INTRODUCTION
Knee osteotomies (KOs) are well-accepted procedures in treating unicompartmental osteoarthritis (OA) of the knee associated with valgus or varus malalignment. Established indications are constitutional deformities, over 3 degrees, inactive patients with unilateral osteoarthritis.1
While for unicompartmental arthrosis in varus knees, a high tibial osteotomy (HTO) is preferred; in the valgus knees, the gold standard is represented by distal femoral osteotomies (DFO).2
These procedures were abandoned mainly following the rise of knee arthroplasty (KA), which is today considered the gold standard in treating osteoarthritis (OA) of the knee. Knee osteotomies (KOs) were considered more demanding with unpredictable results and associated with higher rates of complications. However, in the last decades, the role of the malalignment correction in treating ligament injuries and knee balance and the development of osteoarthritis led to a re-evaluation of the osteotomies.3
Furthermore, patients with knee osteoarthritis (OA) are becoming younger and aim to perform more demanding activities. In such cases, preserving the native joint allows more physiologic knee kinematics ensuring an easier return to demanding activities. In addition, knee arthroplasties (KAs) have their limitations. They are not ideal for young individuals who play sports because of the possible higher risk of polyethylene wear, implant loosening, and risk of multiple revisions. These factors have brought back attention and increased the use of knee osteotomies, which could postpone or even avoid KAs.4–7
Similarly, better evidence-based guidelines for the selection of patients have been defined, new operative techniques have been developed, and improved fixation devices that provide superior stability have been introduced. As a result, many studies have demonstrated good clinical outcomes and survival rates after Knee osteotomies (KOs).8
Since osteotomies are performed more often in young patients and show good results in unicompartmental osteoarthritis, it is also important to evaluate among the clinical outcomes the Return to high-demand physical activity such as the Return to sport (RTS), because the inability to return to sport (RTS) can negatively impact the quality of life. The Return to sport (RTS) following knee osteotomies has historically been poorly investigated. There has been a greater interest in recent years, especially concerning high tibial osteotomy (HTO).9–11
Regarding distal femoral osteotomy (DFO), the data are scarce, lacking, unclear, and there is no systematic review examining this aspect.
OBJECTIVES
This study aims to investigate the Return to sport (RTS) following distal femoral osteotomy (DFO). The primary outcomes were the percentage and number of patients to return to sport (RTS) after distal femoral osteotomy (DFO). Secondary outcomes included timing, level, and frequency of return to sport (RTS).
MATERIALS AND METHODS
Study setting and design
A systematic review of the literature was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Search strategy and study selection
Cochrane database, MEDLINE via PubMed, Embase, and Scopus were searched using the keywords: “return to sport following distal femoral osteotomy” and their MeSH terms in any possible combination. In addition, the reference lists of selected studies were scanned to identify any additional studies for inclusion. The searches were performed up until April 1, 2021.
Inclusion and exclusion criteria
All the studies published as full-text articles in indexed journals, with all levels of evidence, which investigated the Return to sport (RTS) following distal femoral osteotomy (DFO), were included. Only articles published in English with available abstracts were included, without publication date limits. We excluded from the review double-level knee osteotomies (simultaneous osteotomies of the distal part of the femur and the proximal part of the tibia), surgical technical reports, expert opinions, letters to the editor, studies on animals, unpublished reports, cadaver or in vitro investigations, abstracts from scientific meetings, and book chapters.
Data extraction and analysis
Two authors (G.C. and L.P.) independently screened the data from the selected studies by reading the abstract. After excluding non-eligible studies, the full text of the remaining articles was evaluated for eligibility. To minimize the risk of bias, the authors reviewed and discussed all the selected writings, the references, and the articles excluded from the study. Any disagreements were resolved by consensus with the senior author (S.C.). At the end of the process, further potentially missed studies were manually searched for among the reference lists of the included papers and the relevant systematic reviews.
For each study included in the present study, the following data were extracted: study information (author, year, country, study design), demographic features (cohort, population size, sex, age, body mass index (BMI), comorbidities, surgical indication, and follow-up), any prior procedures, treatment performed, any other intraoperative process, complications, outcomes, further postoperative surgery, preoperative and postoperative activity and return to sport (RTS) information (percentages, time and level of RTS).
Statistical Analysis
The kappa value (k) was used to assess the agreement between the two independent reviewers in selecting articles. Agreement was classified as poor with k <0.30; partial with 0.30 <k <0.60; and total with k> 0.60. Due to the high heterogeneity between the studies; however, we conducted multiple indirect comparisons.
RESULTS
Literature Search
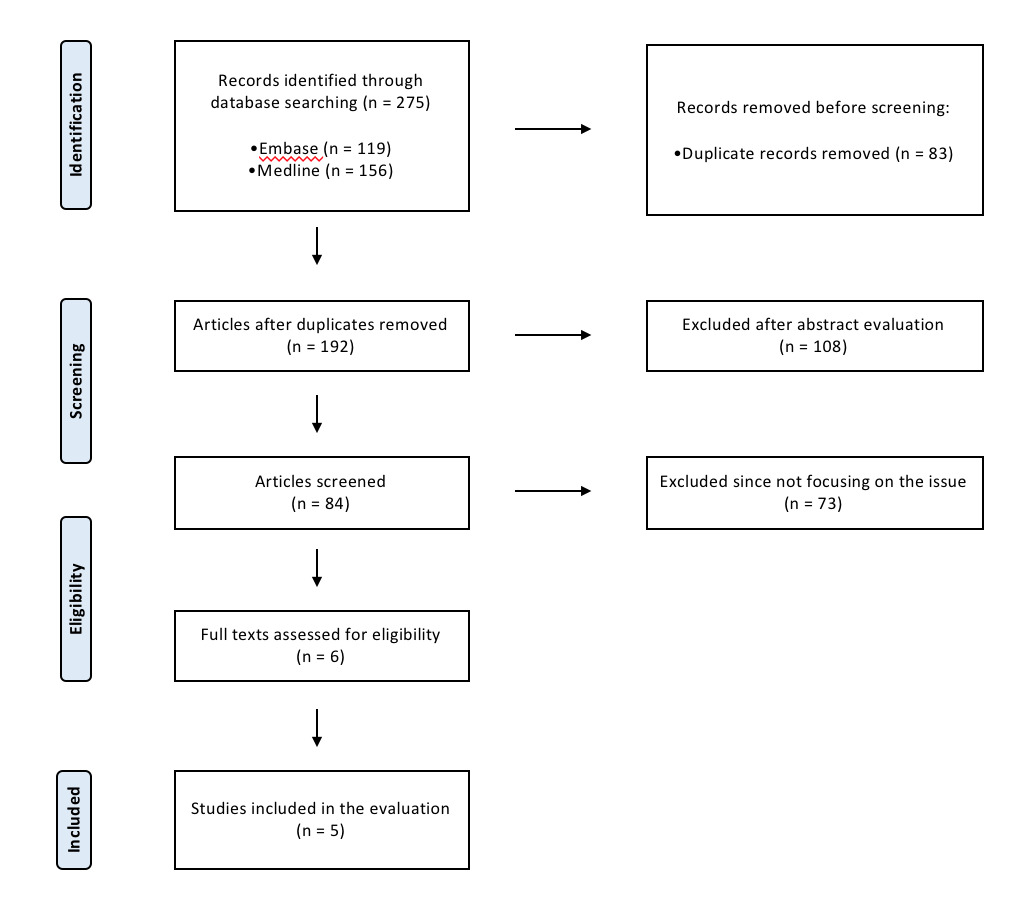
The initial literature search extracted 275 potential studies, as seen from the PRISMA flowchart (Figure 1).
Eight articles were identified after eliminating the duplicates and applying the inclusion and exclusion criteria. The senior author’s decision resolved one case of disagreement between the two independent reviewers. In addition, the citations of the included items were checked to look for any work that was mistakenly overlooked. We also removed from the analysis those studies where patients received double-level osteotomies (simultaneous osteotomies of the distal femur and proximal tibia) and where the information of RTS was not clear. In conclusion, of the 275 studies we included in our review, the five met the study inclusion criteria. In addition, we observed a high rate of reviewer agreement in article selection (k = 0.91; CI 0.90 to 0.92). The five articles included are all case series, retrospectively studied, published between 2012 and 2020 (Table 1).12–16
Four studies were performed in the USA and one study in Brazil. Two studies, coming from a single-center series, compared the Return to sport after isolated DFO and after meniscal allograft associated with DFO.
Demographic Data
A total of 84 patients and 84 knees underwent distal femur osteotomy. Unfortunately, 8 (9.5%) patients were lost to follow-up. Therefore, the total number of patients included in the study is 76 patients and 76 knees.
There were 30 men (39.5%) and 46 women (60.5%). Twenty-six patients (34.2%) came from a single study. The mean follow-up was 45.53 months. The mean age of patients at the time of surgery was 33.87 years. Patient BMI was specified in 3 studies (60%) and averaged 28.16 kg / m2. The mean valgus malalignment was 5.59°, the degree of valgus malalignment was not included in one patient.16
Prior surgery
In one case series, no information regarding previous surgical interventions was reported.15
While, in the other four studies, 92% (46/50) of patients had received a previous surgery on the ipsilateral knee before DFO. DFO was the first operation on the index knee in 8% (4/50) (Table 2).
Surgical Technique
In 70 cases (92.1%), patients received a lateral opening-wedge DFO, while in 6 cases (7.9 %), a medial-closing-wedge DFO was performed.
Other procedures
In one study, no further procedures were performed as a criterion for patient inclusion, while, in the other studies, any additional procedures performed are reported.12
In addition to the main procedure of distal femur osteotomy, 18 lateral meniscal allograft transplantations (MAT) were performed, of which 17 were from a single study as a criterion for inclusion of the study. Treatment of cartilage defects on the lateral femoral condyle in 29 cases (20 Osteochondral grafts, seven chondroplasties, one microfracture, one autologous chondrocyte implantation). Other procedures included ten partial lateral meniscectomies, one lysis of adhesions, patellar tendon debridement, one loose body removal. In addition, six medial compartment chondroplasties were done in one study, while in one other, three treatments of cartilage defects on the tibia (2 microfracture procedures, one debridement) were performed.
Intra-operative complications
In one case (1.3%) of lateral opening-wedge DFO. A fracture of the medial cortex of the femur was reported, which required further treatment with locking plate distal medial femoral.16
Postoperative complications
Eleven patients (14.5%) were reoperated before the final FU: meniscal debridement or meniscectomy in 3 cases (3.9%), hardware removal (one patient for symptomatic irritation underneath the iliotibial band, one patient before returning to competitive sports nine months after surgery, while in another it is unspecified) in 3 cases (3.9%), ACL reconstruction in 1 patient (1.3%), manipulation under anesthesia in 1 case (1.3%) and MAT and OAG revision in 1 case (1.3%), two years after DFO. Furthermore, 2 (2.6%) require TKA at 6.8 and 7 years after DFO.
Return to Sport
Of the 76 patients included in the study, only 65 performed sport before symptoms (Table 3).
56 (86.1%) returned to sports after DFO surgery. The average delay after which they returned to sports was 12.3 months. In one study, the average wait to return to sports was not reported.15 Individual studies report no statistically significant differences between patients treated with additional procedures associated with DFO and those with isolated DFO. The Return to the sport was investigated with different methods (Marx activity score, Lynsholm score, International Knee Documentation Committee Subjective Knee Evaluation Form (IKDC), Single Assessment Numerical Evaluation (SANE) score activity, VAS-Pain score).
The most commonly used score was the Marx activity score, administered in 3 studies (60%). In these series, the mean Marx activity score, at the last follow-up, was 7.6.12–14
Of the 56 patients who returned to sports after distal femur osteotomy, 43 patients (76.8%) resumed a level of activity equal to or superior to those practiced before the onset of symptoms.
Overall, 28 patients (50%) performed sporting activities at a strenuous level (collegiate or competitive level or endorsed participating in sporting activity at least four days out of every week) before surgery. All (100%) RTS and 22 (78.6%) resumed sports activities at the same level as before symptoms after DFO. In the series with the highest number of cases, no patients who perform high-level sports are reported before or after surgery.15
No, statistically significant differences were observed in the Return to sport rate between those who performed a lateral DFO and those who completed a medial closing-wedge DFO.
DISCUSSION
The most important result of our study concerns the high rate of return to sport following distal femur osteotomy. Fifty-six 65 patients (86.1%) resumed sports activities after an average follow-up of 12.3 months. Furthermore, 76.8% achieved an activity level equal to or superior to the one practiced before the onset of symptoms.
The study revealed a single case of intraoperative complication (1.3%) and 11 cases (14.5%) of postoperative complications; these results are similar to the other studies in the literature.17,18
In particular, the case of intra-operative complication involved a fracture of the medial cortex of the femur during a lateral opening-wedge distal femur osteotomy, which was fixed with a medial femoral plate. The patient, a collegiate women’s basketball player, returned to the sport after nine months from surgery. After 4-years of clinical follow-up, radiographs demonstrated stable alignment, and the patient was asymptomatic.16,19
These results demonstrate that DFOs can be a reliable treatment option, alternative to joint replacement in young patients with valgus knee deformities and symptomatic unicompartmental OA.
The present results are similar to another systematic review on the Return to sports activities after knee osteotomy (tibia and femur). The Return to sport rate was 85%, and a clear tendency toward a return to lower-impact sports emerged.20
Furthermore, specifically in the osteotomies of the distal femur, there are reported over 80% survival rates at ten years of follow-up for both opening-wedge and closing-wedge osteotomy, with a low complication rate.21–23
In the present study, there were no statistically significant differences in Return to sport after lateral opening-wedge and the medial closing-wedge osteotomies. Furthermore, no statistically significant differences were observed between isolated osteotomies and those associated with other procedures on the cartilage (such as osteochondral grafts, chondroplasty, or autologous chondrocyte implantation) or menisci (such as MAT or meniscectomy).
Regarding the nine patients (13.9%) who did not return to sport, it should be noted that the RTS rate was stratified by the level of demand of each mark; in fact, the return rate was almost complete for low-demand sports (golf, weightlifting, yoga) and lower for high-demand sports (Volleyball, football, tennis, basketball). In addition, the RTS rate was not related to more significant unilateral osteoarthritis or perioperative complications.
The present results are by Hoorntje et al., who found, in a single-center case series, a return to sport rate of 77% (65 out of 84 patients) within six months from distal femur osteotomy, showing a shift over time from a competitive or professional level to a recreational level sport activity.
We did not include this study in the article because 30% of cases were treated with combined osteotomy of the femur and tibia.24
Ekhtiari et al., in their study on the Return to sport following high tibial osteotomy, showed a return to sport rate of 87.2% (218 out of 250 patients). In comparison, 78.6% of subjects returned at an equal or greater level after HTO, and 89% returned to sport within one year.25
Regarding the specific RTS at a competitive or professional level, among the professional athletes involved in the study, a complete return to sport (100%) was observed at short to medium-term FU. In particular, in those patients, the RTS was at an equal or superior level than before the onset of symptoms in 22 of 28 (78.6%).
This probably indicates that professional athletes’ motivation and athletic training allow them to return to higher levels than recreational athletes.
When DFO was associated with MAT, a high rate of RTS was observed, 14 of 15 patients (82.4%) that came back to sports at an average of 16.9 months; however, less than a half (46.7%) were able to return to their preinjury level of participation. In particular, the RTS rate was stratified by the demand level of each sport: 100% low-demand, 72.7% medium-demand, and 53.3% high-demand sport.13
On this aspect, we agree with Myers et al., who stated that distal femoral varus osteotomy combined with MAT is a major surgical procedure that represents a salvage surgery for a knee that is deteriorating and heading for arthroplasty at some future point. The purpose of this surgery is not to return to high-demand sports instead reduce the progression of osteoarthritis by ensuring knee function by unloading the lateral compartment of the femur and eventually returning to recreational sports.26
Although these promising results, several concerns still exist on the surgical difficulties, the possible complications, and the deterioration of the outcomes at long-term FU.
However, as Mayfield et al., DFOs have satisfactory outcomes and high survival rates when the correct indications are followed. In particular, predictors associated with the failure of this technique are advanced age, hypertension, asthma, a diagnosis of osteoarthrosis, or traumatic arthropathy at the time of surgery.27
Furthermore, the medium-term results of TKA after KO are comparable to arthroplasty performed as a primary procedure. Still, crucial aspects of achieving satisfactory results are proper soft tissue balance and correct mechanical axis.28,29
Although reasonable rates of RTS after KA are reported in the literature, particularly after unicompartmental arthroplasties, the Return to high-demand sports is not recommended. In contrast, osteotomies preserve menisci and ligaments, thus ensuring more physiologic kinematics of the joint, which is of great advantage in high-demanding activities.30
For this reason, in our opinion, it is advisable to allow the use of distal femur osteotomy isolated or in association with other surgical techniques when we want to bring a patient back to athletic level sports, rather than knee arthroplasty.
The present study has several notable limitations. First of all, the included studies are only 5; they are retrospective case series, with short to intermediate follow-up and with no control group. Two of the five selected articles come from a single surgical case that investigates different aspects within the population; this may have created potential biases.
CONCLUSION
The Return to sport after the distal femur osteotomy is frequent (86.1%), with a mean time of almost one year after surgery (12.3 months). In most cases (76.8%), patients recovered to a level equal to or higher than that practiced before the onset of symptoms. However, while a return to the same or a higher level is frequent in athletes, there is often a return to lower impact sports in other patients.
ABBREVIATIONS
DFO: distal femoral osteotomy;
HTO: high tibial osteotomy,
IKDC: international knee documentation committee subjective knee evaluation form;
KA: knee arthroplasty;
KO: knee osteotomies;
MAT: meniscal allograft transplantations;
OA: osteoarthritis;
PRISMA: preferred reporting items for systematic reviews and meta-analyses;
RTS: return to sport;
SANE: single assessment numerical evaluation score activity.
Acknowledgments
None.
Ethical approval
The study design was approved by the Institute and School Council.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
All authors have disclosed a potential conflict of interests related to the publication of this manuscript. However, the authors also declare no competing interests.
Funding information
Publication costs are funded by the Orthopedic and Traumatology School of Università Cattolica del Sacro Cuore – Roma. However, the funders did not play any role in the study’s design, collection, analysis, and interpretation of data or manuscript writing.
Authors’ contributions
GC wrote the manuscript. GC and SC designed the study. GC, LP, MM, KC collected the data. SC, GM, and ASP are the authors who reviewed the manuscript. In addition, GC and KC provided data analysis. The authors approved the submitted version.