Introduction
Total knee arthroplasty (TKA) is one of the most reliable and successful surgical procedures in orthopedic surgery with high clinical outcomes in patients with symptomatic osteoarthritis.1,2
However, some complications after TKA may occur, and they could be very threatening for the patient. Among those are included all types of integumentary closure disorders, such as delayed wound healing, wound dehiscence, or skin necrosis which may lead to prosthetic infection or amputation.3,4
In general, systemic comorbidities (i.e., diabetes, collagen vascular disease, or obesity), chronic immunosuppression, smoking, and malnutrition lead to delayed wound healing, which contributes to higher rates of incisional dehiscence.5,6
Integumentary defects after knee replacement are difficult to manage, especially if the infection is deeper than expected and the prosthesis is already involved or if the bone or prosthesis is exposed.
The correct management of prosthetic infection should include a joint team of orthopaedics and plastic surgeons in order to allow the limb salvage, whose evolution would otherwise be, in many cases, amputation.7,8
Flaps have been widely used in orthopedic surgery for the management of congenital, tumoral9,10 and infectious diseases and on the basis of anatomical content, they can be divided into skin flaps, muscle, and myocutaneous flap, and fascia or fascio-cutaneous flap.11
Soft tissue coverage of the knee, in most cases, can lead to good functional and even aesthetic results, avoiding the appearance of bone sequelae and accelerating the healing process by providing adequate local blood supply with faster and complete absorption of antibiotics.
The choice of the type of flap is determined by many factors such as the general conditions of the patient, the concomitant injuries and pathologies, the possible functional sequelae, and of course by the type of wound the surgeon has to deal with.
We report a systematic review of the literature on the role of muscular flaps for the treatment of knee prosthetic joint infection. The review was performed to answer the following question: are muscular flaps useful for the management of wound dehiscence in prosthetic infection of the knee?
Material and methods
Study setting and design
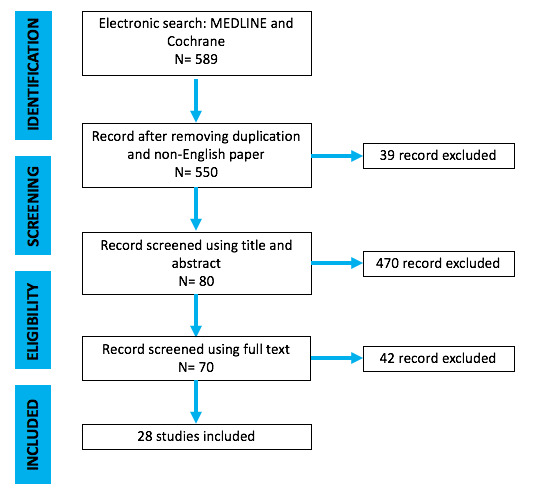
The present investigation represents a systematic literature review reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Figure 1).
Inclusion and exclusion criteria
In this review we considered the studies published as full-text articles in indexed journals, which investigated the value of muscular flaps for the management of knee prosthetic infection. Only articles written in English with available abstract were included. No publication date limits were set. Surgical technique reports, expert opinions, letters to the editor, studies on animals, unpublished reports, cadaver or in vitro investigations, review of the literature, abstracts from scientific meetings and book chapters were excluded from the present review.
Search strategy and study selection
Scopus, Cochrane Library, MEDLINE via PubMed and Embase were searched using the keywords: “muscular flaps”, “gastrocnemius muscle flap”, "vastus lateralis muscle flap ", “muscular”, “flaps”,“periprosthetic knee infection”, “knee prosthetic joint infection”, “Infected Arthroplasty”, “infected knee”, “two-stage revisions” and their MeSH terms in any possible combination. The reference lists of relevant studies were screened to identify other studies of interest. The search was reiterated until April 15, 2021.
Data extraction and analysis
Two independent reviewers (A.S and D.D.M) collected the data from the included studies. Any discordances were solved by consensus with a third author (G.R.). For each study included in the present analysis, the following data were extracted: year, types of research studies, demographic features, diagnosis, previous knee surgery, pathogens, treatment performed, possible complications and outcomes, follow-up. Numbers software (Apple Inc., Cupertino, CA) was used to tabulate the obtained data. Categorical variables are presented as frequency and percentages. Continuous variables are presented as means and standard deviation. Only one decimal digit was reported and was rounded up.
Results
After screening 589 articles by title and abstract, 70 were considered eligible for the full-text analysis. 500 articles were excluded because they did not fulfill inclusion criteria. Finally, 28 studies (Table 1) that met inclusion criteria were included in this review (Figure 1). All these studies had a retrospective descriptive design.
Overall, 345 patients (139 males, 206 females) suffering from TKA infection treated with muscular flaps were collected. The mean age was 57.3 years. Mean follow-up, reported in all studies, was 30.1 months (Table 2).
In most of the papers the patients were treated with TKA after diagnosis of primary osteoarthritis5,12–18 Only two articles specify the type of the implant.16,17
Infection timing was reported in 7 studies15,17,19–22 with a range of 10 days - 6.6 months.
Pathogens responsible for the infections were specified in 12 studies. The most common organism was Staphylococcus Aureus,12,14,15,18,21,23–26 followed by Pseudomonas Aeruginosa18,25,26 and Enterococcus.15,25 Only three papers mentioned antibiotic therapy administered to the patients.17,23,27 Most of the therapeutic choices were based on the susceptibility test and the results of the Antibiogram. Stiehl JB. et al.17 described initially the use of cefazolin as empirical treatment and later, as the isolation of the pathogens was completed, the therapy was then adapted and changed with ciprofloxacin + piperacillin-tazobactam. Whiteside et al.23 performed intraarticular administration of vancomycin or Gentamicin depending on the pathogens isolated during the microbiological investigations. Vancomycin was chosen also by Huang,27 who administered it for two weeks after the surgery.
As shown in table 2 different types of vascular muscle flap were reported for treatment of knee prosthetic joint infection: medial and lateral gastrocnemius muscle flap; vastus medialis and vastus lateralis flap; gracilis, hemy soleus flaps, rectus abdominis and latissimus dorsi free flaps.
Medial and lateral gastrocnemius were used in 270 patients. In the cases where a gastrocnemius muscle flap was performed, the outcomes were really satisfying, with (Table 3) the 93.9% rate of complete healing with no evidence of infection at last follow-up and all the wounds healed unremarkably. Regarding post-operative complications, a small percentage of patients treated with gastrocnemius muscle presented partial flap necrosis, reinfection and venous thrombosis (Table 3).
Among other flap options, latissimus dorsi was used in 28 patients,18,28 and a combination of medial gastrocnemius and hemi soleus flap was used in ten patients,29 both with a good outcome. Gracilis muscle flap was used in one case with a good outcome.30
Discussion
Total knee arthroplasty is a successful surgical procedure for the treatment of osteoarthritis, which leads to prompt pain relief and significant quality of life improvement in those patients who are suffering from osteoarthritis with severe clinical picture and a deep limitation of daily activities. For these reasons, TKA is among the most common surgery procedures, even today, despite the difficulties and the limitations due to the COVID-19 Pandemic.31 However, TKA is a greater orthopedic procedure, involving a massive surgical intervention and a complete substitution of the native articulation. Choosing this kind of procedure the surgeon knows the related risks, and the patient has to be informed as well.32,33 Among complications, one of the most insidious is the periprosthetic joint infection (PJI).
Wound healing complications of prosthetic knee replacement can lead to integumentary defects, prosthetic infection and poor clinical outcomes, even limb amputation. Skin necrosis and breakdown of the superficial wound without involvement of the deep layers or the presence of a wound sinus are relatively easier to solve, as long as the surgical team reacts quickly and accurately. Antibiotics are still the first line-therapy to face PJI, and even if they are necessary, sometimes they are not enough. As already said, few articles illustrated the chosen antibiotical protocol. Stiehl JB. et al17 described initially the use of cefazolin as empirical treatment and later, as the isolation of the pathogens was completed, the therapy was then adapted and changed with ciprofloxacin + piperacillin-tazobactam. Whiteside et al23 performed intraarticular administration of vancomycin or gentamicin depending on the pathogens isolated during the microbiological investigations. vancomycin was chosen also by Huang,27 who administered it for two weeks after the surgery.
The use of vacuum closure devices (VAC) can be considered to treat this type of complication and has precise purposes, such as reducing the size of the wound by eliminating exudate and reducing edema, producing granulation tissue due to increased local microvascular perfusion, improving the wound bed before rescue surgery, and allowing easier surgical wound closure procedures.34,35 The tissue produced by the VAC is an unstructured granulation tissue, without a scaffold, therefore it doesn’t allow a good defense against infection or trauma.36 For this reason, it cannot be a definitive treatment, and it is usually used only to close small wounds, or to prepare the wound bed before a definitive treatment such as a free skin graft or flap.37
Surgical procedures requiring a deep intervention on the tissues of the knee are vulnerable to cellulitis, abscesses and consequently more extensive tissue involvement and joint instability. If the wound dehiscence involves the fascial layer, the prosthesis exposure is most likely present, leading to a need for a muscle or myocutaneous flap, which is considered the gold standard treatment option.38 Muscle flaps help to control infection through the large vascular supply. Although many surgical techniques for plastic coverings have been described, the most used flaps are those found closer to the lesion.37 According to our systematic review of the literature the gastrocnemius flaps are the most frequent flaps used for the treatment of wound dehiscence of the knee because they have been traditionally considered effective. In fact, gastrocnemius flaps provide well-vascularized, bulky, and robust soft tissue coverage to obliterate dead space and provide a bed for wound healing and skin grafting in the setting of chronically infected wounds.38,39 The gastrocnemius muscle has a medial and lateral head, with independent vascular supplies, leading to the possibility to choose the muscle flap depending on the knee defect localization. It is widely accepted that the arc of rotation of the gastrocnemius muscle flap has sufficient reach to cover the middle and lower portion of the knee in both the anterior and posterior regions of the popliteal fossa. This is the gold standard option in case of necrosis and it is performed after the receiving region has been extensively sterilized and debrided, to prevent complications. The use of multiple drains is recommended to prevent fluid accumulation in the dissected space.40 These flaps have provided reliable results in covering exposed knee prostheses. A recent study by Warren et al41 reported a 42.3% of infection-free patients with a retained prosthesis after treatment at a mean follow-up of 5.3 years. Gerwin et al14 found that 11 of 12 patients (92%) who had medial gastrocnemius coverage of an exposed or infected knee prosthesis had an excellent outcome, with 10 of 12 patients (82%) retaining their prostheses or having a successful reimplantation. Nahabedian et al5 demonstrated that early aggressive debridement and irrigation of the wound with early muscle flap coverage, especially gastrocnemius, has 83% salvage rate.
The use of the vastus medialis and lateralis muscle with a proximal pedicle, is a common technique in the reconstructive surgery, such as the treatment of complicated ulcers in the pelvic girdle42 but its use for the knee coverage is not common and it is based on the studies of Wang and Swartz.43,44 However, a combination of the vastus medialis or vastus lateralis tibial attachments with a gastrocnemius muscle flap may be necessary to soft tissue coverage when there is a large anterior wound defect and the extensor mechanism or capsule have been affected. Whiteside et al23 used this surgical technique, combined with a distal expansion using a soleus flap in revision TKA with extensor mechanism deficiency.
The use of the soleus alone would have been insufficient due to the usual size of the wound defect, and also their combined use as bimuscular flap, helps to limit flexion and improve stability of a severely affected knee.45,46
An option within the musculocutaneous local flap is the pedicled gracilis muscle flap, as it provides long, thin and versatile muscle coverage with a vascular pedicle and minimal donor site morbidity. Jung AJ et al30 reported a case of soft tissue reconstruction using a reverse gracilis muscle flap, demonstrating its potency for knee area reconstruction or in addition to a medial or lateral gastrocnemius flap.
Free flaps may be the best treatment choice in case of an exposed or threatened prosthesis when local flaps are inadequate. Economides et al37 compared pedicled muscle flaps to fasciocutaneous flaps and found a comparable limb and prosthetic salvage rate. According to our review of literature, latissimus dorsi and rectus abdominis free flaps have been used for knee defects. A latissimus dorsi free muscle flap provides excellent coverage to the anterior knee because it has the potential to be quite large and it has a reliable blood supply. The rectus abdominis flap is another good coverage alternative which provides robust local perfusion. Cetrulo et al47 reported their experience using free tissue transfer, both latissimus dorsi and rectus abdominis, to reconstruct wound dehiscence after TKA. This study achieved 100% limb salvage and 91% prosthesis salvage in eleven patients presenting with exposed total knee arthroplasties using a combination of aggressive antibiotic therapy and microvascular free tissue transfer.
Conclusion
Given the increasing number of knee joint replacements globally performed every year, a careful evaluation of the optimal management for the treatment of possible complications remains of great importance.
The results reported by the different authors in the present review highlight the effectiveness of muscular flaps for the treatment of periprosthetic infection, in terms of function, limb salvage, prevention of the recurrences, cost-effectiveness, and quality of life postoperatively.
Muscle flaps provide an excellent management option for patients with persistent infection after knee arthroplasty.
Further, larger studies, with a randomized controlled design, may consolidate these findings.
Contributions
The authors contributed equally.
Conflict of interests
The authors declare no potential conflict of interest
Funding
The authors received no financial support for the research and /or authorship of this article.