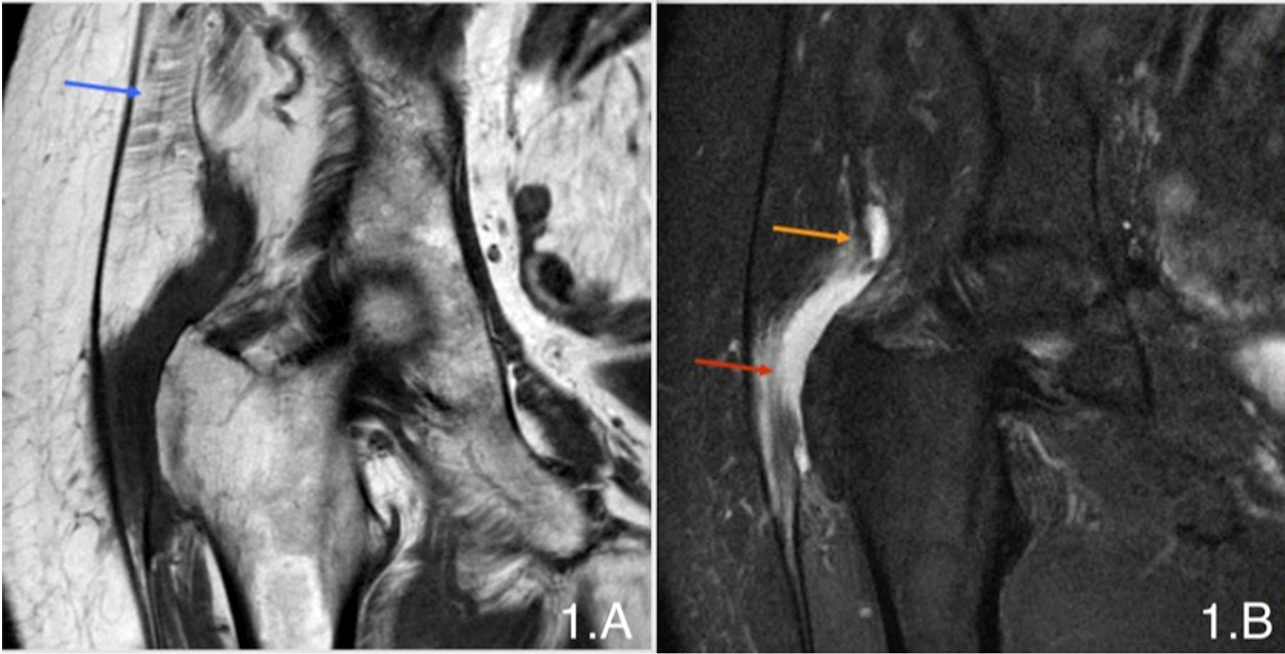
All of the patients presented with refractory pain to non-operative treatment, including corticosteroid trochanteric bursal injections (range 2 to 4) and physical therapy for the abductor mechanism. This conservative treatment was carried out on average 20 months (range 15-24) before surgery due to the persistence of pain and severe limp. On evaluation, our three patients had severe limp, positive Trendelenburg sign, and pain over their greater trochanter and gluteus medius and minimus muscles. There was weakness (M1/M5) and trochanteric pain with hip abduction in the lateral decubitus. There was no hip pain with passive range of motion, the passive range of the hip motion was full and non-painful, and there was no pain in the low back during the physical examination. AP and axial radiographs were normal in two of the three patients, with no calcifications adjacent to the greater trochanter or degenerative hip changes. One of the patients showed slight osteoarthritis of her hip with no clinical relevance. All of the patients underwent magnetic resonance imaging (MRI) preoperatively. The T1-weighted axial view was used to determine atrophy of the gluteus medius and minimus muscles. The main indication to reinforce the gluteus medius repair was a fatty degeneration of the muscle fibres and a significant retraction of the tendon. MRI revealed a full thickness rupture of the gluteus medius with significant muscular fat atrophy in addition to trochanteric bursitis in the first patient. In the second subject, gluteus medius tendinopathy and muscular atrophy with partial rupture in its posterosuperior facet and full thickness rupture of the rest of the insertions to the great trochanter was observed. The last patient’s MRI showed a full-thickness rupture of the gluteus minimus tendon with atrophy and fatty infiltration in the muscle and a partial rupture of the gluteus medius tendon with atrophy of the muscle (Figures 1A-1B and Figures 2A-2B).
The same surgical protocol was followed in all of the cases. The patients were positioned in lateral decubitus. A longitudinal incision of 15 cm was made centred in the greater trochanter. The gluteus maximus muscle and fascia lata were split in line with its fibres. After bursectomy, the rupture of gluteus medius was identified as the fatty infiltration and retraction of the tendon (Figure 3).
The gluteus medius muscle and tendons were debrided and individualised, mobilising the scarred-in tendons from the surrounding tissue to allow for the placement back in its footprint of the greater trochanter. Then the greater trochanter was decorticated with a rectangle-shaped chisel (Figures 4A and 4B) and a cancellous bed was created to adjust the gluteus medius direct repair and the gluteus maximus transfer according to the Whiteside technique11 (Figure 5).
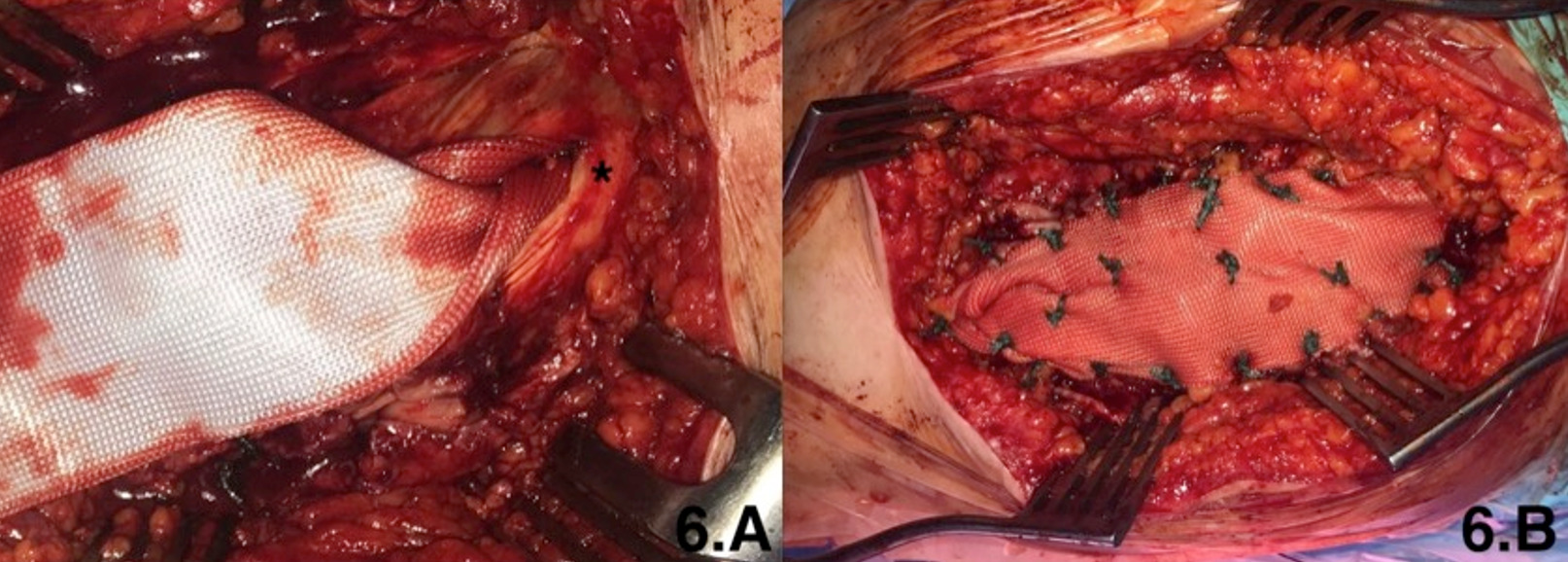
In the first step, the anterior part of the gluteus medius was reinserted at the anterior facet using 3 trans-osseous simple sutures with heavy non-absorbable sutures (Number 5 Ethibond, Ethicon Inc., Somerville, NJ, USA). This direct repair was made while the hip was positioned in 20º of abduction. Afterward, the anterior third of the gluteus maximus was mobilised and transferred to the lateral and posterior facets with a “V”-shaped designed flap. This flap was anchored by trans-osseous drill holes using a heavy non-absorbable suture to cover the entire great trochanter. The contiguous gluteus medius and gluteus maximus edges were sutured together with non-absorbable sutures. We covered and reinforced the flap with a synthetic polyethylene terephthalate mesh with multiple No. 5 Ethibond sutures (Figures 6A and 6B). This mesh was finally buried in the vastus lateralis and sutured under it. In all of the cases, a hip abduction orthosis was placed in 20º of abdution and was used to avoid active abduction and more of 90º of flexion for one month postoperatively. Partial weight bearing with 2 crutches was allowed for 2 months and a cane was recommended for an additional 2 months. Active abduction exercises were avoided for 6 weeks postoperatively. After this period, gradual abduction strengthening exercises were allowed.
Clinical status was measured using the Visual Analogue Scale (VAS)12, modified Harris Hip Score (HHS)13, and abductor strength using the Medical Research Council muscle strength grading system (grades 0 to 5, with grade 0=no muscle contraction to grade 5=normal power) (Table 1). The patients were examined in the lateral decubitus position confirming weakness in the abductor mechanism.
Results
All three patients were female, with an average age of 79.6 years (range 76-87) and an average BMI of 24.6 (range 23-27) (Table 2).
In all of the cases, a complete rupture of the gluteus medius tendon was observed during surgery with significant retraction. The average follow-up was 18 months (range 12-24 months). Pain and functional status improved in all of the cases. The average VAS score improved from 8.3 (range 7-10) preoperatively to 1.6 (range 1-2) postoperatively. Marked improvement was noted in the Modified Harris Hip Score, increasing from an average of 31.8 (range 9.2-59) to an average of 75.6 (range 71.8-82) (Table 3). The patients were also examined in the lateral decubitus position, evaluating the hip abductor mechanism against gravity. According to the Medical Research Council muscle strength grading system, the patients showed muscle strength gain, all increasing from 1 to 3 (Table 3). Trendelenburg sign, that was preoperatively present in the three patients, dissapeared after the surgery in all of the cases (Table 3). There were no postoperative surgical sites or other complications.
Discussion
Rupture of the hip abductor mechanism in the non-prosthetic hip can occur spontaneously because of a degenerative process or as an acute traumatic rupture without prior peritrochanteric chronic pain.14,15 The patients included in this small series had spontaneous degenerative tears in their hips without previous surgery. In many cases, the diagnosis is delayed, since many patients initially present with gluteal tendonitis or trochanteric bursitis.16,17 A rupture of the hip abductors should be suspected due to the lack of improvement in pain through adequate conservative treatment or local injections and severe functional impotence on physical examination, often accompanied by the Trendelenburg gait and disability or loss of strength to perform active abduction in the lateral decubitus position. The Trendelenburg sign has been shown to be the most sensitive and specific for diagnosing tendon ruptures of the gluteus medius, with acceptable interobserver reproducibility.18 This pathology has been classically considered to be uncommon, although modern literature shows a high prevalence, up to 45.8%, in patients with a clinical duration of peritrochanteric pain longer than 12 months.18 At the time of diagnosis, imaging tests such as ultrasound or MRI are useful to confirm clinical suspicions.19
Systematic reviews of open and endoscopic repair techniques have shown similar improvements in pain and function for ruptures of the gluteus medius with the absence of substantial retraction.20 However, for large retracted tears or those with high fatty degeneration, an open technique offers a comprehensive approach and allows the use of different augmentation methods. In cases where the tendon has fatty degeneration or a large retraction that prevents direct repair, augmentation techniques are recommended. Betz et al.7 described the advancement of the abductor apparatus using the lateral vast of quadriceps in a study of 9 patients and managed to treat defects of the abductor apparatus of up to 10 cm with a 69% satisfaction rate, although they reported a significant loss of strength in the quadriceps. Augmentation can also be achieved by transferring the gluteus maximus and tensor fascia lata. In a study of 11 patients using this technique, Whiteside et al.9,11 reported that nine patients regained strong abduction against gravity with a mean follow-up of 33 months (range 16-42 months); one patient had weak abduction with a moderate limp and another with multiple health issues had weak abduction with a severe limp even after 6 months. Chandasekraran et al.10 used the same gluteus maximus and tensor fascia lata (TFL) transfer for chronic abductor tears that could not be repaired in 3 patients, all with preoperative Trendelenburg gaits. At the latest postoperative review, 2 patients had a normal gaits and the other continued to have a Trendelenburg gait. Using a different augmentation technique, Davies et al. described an open repair with trans-osseous tunnels and allograft of human dermal fascial supplement (GRAFTJACKET, Wright Medical Technology, Memphis, TN, USA) for complete ruptures of the gluteus medius. They reported good outcomes with an overall mean improvement of 34 points on the HHS while the strength on manual muscle testing improved from a mean of 3.1 to a mean of 4.7 at one year. Bucher et al. reattached the gluteus medius tendon using synthetic augmentation (using the Ligament Augmentation and Reconstruction System) through a trans-osseous tunnel, obtaining significant improvement (p<0.05) in all clinical scores studied in a series of 22 patients.
Our novel augmentation technique for retracted degenerative gluteus medius ruptures via direct suture of the remnant gluteus medius reinforced with a “V” flap of the gluteus maximus and Trevira mesh, providing mechanical support to the suture, is an alternative technique to prior methods, with significant improvement in pain and function in all three patients, as demonstrated by the VAS and Harris Hip Scale and gain of three points in strength according to the Medical Research Council muscle strength grading system. Furthermore, our technique was able to correct the Trendelenburg sign and improved the limp in our 3 patients after a 1-year follow-up.
Conclusion
Although our study’s limitations include the small sample size attributable to the fact that this injury is relatively uncommon, this technique using a combination of a gluteus maximus flap and synthetic mesh to repair retracted and fatty degenerated gluteus medius ruptures suggests efficacy in terms of improving clinical symptoms and functional status as verified by the scores. Therefore, we believe that our novel technique is a reproducible way to augment irreparable tears of the abductor mechanism of the hip.
Authors contribution:
Iñigo Jimenez-Telleria and Xabier Foruria:
- Conception, design acquisition, analysis and interpretation of data for the work; AND
- Drafting the work
- Final approval of the version to be published;
- Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Jesús Moreta and José Luis Martinez-de los Mozos:
- Analysis and interpretation of data for the work;
- Revising it critically for important intellectual content
- Final approval of the version to be published;
- Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Lucia Bernuy and Oscar Casado:
- Acquisition and interpretation of data for the work;
- Revising it critically for important intellectual content
- Final approval of the version to be published;
- Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Declaration of conflicting interests
The authors declare that they have no conflicting interests. They have not received grant support or research funding and have not any proprietary interests in the materials described in the article.

_and_fat_saturated_t2_weighted_(figure_2b)_images_.png)
_and_the_fatty_infi.png)
_and_after_being_decorticated_(b)_.png)
.png)

_and_fat_saturated_t2_weighted_(figure_2b)_images_.png)
_and_the_fatty_infi.png)
_and_after_being_decorticated_(b)_.png)
.png)