Introduction
Discoid meniscus is a thicker and broader meniscus with an abnormal shape covering a more excellent tibial plateau surface than normal meniscus does.1–7 Discoid meniscus presents an irregular structural arrangement of the circumferential collagen fiber, making it more fragile and prone to a higher rate of a meniscal tear than the normal meniscus.7
The lateral meniscus is involved more frequently, with an incidence ranging from 1.2% to 5.2%.5 Medial discoid meniscus is estimated to occur in 0.06% to 0.3% of the population,4 being bilateral medial discoid menisci. However, cause some cases of discoid menisci may be asymptomatic or paucisymptomatic, it is hard to define the actual prevalence of medial bilateral discoid menisci.4
The standard treatment for symptomatic discoid menisci consists of partial meniscectomy. The current tendency to be very conservative in treating meniscal lesions should be applied to the discoid meniscus, too, so that the cauterization and suture of a torn discoid meniscus are gaining support.8
Case presentation
We present the case of a 13-years-old Caucasian male competitive football player referred to Our Institute with a diagnosis of bilateral medial discoid menisci. He complained that progressive pain in the left knee developed traumatically over six months, exacerbated by squatting, kneeling, running, or cutting movements, and was associated with recurrent knee joint effusion and sensation of popping or locking. In the right knee, the patients referred just a slight discomfort and an occasional feeling of popping without pain, flow, or limitation in daily activities.
Physical examination revealed knee joint effusion and medial standard line tenderness on the left knee. McMurray and Apley’s tests were positive for the posterior horn of the medial meniscus. A pretty normal range of motion (ROM) (0°-130°) was present with maximal flexion movements causing a painful click in the medial compartment. Laxity tests and patellar tracking were regular. There was no effusion or pain on the right knee, and a full ROM was present. Meniscal tear tests were negative, but the patient referred to a sensation of discomfort and popping in the medial compartment during maximal flexion movements. A Lysholm score of 59 and an International Knee Documentation Committee (IKDC) of 54 was recorded for the left knee.
MRI of both knees showed an enlarged saucer-like appearance of the medial meniscus in the coronal plane, extending into the intercondylar notch. In addition, a sizeable horizontal tear involved the posterior horn of the left knee’s medial meniscus, and intrasubstance degeneration signals were found in the right knee medial meniscus. MRI of the left knee also demonstrated the appearance of meniscal subluxation in the coronal plane (Figures 1 and 2).
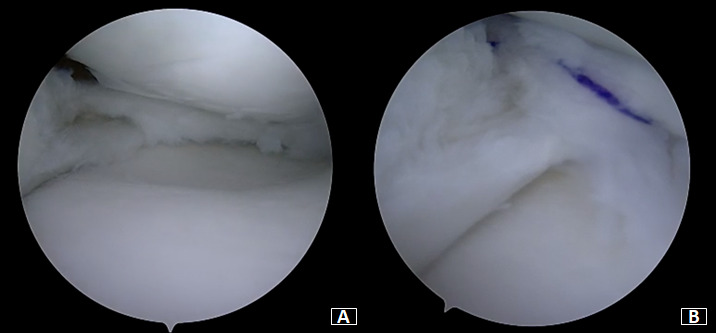
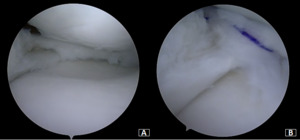
Under general anesthesia, a left knee arthroscopy using standard anterolateral and anteromedial portals. An incomplete type medial discoid meniscus with an atypical hypertrophic posterior root and an enlargement of the body and the posterior horn of the meniscus was found (Figure 3A). In addition, instability of the posterior horn, with a lack of rear tibial attachments, was observed (Figure 3B). Saucerization of the central discoid element was performed until an average meniscal width and semilunar shape was reached (Figure 4A). Two outside-in sutures with absorbable stitches were thus applied to repair the horizontal tear and stabilize the meniscus’s peripheral rim to the knee capsule (Figure 4B). A probe was used to assess the repair’s tightness and stability. Because the right knee was paucisymptomatic, no treatment was performed.
Partial weight-bearing with crutches and the knee in a full extension brace was allowed immediately. Isometric quadriceps exercises started on the first post-operative day. After three weeks 0°-90° and after five weeks, full ROM recovery was encouraged, together with progressive strengthening exercises. Return to the sport was allowed after three months.
At the final evaluation at seven months postoperatively, the patient has referred to the complete resolution of the symptoms without the sensation of popping or instability on his left knee. Full ROM and negative meniscal tests were observed. A Lysholm score of 94 and an IKDC score of 89 was reached. No worsening of symptoms in his right knee was reported.
Discussion
Since the first report by Cave and Staples in 19419 and the first bilateral discoid medial menisci documented by Murdoch in 1956,10 bilateral discoid medial menisci remains an extremely rare congenital pathology with an estimated incidence of 0.012%.4 The actual incidence of the discoid medial meniscus is difficult to determine because of its asymptomatic occurrence.5,6
The etiology of the discoid meniscus is controversial, and many theories have been postulated through the years. In 1948, Smillie et al.11 hypothesized that the discoid shape is a normal developmental stage during embryological development. The persistence of this shape during the fetal stage due to failure of absorption of the central portion leads to “congenital discoid meniscus.” Kaplan et al.3 suggested that discoid menisci developed due to an abnormal motion from the absence of the posterior tibial attachment. Raheel reported a case of familial discoid medial meniscus tears, present in three family members, suggesting a genetic association in the etiology.12
Discoid medial menisci seem to occur more frequently in male patients, with the most reported symptomatic cases in young athletic patients and many of them even more youthful than 18 years old.5
MRI is the recommended diagnostic method. The presence of a discoid meniscus is suggested by the occurrence of the “bow-tie” sign in >3 slices in the sagittal plane of MRI and by the ratio of the minimal meniscal width to the maximal tibial width >20% in the coronal plane.3 According to the Watanabe classification, the discoid lateral meniscus is divided into three types: complete, incomplete, or Wrisberg variant.13 Jordan et al.2 in 1996 classified discoid meniscus as stable (including both complete and incomplete types) and unstable (including regular and discoid meniscus). No specific classification for the discoid medial meniscus exists at this time.14
Cupping of the medial tibial plateau, hypoplasia of the anterior horn, abnormal insertion of the anterior horn of the medial meniscus into the anterior cruciate ligament, strange posterior horn attachment to the femoral condyle, pathological patellar plica, and meniscal cyst are common anomalies associated with the discoid medial meniscus.6,15 In the current case, an incomplete type medial discoid meniscus, with an atypical hypertrophic posterior root and an enlargement of the body and the posterior horn of the meniscus, was found. It was associated with a lack of posterior tibial attachments, which caused instability of the posterior horn and meniscal subluxation. A sizeable horizontal lesion was present. This is the first case reporting a selective enlargement of the posterior element with posterior root hypertrophy and associated instability to the best of our knowledge.
Patel et al.16 recommended preservation of the discoid meniscus in asymptomatic or minimally symptomatic patients and encouraged saucerization of a torn symptomatic discoid meniscus. Meniscectomy has been for many years the standard treatment for symptomatic discoid meniscus. However, different studies demonstrated that total meniscectomy increases the risk of osteoarthritis compared with partial meniscectomy.17,18 Nowadays, more conservative treatments are gaining support, being suture of meniscal tears and meniscal preservation even more popular. Arthroscopic saucerization and peripheral suture repair are also proposed surgical treatments for symptomatic discoid meniscus.5,8 Flouzat-Lachaniette et al.1 described four cases of discoid medial menisci treated with meniscoplasty, removing only the central part of the meniscus, and one case with associated meniscal repair demonstrating satisfactory results. Cho et al.19 reported a case of bilateral discoid medial menisci with unilateral symptoms. The patient was treated with good final results by cauterization and all-inside repair of the anterior horn tear. Similarly, in our case, we performed saucerization of the hypertrophic portions and suture of the associated lesions of the symptomatic discoid medial meniscus. Saucerization of the central discoid meniscus was performed first until a regular semilunar shape with a normal width was obtained. Unlike Cho et al.,19 which performed an all-inside repair of the anterior horn, in our patient, the repair was performed in the posterior horn, which appeared unstable and with a horizontal tear, through an outside-in technique.
Meniscal repair reached a consensus over the past decades, demonstrating an efficient alternative to meniscectomy. Nowadays, it is recommended to attempt a meniscal repair in all repairable tears, especially in active and young individuals.20 Arthroscopic repair should be considered even in horizontal meniscal and root tears because it provides good clinical outcomes.21,22 Ogawa et al.21 in 2020 demonstrated that although meniscus healing of horizontal tears may be poor, arthroscopic repair of the horizontal lesions should be attempted providing good clinical outcomes. The 2019 consensus on managing traumatic meniscus tears stated that numerous meniscus tears that were considered irreparable should be repaired.23 We believe that the same principle should apply to the discoid meniscus.
In agreement with the present literature,4,5,8,14,24 no treatment was performed in the right knee since paucisymptomatic. Indeed, conservative treatment is the preferred option in asymptomatic patients, and at the final follow-up, no worsening of the right knee symptoms was referred.
In conclusion, the bilateral discoid medial meniscus is a rare abnormality with uncertain pathogenesis. The conservative treatment is the preferred option in asymptomatic patients. Sauceriziation and eventual repair represent the surgical treatment in symptomatic individuals. Further research is necessary to clarify the optimum management and long-term consequences of such pathology.
Author Contributions
RI and DM: surgical procedure. EV and AR: follow-up of the patient and data acquisition. EV and SMP: manuscript preparation. RI and AF: critical revision for important intellectual content. All authors: final approval of the version to be published
Conflict of Interest
There is no conflict of interest.
The patient gave their informed consent before study inclusion.

_and_coronal_(b)_t2-weighted_mri_sections_of_the_right_knee__showing_incomplet.png)
_and_coronal_(b)_t2-weighted_mri_sections_of_the_left_knee__showing_incomplete.png)
_and_coronal_(b)_t2-weighted_mri_sections_of_the_right_knee__showing_incomplet.png)
_and_coronal_(b)_t2-weighted_mri_sections_of_the_left_knee__showing_incomplete.png)