Background
Despite recent improvements in peri-operative pain control and rapid recovery, up to 20% of TKA patients are not satisfied, mainly due to persistent pain.1,2 While gross instability manifesting as pain is the second most common reason for revision,3 subtle instability and altered knee kinematics manifesting as pain in daily activities are likely causes of inadequate patient satisfaction. Various tibial insert designs have been created attempting to mimic native knee kinematics to attempt to improve function and satisfaction while avoiding complications.
Traditional cruciate-retaining (CR; Figure 1) and posterior stabilized (PS; Figure 1) designs have demonstrated excellent survivorship4,5 including data from multiple registries.6–8 However, CR knees have been reported to have abnormal knee kinematics secondary to paradoxical motion (lack of rollback, paradoxical forward femoral motion, and rotational pivot mechanics with the pivot potentially in the lateral compartment)9 due to non-anatomic surfaces.10 Drawbacks to PS knees include additional bone resection for the cam and post mechanism, which increases the risk of condylar fracture.11 In addition, post failure and patellar clunk syndrome12 are also potential drawbacks.
Anterior stabilized (AS), bicruciate retaining (BR), bicruciate stabilized (BCS), and medial pivot (MP) inserts have been developed to improve stability, with the intent of improving patient satisfaction. AS (Figure 1) inserts intended to be utilized with a CR femur with or without a competent posterior cruciate ligament (PCL) have a deeper, more conforming geometry that is aimed to improve kinematics. However, the increased conformity can result in higher medial and patellofemoral contact pressure and wear.13,14 Despite these concerns, no significant differences have been noted between AS and traditional CR or PS outcomes in most clinical studies.15
MP (Figure 1) inserts incorporate a medial deep-dish portion and a relatively flat lateral side in an attempt to recreate the native tibial plateau geometry and medial pivot knee kinematics.15 Improved patient satisfaction has been reported with MP design, but there have been concerns reported regarding the potential for stiffness and increased wear due to the increased medial conformity.15 However, some studies have also shown no difference in need for MUA.16
BR designs require preservation of an island of bone for retention both the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL), in order to theoretically retain near-normal knee kinematics.17,18 However, there have been notable complications associated with the BR design including early failure, lateral pain, stiffness, and tibial island fracture.17,18
BCS inserts use an asymmetric cam-post mechanism in an attempt to restore more normal knee kinematics.19,20 This device also utilizes a more congruent medial compartment and a more concave lateral compartment, like the MP design. These features allow more external rotation and accommodate high flexion, which help approximate normal kinematics; however, there have been concerns about lateral knee pain and posterior positioning of the femur leading to quadriceps inefficiency.21,22
The six different fixed bearing polyethylene insert designs discussed above have significant differences in design and kinematics. Multiple RCTs have compared two polyethylene insert designs8,13,14,17–37 but a trial comparing all six designs has not been conducted to date, partly due to a lack of feasibility. So, there is a paucity of level I evidence on comparative safety and efficacy of various tibial insert designs.
The aims of this study are to evaluate the comparative efficacy (patient reported outcome scores, range of motion, and patient satisfaction) and safety (reoperation and MUA) of six different fixed bearing polyethylene insert designs, using network meta-analysis (NMA) of randomized controlled trials (RCTs).
Methods
Literature Search
We searched for relevant studies in the Medline, EMBASE, the Cochrane Library, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Controlled Register of Trials (CENTRAL), and Institute of scientific information (ISI) Web of Knowledge, from inception to February 2021. All searches were limited to randomized controlled trials in humans published in English language. The following search terms were applied for systematic searching: “total knee arthroplasty” OR “knee replacement” AND “ultra-congruent” OR “deep dish” OR “anterior stabilized” OR “medial pivot” OR “medial stabilized” OR “ball and socket” OR “posterior stabilized” OR “cruciate retaining” OR “posterior stabilized plus” AND “randomized controlled trial”.
Study selection
Inclusion criteria were RCTs comparing two or more fixed bearing polyethylene inserts used for patients with primary knee osteoarthritis and reporting patient reported outcomes at minimum 6-month follow-up. Exclusion criteria were study design other than RCT, studies with inflammatory or posttraumatic osteoarthritis. Title and abstract screening were performed by two authors and full texts of all selected studies were then reviewed for selection confirmation. Any disagreements were resolved by discussion.
Included studies
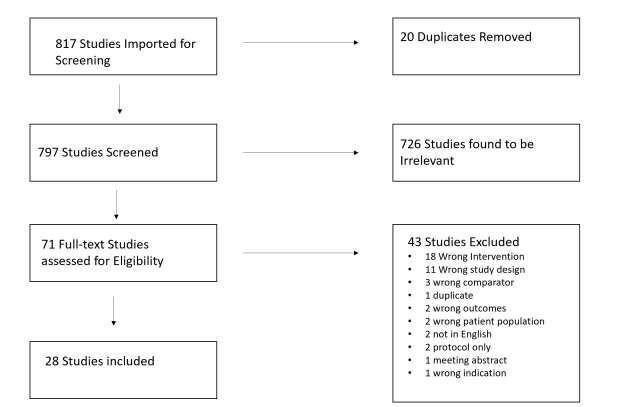
As shown in the PRISMA flow diagram (Figure 2) 817 studies were identified from database searches, and after removing duplicates, 797 were screened for inclusion. The abstract and title review yielded 71 articles that required full-text review. Of these, 28 met inclusion criteria for the systematic review and meta-analysis. One of these 28 studies excluded as it was a further follow-up of a previous trial leaving 27 trials in total.32
Data Extraction
The data was independently extracted by two reviewers using web-based systematic review program, Covidence (www.covidence.org, Melbourne, Australia). The following information was extracted from the included articles: first author, year of publication, patient demographics, insert designs, patient reported outcome scores, range of motion, satisfaction and adverse events including manipulations and reoperations. Any disagreement concerning the data extraction was resolved by discussion.
Assessment of Study Quality
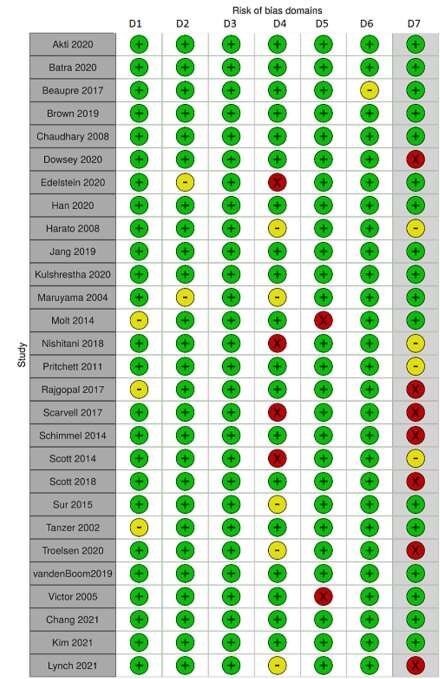
Two authors assessed the risk of bias of all included studies using the Cochrane Collaboration Tool Risk of Bias Assessment Tool (Robvis).38,39 The tool assesses the risk of: selection bias (“sequence generation” and “allocation sequence concealment”), performance bias (“blinding of participants and personnel”), detection bias (“blinding of outcome assessment”), attrition bias (“incomplete outcome data”), and reporter bias (“selective outcome reporting”).40,41 The risk of each individual bias was assessed as high risk, low risk, or uncertain risk.
Statistical Analysis
Continuous variables were expressed as mean and standard deviation. Dichotomous variables were reported as odds ratios. When standard errors of the mean or median and range were provided, we calculated the standard deviation by the method described by Hozo et al.42
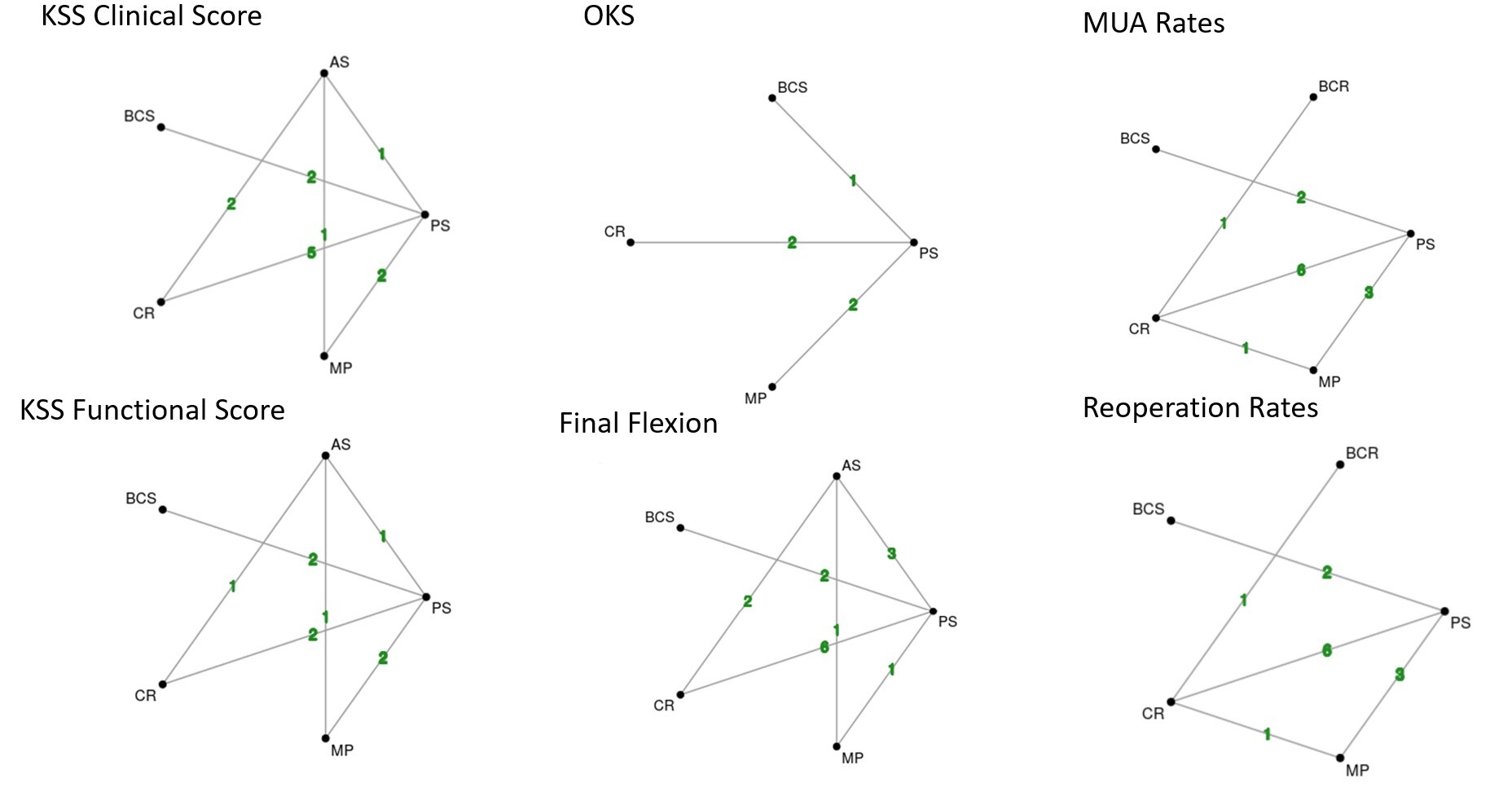
When trials reported comparable data from multiple pair-wise comparisons, we examined the data using MetaInsight43 network meta-analysis software. Network plots were created and when there was a connected network of evidence, further network analysis was performed using the random effects model. Cruciate retaining inserts were used as the reference treatment for network comparisons. Frequentist meta-analysis was performed and forest plots of the pooled effect estimates (mean difference), and their associated uncertainty (95% confidence intervals) were generated, for all interventions compared to the reference treatment. To adjust for multiple comparisons in the NMA, we utilized the Holm’s Sequential Bonferroni Procedure to adjust the p values.44 Differences were considered clinically significant if they exceeded Minimal Clinically Important Difference (MCID) values. MCID values used for KS clinical, KS functional and OKS were 9, 1045 and 546 respectively. Treatment rankings were plotted in a matrix displaying relative treatment effects with treatments ranked from best to worst along the leading diagonal. Agreement between treatment effect estimates obtained from direct (head-to-head) and indirect (indirect comparisons in network) evidence was examined in consistency tables using 95% confidence intervals and p values with p < 0.05 considered inconsistent.43 Funnel plots were created for each continuous variable using Meta-Essentials47 to assess publication bias utilizing the study standard error compared with the effect size using Cohen’s method.48
Results
Characteristics of included studies
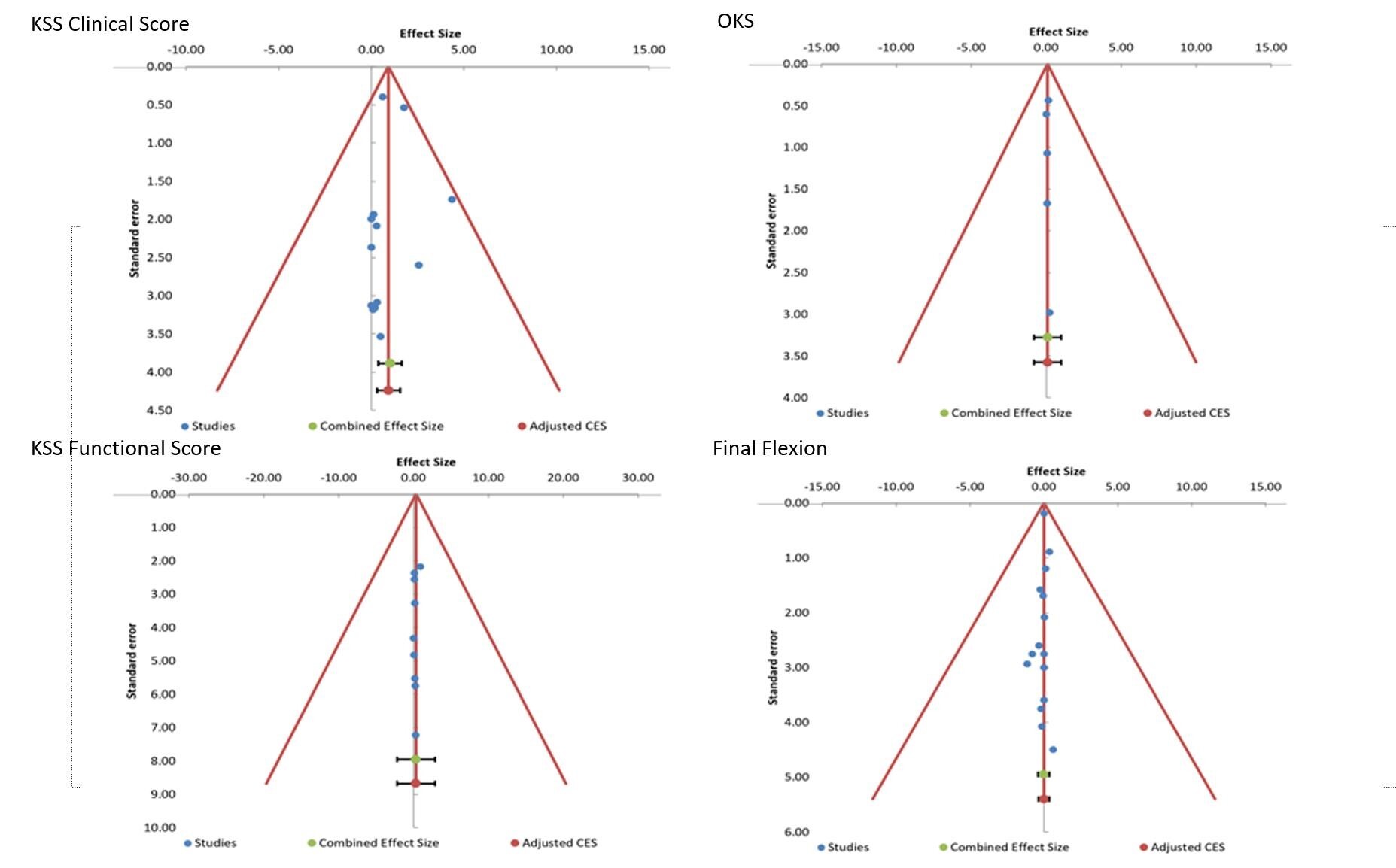
27 RCTs published between 2002 and 2021 with total of 2984 patients were included. 9 trials compared CR and PS,24,27,28,34–36,49–51 5 compared AS and PS,12,23,25,32,33 2 compared CR and AS,31,52 2 compared BCS and PS,21,22,31 1 compared AS and MP,29 4 compared PS and MP,26,37,53,54 1 compared CR and BR,18 3 compared multiple groups (CR, PS, MP,)55 (CR, PS, MP, BR),17 and (CR, PS, RP).56 All studies reported patient outcomes of greater than one year with the exception of the study by Batra et al37 which was 6 months and 21 out of 27 studies had a follow up of 2 years or more. Overall, the risk of bias was considered low. Four of the studies21,32,55,56 were funded by implant manufacturers and were therefore considered at high risk of “other” bias (Figure 3). There was enough data to perform NMA for Knee society clinical and function score (1989 version)57 Oxford knee score,58 maximum flexion > 1 year, MUA and reoperation rates (Figures 5 and 6). Inconsistency (Appendix 1) was low with p-values <0.05. Publication bias was noted to be low based on funnel plots (Figure 4). There was not enough uniform data to perform a NMA for Knee society score (2011 version), KOOS, WOMAC, Forgotten Joint Scores, and patient satisfaction.
Patient Reported Outcomes
14 studies reported KS clinical scores, 10 reported KS function scores and 7 reported OKS. There were no clinically or statistically significant differences in KS clinical, KS function scores and OKS for the six different inserts in the NMA (Figure 6).
Flexion
19 studies reported maximum flexion at >1 year follow-up. Mean differences in final flexion for different inserts compared to CR inserts were less than 4 degrees. Flexion was statistically more for PS inserts compared to CR inserts in the NMA (MD 3.2 degrees; CI 0.7 - 5.7) (Figure 6). These differences do not appear clinically significant. Flexion needed for walking, rising from a chair and descending stairs is 65, 70 and 100 respectively (reference). All of the inserts achieved more than 100-degree flexion and so were adequate for all these activities of daily living.
Manipulation Under Anesthesia and Reoperations
MUA rates were reported in 11 studies and reoperation rates in 19 studies. Our analysis found that odds of MUA compared to CR inserts were: BCR 7.93, BCS 1.11, PS 0.68 and MP 0.54. The odds of reoperation compared to CR inserts were: BCS 4.29, BCR 3.13, MP 2.54 and PS 1.35. Many of these differences appear clinically significant, however, they did not meet statistical significance after the Holm’s Sequential Bonferroni Procedure was applied to p-values to account for multiple comparisons. (Figure 6).
Patient Satisfaction
Given the heterogeneity of reported outcomes, we were not able to perform an NMA to evaluate patient satisfaction. Instead, we performed a systematic review of the available 27 studies. 4 studies evaluated KS satisfaction score. 3 showed no difference26,29,55 with one study showing improvement in satisfaction with MP vs PS inserts (32.6 vs 29.5 p 0.0).37 One study evaluated a functional satisfaction question through a survey where they reported 72% of PS inserts were satisfied versus 81% of MP inserts.53 Two studies evaluated VAS satisfaction scores with neither showing significance comparing BCS and PS (88 and 94 p 0.45)22 and CR and PS (19 vs 11 p > 0.05).56 Pritchett et al17 compared multiple inserts and found that patients preferred BR to CR (73.6% vs 18.7% p <0.001) and BR to PS (89.1% vs 4.3% p < 0.001). It showed no difference between BR and MP (48.4% vs. 48.4% p 1.0). It also showed MP inserts had higher satisfaction with MP vs PS (76.2% vs 9.5% p <0.001) and MP vs CR (76% vs 12% p < 0.001). Finally, there was no difference between CR and PS (43.8% vs 42.2% p 0.893). Overall, there is inadequate data to suggest superiority of one insert over the others.
Discussion
Different tibial inserts have been designed to encourage native knee kinematics, provide intrinsic knee stability and adequate satisfaction to all patients. Our analysis of 2984 patients with primary knee osteoarthritis addresses the knowledge gap in comparative efficacy and safety of different fixed bearing tibial inserts.
For patient reported outcomes, we did not find significant differences in 6 different fixed bearing tibial insert designs for KSS clinical score and Oxford knee score. Previous systematic reviews and meta-analysis of CR and PS designs59,60 have shown what?
For final knee ROM, we found that PS inserts studies had 3.2 degree higher final flexion compared to CR inserts. However, it is unlikely that this increase in flexion improves clinical outcomes. Our finding of higher flexion with PS compared to CR inserts is in agreement with multiple other studies.23,24,26,27 A meta-analysis of level IV studies has also shown deeper flexion with PS or BCS designs as compared to CR designs.61 Another meta-analysis and systematic review60 and a systematic review59 of RCTs comparing only PS and CR designs has also demonstrated improved flexion with PS inserts.
For MUA, our analysis showed high rates of MUA with BCR design and low rates of MUA with PS and MP designs compared to CR design. However, these clinically important differences did not meet statistical significance.
Odds of reoperation compared were lowest for CR inserts and highest for BCS (4.29) followed by BCR inserts (3.13), though these clinically important differences did not meet statistical significance. However, study follow up was at most 5 years for the RCTs evaluated. Registry data is available for multiple designs in our study. The MP design has an acceptable 7.4% revision rate at 10 years in the Australian registry and 9.8% at 10 years in the Dutch registry.62 BR knees have reported >90% survivorship free of revision at 10 years for first generation designs,63 whereas one AS design has reported >95% revision-free survivorship at 7 years in a large series.64 Finally, the BCS implant shows comparable revision rates as compared to PS knees at 5 years in single RCTs.65
Recent literature has been heterogeneous in terms of showing whether particular implants improve satisfaction.64,66,67 Though satisfaction is important for patient outcomes following total knee arthroplasty, most of the studies reviewed were powered and designed to evaluate patient reported outcome scores rather than satisfaction. Two studies did show that MP inserts may have improved satisfaction17,37 and one showed that BR inserts may have improved satisfaction.17 However, given the heterogeneity of the data available and the study designs evaluated, we cannot make new meaningful conclusions based on any improvement in patient satisfaction when comparing all six inserts.
Our study has several limitations. First, our results apply only to TKA for primary osteoarthritis and not for other TKA indications such as inflammatory or traumatic arthropathy. Inserts of same type from different manufacturers have subtle design differences which may affect outcomes. This heterogeneity combined with differences in surgical technique may have affected comparisons reported in this analysis. The BR and BCS inserts had fewer studies than the PS or CR inserts which may have introduced type II error. We were also unable to report a meta-analysis regarding satisfaction as the scoring outcomes were too heterogenous. Most trials included had two-year follow-up, which would be considered short-term for TKA. Despite these limitations, this is the first study to date which reports comparisons among six separate TKA polyethylene designs that are designed to produce differing kinematics.
In conclusion, our network metanalysis shows no clinically significant differences in patient reported outcomes in fixed bearing inserts. PS inserts had more knee flexion at >1 year follow-up compared to CR inserts, but the 3-degree difference in flexion does not appear clinically significant. There were clinically important differences in manipulation and reoperation rates of different inserts with high rates of manipulation and reoperations with bi-cruciate retaining and bi-cruciate substituting designs, but these did not meet statistical significance. We advise caution with BCR and BCS designs and feel that inserts should be chosen based upon clinical situation rather than improvements in PROMs, satisfaction, or avoiding complications.
Funding/Support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.