Introduction
[Hip fusion (HF)] is an increasingly uncommon surgical procedure. It used to be a treatment option for young patients with severe damage to the joint and long-life expectancy, or with contraindications for [total hip replacement (THR)]. Advancements in hip arthroplasty, which leads to rapid improvement in pain and function, caused HF is regarded as a procedure with inferior outcomes to those of THR.1 However, there are also cases of non-iatrogenic HF, which might be a result of various pathologies, such as developmental dysplasia of the hip, inflammatory arthritis (eg. rheumatoid arthritis or juvenile arthritis), infectious or septic arthritis, or trauma (such as a proximal femoral fracture).2–4 Some patients do adapt to a lack of motion of the hip joint and may report optimal function for a long period – however, it is not without compromises. Many of them face significant limitations in activities of daily living, such as putting on shoes, climbing stairs, and driving a car, and report that their condition also affects their sexual life – all of which contribute to a generally lower quality of life.1,4
In patients with hip fusion – either iatrogenic or of another origin – the development of secondary degenerative changes in adjacent joints seems inevitable. After 20-30 years, most of them tend to complain about pain in the lumbar spine, contralateral hip, and ipsilateral knee, which is true even for those who have had their hip fused in an optimal position.3 Degenerative changes in the ipsilateral knee following hip fusion are estimated to appear in up to half of the patients.5 Knee arthritis in these cases is a result of abnormal gait pattern, which results in overloading of the ipsilateral limb during a stance phase when the knee compensates increased pelvic rotation and lack of motion in the hip.1
Currently, there is no general standard of care or guidelines which could serve to inform the decision process of joint replacement surgery in patients with hip fusion undergoing joint replacement due to secondary arthritis. A surgeon must evaluate each case individually and carefully plan further procedures, especially in patients with significant comorbidities, where their burden should be minimized. On the other hand, the surgeon has to consider options that would lead to the best possible function for the patient, especially if the patient has the potential for a positive postoperative outcome.6 [Chronic kidney failure (CKD)] is a progressive disease, which leads to the [end-stage renal disease (ESDR)], defined as [glomerular filtration rate (GFR)] less than 15 mL/min per 1.73 m. In such patients, several factors associated with this condition have to be taken into account in the preoperative planning, such as the increased risk of cardiovascular complications, perioperative fractures, anemia, altered hemostasis, electrolyte status alterations, and scheduling of the dialysis.6,7 Hereby we present a case of a 70-year-old male with spontaneous HF and knee arthritis, who successfully underwent conversion from hip fusion to THR and subsequent [total knee arthroplasty (TKA)].
Case report
Preoperative assessment
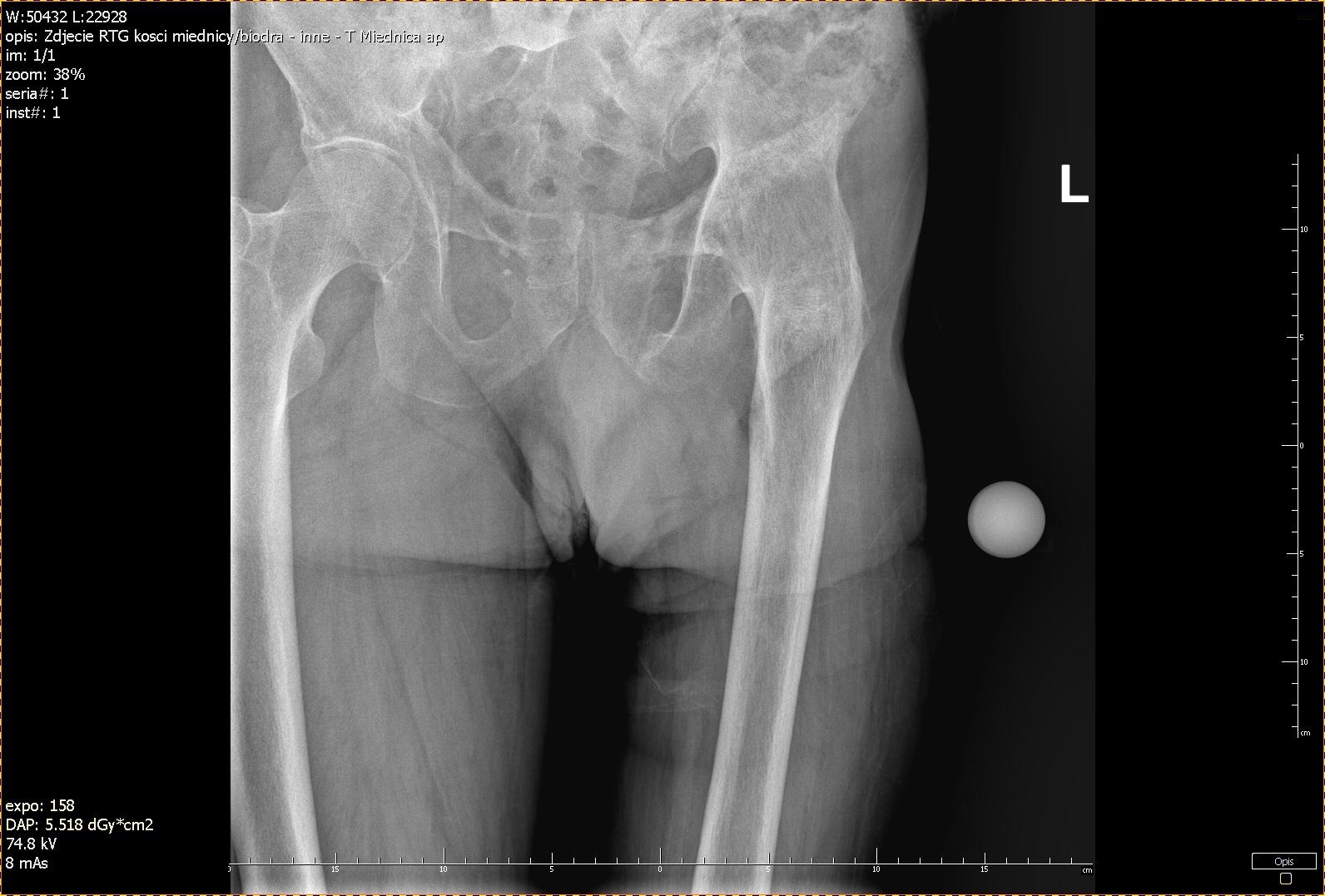
A 70-year-old male presented in the Orthopedics Clinic on the 25th of April 2019, with debilitating pain in the left knee. Apart from limitations in his daily activities, the patient complained about difficulties in driving a car, walking longer distances above 1km, excluding him from recreational activities. The patient had tuberculosis at a young age, which led to the spontaneous fusion of his left hip. On physical examination, the hip was immobile, fused in 10◦ flexions, 0° rotation, and 5° abduction, with no movement in the joint. The left knee had limited mobility to 70° flexion, and flexion contracture of 8° was present, as well as positive Solo-Halla’s and Zohlen’s signs and a sense of friction was felt during the knee movements. Leg length discrepancy measured 3 cm. The strength of the muscles surrounding the hip was evaluated according to Lovett’s scale: flexion - 3; extension - 2; internal and external rotation - both 1.
The [computed tomography (CT)] scan of the lower limbs revealed generalized osteoporotic changes, left hip ankylosis, past fracture of pelvic bones (partial union of the left side of the sacral bone, and a non-union of the upper and lower branch of the pubic bone), atrophy of lower limb girdle’s muscles on the left side, and also considerable degenerative changes in the lumbar spine, non-significant degenerative changes in the right hip joint and focal osteolysis in the sacral bone on the right side – indicative of a brown tumor, which was related to chronic kidney failure as well as generalized osteoporotic changes.
Taking into account the findings of physical examination and the CT scan, performing TKA without conversion from HF to THR was not considered a good option. From a biomechanical point of view, mobility of the hip joint is necessary to preserve a normal gait pattern, which has an impact on prosthetic material durability as well as the rehabilitation process. In this case, a perspective of revision surgeries, which could have been a result of avoiding THR, had to be minimized due to ESRD. Taking into account his general good condition, after consulting with nephrologists he was qualified for a 2-step surgical joint replacement procedure – with conversion to THR and TKA 6 months after the first procedure. The therapeutic options and associated risks were also discussed with the patient before obtaining his consent for the management plan. The patient has signed informed consent for these procedures and the publication of his case.
Hip fusion takedown – surgery and technique
Hip joint reconstruction followed by arthroplasty was performed on the 26th of April. The electrolyte status and hemostatic parameters were checked on the day before and were within normal limits. Blood count showed [hemoglobin (HGB)] and [red blood count (RBC)] slightly below normal limits (12,70 g/dl; 4,1 M/uL). The hematocrit was kept at around 30% in the whole pre-and postoperative period to decrease the risk of bleeding.
The patient was placed on the operative table on the lateral side. A postero-lateral transtrochanteric approach was used to access the left hip joint, as it allows the best visualization of the hip and acetabulum. Osteotomy of the femoral neck was performed with the guidance of an X-ray and Kirschner wire; afterward, the bone was cut. The acetabulum was cleaned from fibrous tissue under control of fluoroscopy before acetabular cup placement of 52 mm, with additional fixation with 3 screws. A polyethylene n◦23 (32 mm) was then placed under an acetabular cup. Femoral bone was reamed and a non-cemented stem n◦5 was inserted with a metal head (n◦4 - 32mm). The total duration of the surgery was 1,5h. 12h after surgery anticoagulant was administered nadroparin 5700 IU (Fraxiaprine 0,6mL). The day after surgery a blood count was performed – with HGB and RBC slightly below normal limits (10,30 g/dL and 3,4 m/ul). On the following day, there was a small decrease in blood count parameters (RBC – 2,9 M/ul, HGB - 9 g/dL). A drop in these parameters might be expected in the case of patients with ESRD. Nevertheless, the patient remained asymptomatic and did not require transfusion. On the 3rd postoperative day, the patient was able to perform active and isometric exercises, as well as breathing exercises. The patient began to ambulate on the 4th postoperative day using crutches. He had hemodialysis scheduled every three days during the hospitalization period. The rest of the postoperative period was uneventful. He was discharged home on the 7th of May and referred for further rehabilitation outside the clinic, and instructed not to bear weight on the operated limb until the follow-up visit on the 3rd of June.
Total knee arthroplasty
The patient was admitted again to our clinic on the 12th of September for TKA. The patient signed a separate informed consent for this procedure. An anterior approach was used. A cemented implant with an antibiotic was used. The patient was able to walk using walking aids on the 3rd day following TKA. The time to perform the procedure was 1,2h. The blood count parameters – RGB and HGB were only slightly below normal limits after surgery (3,0 M/ul, 9,4 g/dL), and electrolyte status was within normal limits. Anticoagulants were resumed 12h post-surgery, as during the previous hospitalization. Hemodialysis was scheduled every 3rd day during the hospitalization period. The patient was discharged on the 18th of September and instructed to walk without weight-bearing on the left lower limb until the follow-up visit, which was scheduled for the 2nd of October.
At the latest follow-up visit on the 29th of December, 2019 patient presented pain-free. His range of movement has dramatically increased. Hip joint’s range of motion – flexion 110°, extension – 10°. external and internal rotation – both 35°. Knee joint – flexion 110°, with no flexure contracture present. The patient was asked to evaluate his [quality of life (QoL)] using a [visual analog scale (VAS)] – in increased from 30/100 (measured preoperatively) to 85/100 after both procedures. He was generally satisfied with the results and declared he can drive a car without limitations and walk longer distances (above 1km).
Discussion
Joint replacement surgery in a patient with HF is challenging not only from the technical viewpoint, but also due to multiple factors that a surgeon has to consider in the perioperative planning such as affected joints and ailments, the patient’s expectations, the needs related to his everyday functioning, and comorbidities. In a patient with HR and degenerative changes in the ipsilateral knee there are three options – performing TKA alone, conversion from HF to THR with TKA as a next procedure, or conversion of the fused hip to THR without TKA.
The knee joint in patients with hip fusion is subjected to excessive load, which leads to premature degenerative changes. According to the literature, arthritic changes become evident on average after 2-to 3 decades after hip fusion.3,8,9 Conversion from fusion to hip replacement alone may relieve some stress put on the knee joint and consecutively- the pain, at least to some extent. Nonetheless, it is not curative, as it is unlikely it will influence the natural progression of the degenerative changes in the knee joint.
Few circumstances are allowing to perform TKA alone in a patient with a fused hip. Beaule et al. indicated that this therapeutic option should be offered only to patients with hip fused in a proper position, which authors define as flexion of 20° - 30°, adduction of 5°, external rotation of 5° - 10°, and an insignificant limb length discrepancy (<2 cm).1 We identified several case reports to support this claim – for example, a report of a patient with intense scarring of soft tissues surrounding the hip after an infection caused by fusion and in an 87-year-old with multiple comorbidities with significant pain relief after TKA alone, and all of them described patients with the hip fused in an acceptable position.4,5,10–12 Another approach was described by Koo et al., who concluded that only patients with lower back pain should undergo conversion from HF to THR before knee replacement surgery – but we did not find any other publication to support this claim.11 Other authors demonstrated that the outcome of TKA alone is not as predictable and is most likely to provide an unsatisfactory outcome. In a study involving 18 subjects with a hip fusion performed 33 years before (on average), in patients who underwent TKA following THR, [Hospital for Special Surgery (HSS)] knee score improved from a mean of 33 to 78 points, whereas in those undergoing TKA alone – from 35 to 44 points.9 There are also other issues that a surgeon might face when deciding to perform TKA alone in patients with HF. First of all, the improper alignment of the fused hip, with increased internal or external rotation, precludes proper positioning of the prosthetic material during TKA,5 and as a result, it leads to premature wear or loosening of the prosthetic material.8,11,12 Secondly, the rehabilitation process of the knee would be difficult with a stiff hip, partly because of increased tension of the muscles crossing both hip and knee, which is best relieved by arthroplasty of the hip. From the patient’s perspective, usually, recovery from THR is less painful than after TKA and as a result, it would positively influence the patient’s attitude towards the second procedure of knee replacement.3 Additionally, retaining hip fusion will not address the limitations in simple activities of daily living patients face, including putting on shoes and socks or climbing the stairs.1,4 Importantly, HF also contributes to technical difficulties in performing TKA itself, because a stiff hip will not allow knee flexion to the extent required for elements placement during TKA – so multiple modifications of the surgical technique might be necessary.5,10,11
On the other hand, a surgeon must bear in mind that conversion to THR is related to a higher complication rate than primary THR and even revision THR, such as infections, intraoperative fractures, sciatic nerve damage, dislocations, and a need for revision surgery.13–15 A study by Richards et al. found that the complication rate in HF conversion might be as high as 53%.14 In a systematic review of 1,104 hips by Jauregui et al.,15 where patients had their hip fusion for 27 years on average, the infection rate was 5,3% for patients undergoing conversion (vs. 1% for primary THR and even revision THR), instability from 2,6% to 15% (vs. 1,5 for primary THR), and revision surgery were necessary for 12% of the patients. Also, nerve-related complications (mainly sciatic nerve palsy) occurred in up to 4,7% of cases, as opposed to only 1-3,7% in the group undergoing primary THR.
Although it is not possible to eliminate the risk of complications entirely for fusion takedown and subsequent conversion, there are a few factors that, when taken into account in preoperative planning, might significantly decrease it. In general, poor gluteus muscle function is considered a contraindication for fusion takedown, making their evaluation an essential step in the preoperative examination. The function of these muscles is crucial for the success of conversion and limp-free gait with negative Trendelenburg’s sign.2 It is best evaluated by simple palpation of abductors before surgery, as the electromyography results do not correlate with intraoperative findings.1,11 Therefore, we encourage assessment of their function and strength preoperatively for e.g. using Lovett’s scale. In a retrospective study including patients after hip fusion takedown, patients with poor abductor function before conversion had to use walking aids in 74% of the cases, while they needed none before fusion takedown, and more than 15% required revision.16 Interestingly, the result was evaluated by patients themselves as good and excellent 76% of them. However, in another study by Kilkgus et al. patients used fewer aids after conversion, and none of the patients required revision,17 which we suppose might be due to better abductor function in this group. Another important factor is limb length discrepancy that has to be corrected to prevent limping in the patient and decrease pain.
The approach used during hip fusion takedown also has to be taken into account. Celiktas et al. suggested that the posterior approach is best, as it minimizes the risk of serious complications, such as abductor muscles damage and heterotopic ossification; however, it is related to a very high risk of perioperative fractures, which occurred in 5 out of 28 patients and prolonged operative time [133 min on average].2 In our patient with advanced osteoporosis related to ESRD and the presence of pelvic injury evidenced by CT scan, we decided that such risk was unacceptable and we opted for the lateral transtrochanteric approach, which allowed better visualization of the operative field and shorter duration of the surgery (90 min in our case).
Another important aspect, that is not always taken into consideration, is the management of patient expectations. Richards et al. showed that although the outcome for conversion to THR and revision THR were comparable, the latter group rated their satisfaction as very high despite low QoL scores, whereas the first group was generally not satisfied with the procedure, although all of them had complete, or nearly complete resolution of their symptoms.14 We agree that patients’ expectations should be tempered if they seem unrealistically high. A detailed discussion with the patient on possible outcomes before surgery should never be avoided.
Several reports were published to discuss the results of patients with combined fusion conversion to THR and TKA (including bilateral surgery).3,8,9 In a series of Romness et al., 12/16 patients with fusion takedown with THR and TKA performed later with a mean follow-up of 5,5 years, patients with THR had a slightly lower range of motion postoperatively than patients with TKA alone (3-72 vs. 0-83), but both groups showed similar improvement of HSS knee score (from 28 to 72,2 and 43,5 to 72,1 respectively). However, the authors mention that the group with conversion to THR before knee replacement had more advanced arthritic changes in the knee, as evidenced on radiographs.8 The authors also stated that the numbers are too small to conclude that TKA alone is superior to a combination of THR and TKA. This is particularly important because in another study by Rittmeister et al. contradictory results were reported, and in his series, patients with TKA alone had poorer outcomes.9 Taking all of the factors described above into account, as well as the individual features of our patient, such as good abductor muscles, state on palpation, the advancement of knee joint degeneration evidenced on CT and by X-ray, and his overall condition - despite ESRD which was well controlled in his case - he was concerned a good candidate for both conversion to THR and knee replacement surgery.
As for patients with ESRD, there are a few additional precautions that an orthopedic surgeon must bear in mind before a joint replacement procedure. Although it is well-known that advanced renal disease is related to higher mortality and morbidity, it is not a contradiction for joint replacement surgery.6 Nevertheless, patients have to be informed that the risk is higher than in the general population -although some studies have shown conflicting results.6,7 This is true primarily for patients awaiting renal transplants and undergoing hemodialysis, and a joint replacement surgery has to be offered for those who most likely will benefit from the surgery.6 For dialyzed patients, it is vital to synchronize the procedure with hemodialysis to correct any volume, electrolyte, and acid-base imbalances before surgery, as this decreases the possibility of complications such as significant bleeding. The use of heparin may be minimized or avoided in the preoperative hemodialysis, and regular hemodialysis should be performed three times a week after surgery. Keeping the HCT around 30% also reduces bleeding risk. If a blood transfusion is required, it should be coordinated with the patient’s hemodialysis to decrease the possibility of volume overload, but it has to be considered only if the HGB level drops below 7-8 g/dL in asymptomatic and below 8-10 g/dL in symptomatic patients,7 therefore, this was unnecessary in this case. Nonetheless, a surgeon always has to take such a possibility into account while planning surgery involving major joints in an ESRD patient. On the other hand, it is worth noting that heparin should not be administered preoperatively, but it should be resumed 12h after the procedure. In the case described above, we chose nadroparin 5700 IU (Fraxiparine 0,6mL) as this is a standard in such patients in our practice. Cardiovascular risk factors, and concomitant hypertension is also important for planning anesthesia, which should be discussed thoroughly with anesthesiologists. If these precautions are taken, then the risk of major complications is minimized.6,7
Conclusion
Patients who develop knee arthritis as a result of ipsilateral hip ankylosis might find substantial pain relief with joint replacement surgery, but it might require a 2-step intervention consisting of fusion takedown with THR and TKA spaced in time. Given the fact that there is no current standard of care for these patients, a surgeon has to evaluate each case individually to propose solutions with the best outcome possible. Due to the limitations of current techniques, the patient has to be well-informed of the possible outcomes and risks of complications associated with each solution, and they should be involved in the decision-making process. Although this is a single case report, and definite conclusions cannot be drawn, we hope that this detailed report will facilitate the decision-making process for orthopedic surgeons facing similar challenges.
Authors’ contributions
Conceptualization, TP and MH.; methodology, TP and WK.; formal analysis, WK, and MH; investigation, TP.; data curation, MH.; writing—original draft preparation, MH.; writing—review and editing, WK, TP and MH.; visualization, WK.; supervision, TP. All authors have read and agreed to the published version of the manuscript.
Consent
Written informed consent for proposed treatment was obtained from the patient, as well as for each surgical procedure individually. A separate consent was taken for publishing this case.
Disclosures
The authors report no conflicts of interest in this work. The authors have no affiliations with or involvement in any organization or entity with any financial interest, or non-financial interest (such as personal or professional relationships), in the subject matter or materials discussed in this manuscript.
Funding
No funding was received for this research as well as for writing this manuscript.