Introduction
Schmorl’s nodes are herniations of the nucleus pulposus through the cartilaginous and bony endplate into the adjacent vertebra. Schmorl’s nodes are widespread and are typically seen as incidental radiographic findings.1 Rarely, Schmorl’s nodes can present acutely and symptomatically.2
In this case report, we discuss a man who presented with acute right-sided back pain and radiculopathy resulting from a tunneling Schmorl’s node. This is an unusual presentation of a Schmorl’s node, and similar cases have rarely been described in the literature.
Case report
The patient is a 63-year-old male who presented to the Emergency Department for a 4-day history of right-sided low back pain. Initially, he was evaluated via virtual telemedicine visit by his primary care provider and was prescribed a course of steroids. The steroids improved his pain, but he started experiencing intermittent numbness and tingling of his right anterior thigh with concomitant weakness of his right leg. He denied any inciting trauma or injury. He also denied weight loss, fevers, chills, bowel or bladder incontinence, a history of cancer, and IV drug use.
His physical examination was notable for 4/5 strength with the extension of his right leg, positive right-sided straight leg test, and minor gait changes to compensate for right leg weakness. The rest of his physical findings were benign. On laboratory testing, his CBC and CMP were unremarkable.
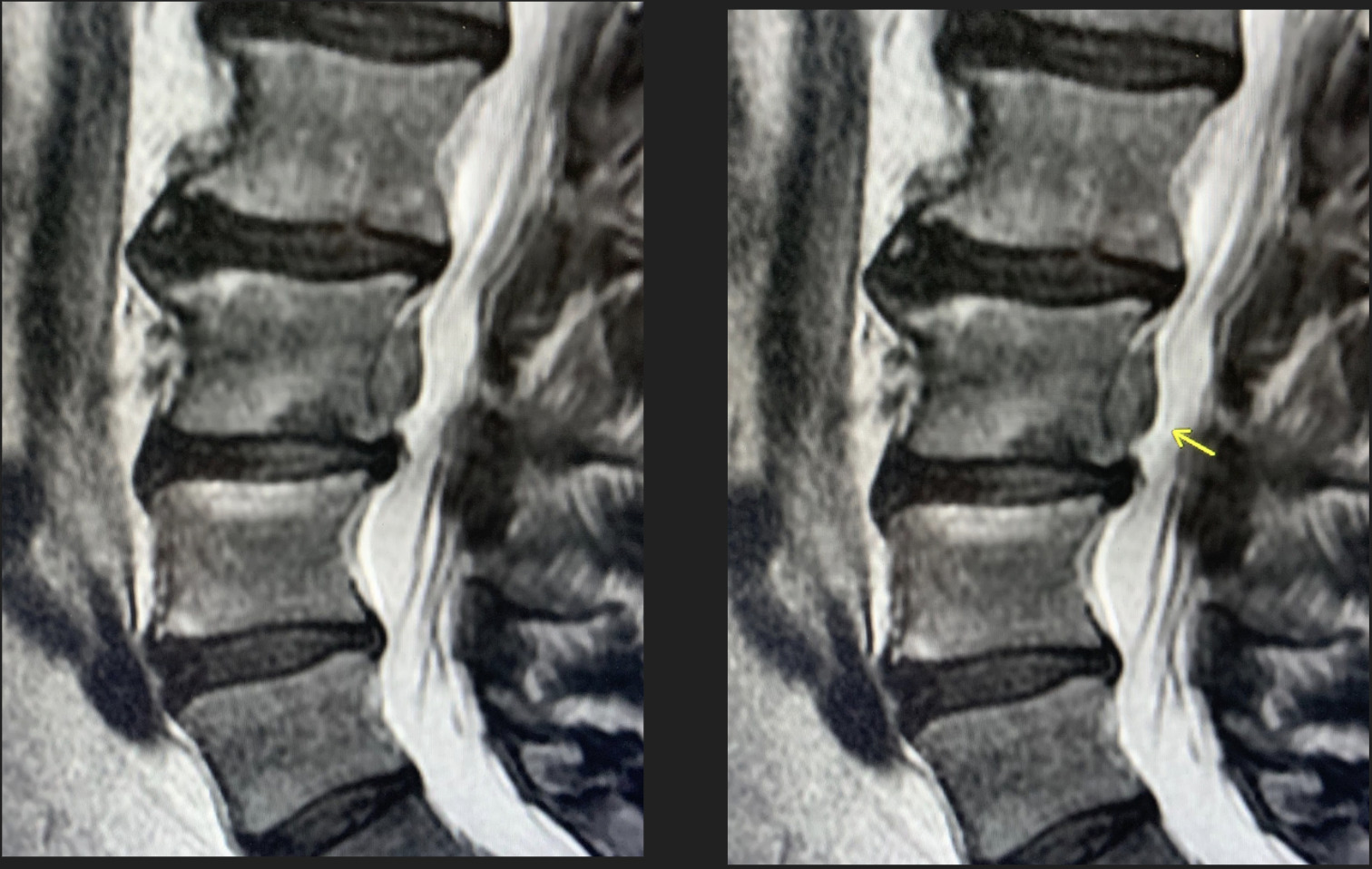
Imaging was performed with an MRI of the lumbar spine with and without contrast. The MRI (Figures 1-3) demonstrated a large L3 vertebral body inferior endplate Schmorl’s node with posterior extension through the vertebral body cortex. This Schmorl’s node extended into the ventral epidural space superiorly with severe effacement of the suitable L2-L3 subarticular recess, as well as the right L3-L4 neural foramen, impinging on the proper L3 nerve root. Additionally, there was surrounding cortical edema and enhancement, suggesting an acute Schmorl’s node.
The patient was discharged from the Emergency Department in stable condition and treated conservatively with acetaminophen and ibuprofen, intermittent ice and heat, and stretching exercises. He later returned home to be managed by his primary care provider.
Discussion
Schmorl’s nodes are prevalent incidental findings. Through postmortem studies, it has been estimated that greater than 70% of the population has Schmorl’s nodes.1 There is a male predominance in those affected, but the frequency of occurrence is similar in all ages.2
The pathophysiology behind the development of Schmorl’s nodes is still unclear. However, it has been hypothesized that these lesions may be related to intrinsic factors within the vertebral endplate, such as abnormal vascular development, ischemic necrosis, and ossification gaps. Other potential causes include direct trauma to vertebrae, intervertebral disc degeneration, and metabolic, neoplastic, and infectious processes. Regardless of the etiology, most Schmorl’s nodes are asymptomatic and found incidentally on imaging.3 Schmorl’s nodes appear on imaging as small, nodular, radiolucent lesions, often with a thin rim of sclerosis. These lesions are best seen on CT or MRI, but approximately one-third can also be seen on plain radiograph. On MRI, these lesions have T1 and T2 signal intensity similar to that of the intervertebral disc.1 Rarely, Schmorl’s nodes present acutely. In these cases, T1-hypointense and T2-hyperintense signals in the adjacent cortex indicate the presence of inflammation and edema.1,4 Acute Schmorl’s nodes may also peripherally enhance with gadolinium administration suggesting neovascularization. It is thought that this inflammation and vascularization, along with signaling from nociceptors in the vertebral endplate and disk annulus, are the cause of pain in acutely presenting Schmorl’s nodes.1 In the present case, the epidural extension of the Schmorl’s node also resulted in impingement of the L3 nerve root causing this patient’s anterior thigh numbness and tingling.
After diagnosis, a Schmorl’s node treatment is typically conservative in both asymptomatic and symptomatic cases.1,2 If conventional treatment fails, there is a wide range of treatment options available, including vertebroplasty, surgical removal of disk material, TNF-a inhibition, and neural blockade.2
Conclusion
In summary, we have presented a rare case of acute back pain with radiculopathy caused by a Schmorl’s node that violated the posterior vertebral body cortex. Although rare, Schmorl’s nodes can cause acute back pain and, even less commonly, radiculopathy.5,6 The imaging modality of choice for the diagnosis of a Schmorl’s node is MRI, as it has a more remarkable ability to detect edema, neovascularization, and in this case, extruded disc material.1 In both asymptomatic and symptomatic patients, the mainstay of treatment for Schmorl’s nodes is conservative therapy. Surgical removal of disc material has been successful in persistent radiculopathy from compression by a tunneling Schmorl’s node.1,2

_and_stir_(right)_images_demonstrating_a_schmorl_s_node_with_disc_materi.png)


_and_stir_(right)_images_demonstrating_a_schmorl_s_node_with_disc_materi.png)