Introduction
Fractures of the radial head and neck are the most common involving the proximal forearm and account for 75% of fractures in this area.1 Radial neck fractures are less common, with a reported incidence of circa 16.7 per 100 000 persons and no difference in gender occurrence.1 Radial neck fractures usually result from a combined valgus and axial load to the elbow, often caused by a fall on the outstretched hand.1
Isolated nondisplaced radial neck fractures can be treated conservatively with a short mobilization period, followed by protected early mobilization.2 Nonunion or delayed unions are rarely reported in adults and are probably asymptomatic. There are case reports where patients have few symptoms and are treated conservatively with favorable functional outcomes.3 Operative treatment choices have also been reported. They are reserved for symptomatic patients with physically demanding occupations and include radial head excision,4 autologous bone grafting with or without additional fixation,5,6 and replacement with a bipolar radial head prosthesis.7
There is no established gold standard surgical technique for treating symptomatic nonunion or delayed union of the radial neck. The purpose of our study is to present a new method of treatment of a radial neck fracture nonunion by using cylindrical bone autograft harvested from the iliac crest and fixed with headless compression screws.
Case report
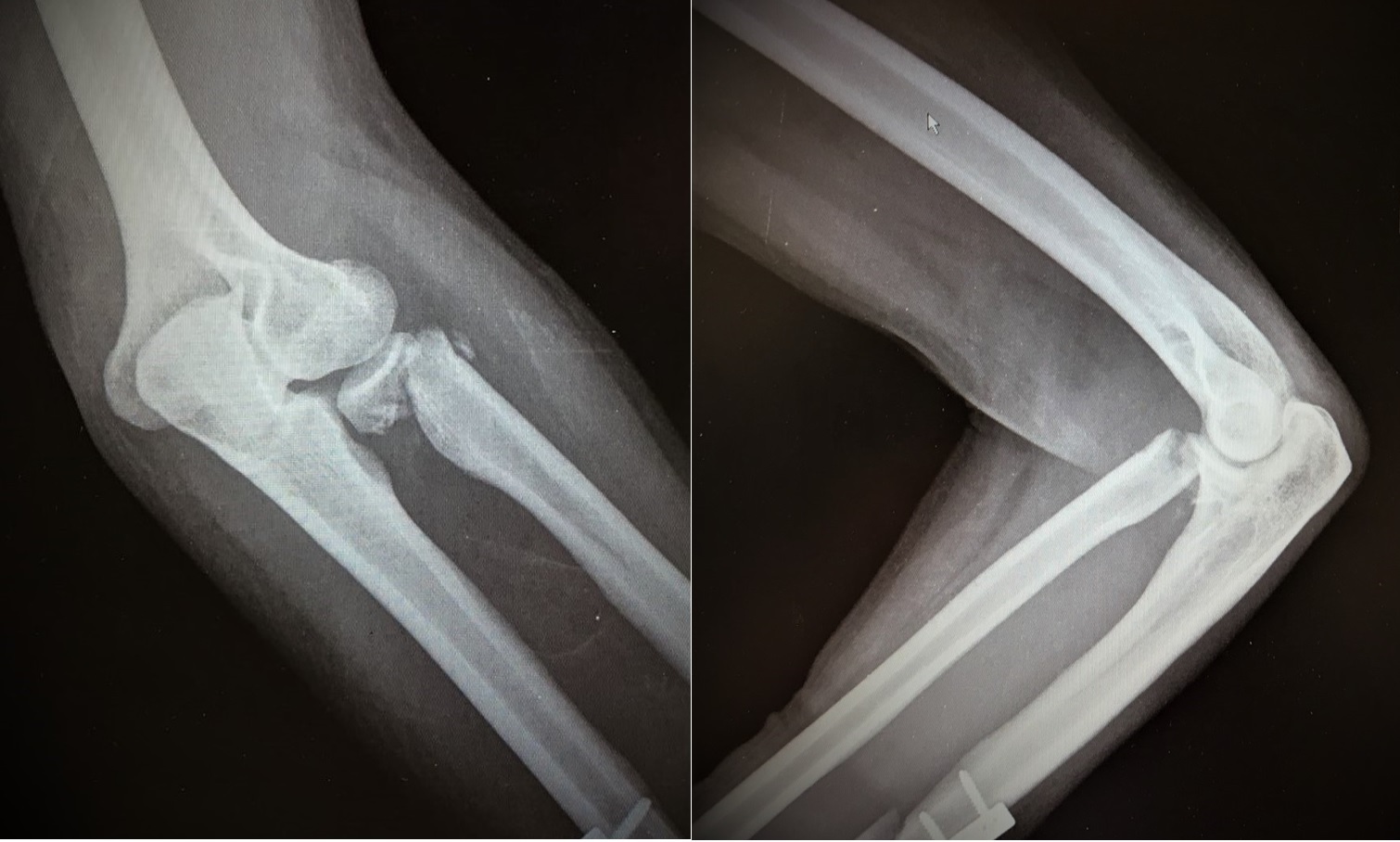
We present a case of radial head nonunion in a 34-year-old male polytrauma patient due to a car accident. The patient provided his written informed consent to publish material that may relate to him. The patient was treated for his concomitant injuries and stayed in the intensive care unit for one month. The fracture of the left radial neck was missed during the initial approach of the patient. It was found two weeks later at his radiographic examination during his hospitalization in the intensive care unit. The fracture was initially treated conservatively with a sling. However, it failed to unite six months after the accident (Figure 1). The patient had persistent pain around the elbow, a normal range of motion, and no radiographic evidence of union.
We decided to treat the patient operatively.
Surgical technique
The procedure was performed under general anesthesia and regional nerve block with the patient in supine position with the shoulder abducted and the arm placed on a radiolucent table. Prophylactic intravenous antibiotics were administered, and a sterile tourniquet was applied to avoid bleeding. The ipsilateral or contralateral iliac crest area was also prepped and draped for iliac bone graft harvesting.
For this technique, we used the posterolateral (Kocher) approach between the anconeus and extensor carpi ulnaris. We marked our landmarks before making an incision: the lateral epicondyle and the radial head (which is felt with pronation/supination of the forearm) with the elbow flexed. An approximately 5cm slightly dorsally curved incision originating from the lateral epicondyle and extending distally over the radial head was made. Then, the interval between the two muscles was identified by finding the small penetrating veins. The deep fascia was incised, the anconeus was reflected posteriorly, and the extensor carpi ulnaris anteriorly. The arm was held in pronation to move the posterior interosseous nerve away from the field. The capsule was then obliquely incised anterior to the lateral ulnar collateral ligament, and the radial head was exposed. The fracture line was found, and the condition of the radial head was evaluated. All the fibrotic tissue was removed, and meticulous debridement of the radial head undersurface was performed until the healthy cancellous bone was found. After that, the radial neck was exposed, and its medullary canal was prepared using a hand reamer from a radial head arthroplasty instrumentation. In the present case, reaming went through until 7mm in diameter and 25mm in depth (Figure 2A).
The skin over the iliac crest was stretched by placing a fist above the iliac crest and pushing the abdominal wall medially. A longitudinal incision of about 3cm long was performed 2-4cm posterior to the anterior iliac spine. Dissection was performed until the periosteum of the iliac crest was reached. The Osteochondral Autograft Transplantation System (COR Precision Targeting System, Depuy Mitek, 325 Paramount Drive, Raynham, USA) was used to harvest a bone cylinder from the iliac crest of 8mm in diameter and 25mm in length. The wound was closed in layers.
The radial head was carefully lifted again, and the graft was gently impacted into the medullary canal of the radial neck (Fig. 2B). The graft was left proud approximately 2mm over the radial neck to restore the length of the radius. Finally, the radial head was carefully placed over the graft, and the fixation was performed with three headless compressions 2.0mm cannulated screws. The initial reduction was maintained by the provisional application of pointed reduction clamps. Three 0.8mm Kirschner wires are inserted through the proximal radial head fragment towards the distal radius. Two K-wires started from the periphery of the radial head, focusing on the cortex of the proximal radius, and one was placed at the center of the head. The purpose was to avoid parallel application of the wires and create a trim tripod configuration. First, the cable’s position and length were checked using fluoroscopy. After that, the length of the screws was determined with the aid of the appropriate depth gauge placed over the inserted K-wires. A 1.8-mm straight cannulated drill was set over every Kirschner wire, and the proximal and distal fragments were reamed to enable bicortical fixation for the screw. The appropriate 2.0mm headless screws (22, 24, and 26mm, In2Bones SAS, France) were inserted sequentially until they were sunk below the chondral surface and the compression occurred (Figure 3A). Intra-operative imaging verified the final screw placement and flexion-extension, and pronation-supination movements ensured the fixation’s reduction and adequate stability. Wound closure was performed in layers, and a sterile dressing was applied.
The patient’s arm was placed in a sling. The first post-op day allowed active flexion and extension of the elbow and slight pronation and supination. The purpose is to obtain the full range of motion 6 to 8 weeks post-operatively.
After four weeks, the fracture eventually showed radiographic signs of healing. The patient was pain-free and regained full range of motion of the elbow joint at six weeks post-operatively. At 12 months follow-up, the patient remained pain-free and had 65 degrees pronation and 80 degrees supination. He had an elbow flexion ranging from 0 to 120 degrees, and the fracture site had fully healed (Figure 3B). He returned to his work and previous activity level without any complaints. The Mayo and Oxford elbow scores were 100/100 and 45/48, respectively.
Discussion
Isolated radial neck fractures usually occur after a fall on an outstretched arm1, and symptomatic radial neck nonunions are rare. The radial head lies exclusively intraarticularly and is wrapped and stabilized by the annular ligament to the sigmoid notch of the ulna. The blood supply to the radial neck is tenuous, with a branch coming from the recurrent radial artery, which commonly anastomoses with the radial collateral artery. The channel also receives a single small interosseous recurrent route that travels proximally to the radial head. In addition to these proximally migrating branches, the radial head is supplied via a vessel from the radial recurrent artery.8 Therefore, a fracture of the radial neck can disrupt the vascular supply to radial head fragments creating ischemic changes responsible for nonunion.
Conservative treatment is recommended for asymptomatic nonunions; the prognosis is excellent and with almost a full recovery.3 Even in patients with clinical symptoms, conventional treatment should be performed for at least six months.3 Operative intervention is usually reserved for patients with elbow dysfunction and achieves physically demanding work. However, no universally accepted treatment algorithm exists for the surgical treatment of delayed unions or nonunions of radial neck fractures due to the lack and inhomogeneity of the literature available. Consequently, three different operative treatment modalities are employed in case reports.3–7 These include bone grafting with or without internal ORIF, radial head excision, and prosthetic replacement.
The technique we describe is unique in that we obtain tripod fixation of the graft with the proper implementation of headless compression screws. It offers an adequate focus and less invasive technique than plating, avoiding the need to care for the safe radioulnar zone.9 The length of the radial neck is restored with the addition of the cylindrical iliac bone plug. We suggest using the following technique in all symptomatic patients, especially those who are active and in physically high-demanding occupations.
Conclusion
Radial neck fracture nonunions are rare and primarily asymptomatic, as shown in this report. However, operative treatment is warranted when clinical symptoms are present and full function of the elbow is required. The described method is a valuable addition to the therapeutic arsenal in the treatment of this type of nonunions, producing excellent results.
Authors’ contributions
LK is the first author and corresponding author, was involved in data curation, formal analysis, writing the original draft, reviewing, and editing the final manuscript. FZ, IB, NZ, IL, KD were involved in data curation, writing the initial draft, reviewing, and editing the final manuscript. AB is the senior and was involved in conceptualization, data curation, writing the original draft, reviewing, and editing the final manuscript.
Funding
None
Declaration of Competing Interest
None


_exposure_of_the_fracture_site_to_prepare_the_medullary_canal__(b)_insertion_of_the_cyl.jpeg)
_insertion_of_245_a_headless_compression_screw._(b)_anteroposterior_radiograph_of_the_e.jpeg)
_exposure_of_the_fracture_site_to_prepare_the_medullary_canal__(b)_insertion_of_the_cyl.jpeg)
_insertion_of_245_a_headless_compression_screw._(b)_anteroposterior_radiograph_of_the_e.jpeg)