Introduction
Periprosthetic joint infection (PJI) is one of the most feared and devastating complications after total knee arthroplasty (TKA).1 The Musculoskeletal Infection Society (MSIS) has recommended criteria to better define and diagnose PJI and these criteria underwent further modification during the 2018 International Consensus Meeting (ICM) on PJI.2 The diagnosis of early postoperative PJI still remains a major challenge and the quick initiation of therapy represents the key to the success of the debridement, antibiotics and implant retention (DAIR) followed by antibiotic therapy. According to the definition of PJI, in the absence of major criteria (i.e., communicating sinus tract or two positive cultures) serologic results are the bedrock of diagnosis.3 Indeed, minor criteria include elevated serum C-reactive protein (CRP) (> 10 mg/L), D-dimer (> 860 ng/mL), and erythrocyte sedimentation rate (ESR) (>30 mm/h).
CRP is an acute-phase protein produced in the hepatocytes for inflammation, trauma, malignancy or infection and lends itself as an inflammatory biomarker for the detection of a potential infection in orthopedic surgery.4 Although CRP can be elevated for as long as 3 months after TKA even in the absence of infection,5 its levels usually peak at day 2 or 3 postoperatively and diminish abruptly if there are no postoperative complications.6 CRP only has limited sensitivity and specificity7,8; notably, the sensitivity of serum CRP in detecting PJI has been reported closer to 80%,9,10 suggesting that the CRP test may fail to detect infection, especially in cases of indolent organisms. Therefore, understanding the limitations of the CRP test is of paramount importance.
We undertook this prospective study in patients undergoing primary TKA for osteoarthritis (OA): (1) to define the temporal pattern of CRP over a 4-week period in non-infected TKA, and (2) to test the association between patients’ baseline characteristics and pre- and postoperative CRP levels.
Materials and Methods
A prospective data collection was undertaken on consecutive patients that underwent primary TKA for OA at our institution between July 2019 and January 2020. Hospital board approval was obtained prior to study commencement and informed consent for study participation was obtained from all study participants. The exclusion criteria were: (1) TKA in patients who had undergone previous knee surgery, (2) revision TKA, (3) TKA performed for any diagnosis other than primary OA, (4) any known rheumatic diseases, inflammatory arthritis, or autoimmune disorders, (5) history of cancer, (6) history of recent surgical procedures, (7) history of medium to long-term steroid intake,11 and (8) concomitant neurological,12 vascular, and orthopedic diseases of the lower limbs. Data gathered included the sex and age of patients, body mass index (BMI), diabetes mellitus (DM), smoke habits, hypertension, heart disease, chronic renal failure, and early postoperative complications (i.e., when occurred less than 30 days after surgery). CRP level (reference range values, 0-5 mg/L) was evaluated the day before surgery (i.e., at hospitalization), at the 4th day after surgery (i.e., the day before the usual discharge), and at the 30th day after surgery (i.e., the first radiological postoperative evaluation). Patient’s functional and radiological evaluation was scheduled 3, 6, and 12 months after surgery.
Surgical technique
All surgical procedures were performed by two surgeons (GG and OG) with high and comparable levels of experience in knee arthroplasty. Deep vein thrombosis (DVT) prophylaxis was carried out by administration of low-molecular-weight heparin,13,14 intravenous antibiotic prophylaxis was administered preoperatively and for 24 hours after surgery using a first-generation cephalosporin.15 Either spinal or epidural anesthesia was performed for all procedures. A well-padded high-thigh tourniquet (Zimmer-Biomet, Warsaw, Indiana, USA) was placed on the operative leg and all patients were placed supine on the operating table. A standard medial parapatellar approach and a cemented, posterior-stabilized Zimmer Persona® knee implant system (Zimmer-Biomet, Warsaw, Indiana, USA) were used in all patients. A closed-suction drain was applied and removed after 24 hours.16
Postoperatively, patients were given intravenous acetaminophen, nonsteroidal anti-inflammatory drugs, and oral opioid for pain relief.17 All patients were mobilized on the day of the surgical procedure and received daily inpatient physical therapy until the time of hospital discharge. Afterwards, all patients were designated for outpatient physical therapy until the first clinical and radiological follow-up at 30 days postoperatively.18
Statistical analysis
All data were measured, collected, and reported to one-decimal accuracy. The mean, standard deviation, and range were noted for the continuous variables with normal distribution; the median and interquartile range (IQR) for the remnant variables and counts for the categorical variables were recorded, respectively. The distribution of the numeric samples was assessed by Shapiro-Wilk normality test. Based on this preliminary analysis, parametric tests were indicated and used in case of normality; otherwise, non-parametric ones were considered.
A non-parametric Friedman test was carried out to compare the CRP values reported preoperatively, 4 days postoperatively, and 30 days after surgery; Dunn pairwise tests with Bonferroni correction were subsequently applied, in order to analyze differences between pairs if the main test was significant.
Pearson Phi’s correlations were investigated with the aim of looking for possible association between CRP over the reference range values (i.e., > 5 mg/L) at the three serum measurements. Patients’ baseline characteristics were tested as predictors. Binary logistic regression analysis was performed to investigate possible predictors of the categorical-dependent variables of abnormal CRP values at 30 days after surgery. Sample size was calculated with the aim to achieve a minimum β-value higher than 0.8 statistical power (α = 0.05) for CRP three-step values analysis; 37 cases were calculated as an adequate number, and since the possibility of drop-out for any reason, a higher number of patients were included in the study (i.e., 41 patients). Patients who developed PJI within 30 days after surgery were excluded from the statistical analysis.
IBM SPSS Statistics software (version 21.0.0.1, IBM Corp., Armonk, NY, USA)19,20 and G*Power (version 3.1.9.2, Institut für Experimentelle Psychologie, Heinrich Heine Universität, Düsseldorf, Germany) were used for database construction and statistical analysis. A p-value of less than 0.05 was considered significant.
Results
The baseline characteristics of the study population are summarized in Table 1. Forty-two consecutive patients fulfilling the inclusion criteria underwent TKA during the study period. No cases of drop-out were recorded. One patient that developed an early PJI was excluded from the analysis of data. The patient showed signs and symptoms of PJI two weeks after surgery when the CRP levels measured 265 mg/L and methicillin susceptible Staphylococcus aureus was isolated from the aspirated joint fluid. The patient was successfully treated with DAIR. As a result, a total of 41 cases were evaluated and no complications or reoperations were reported one year after surgery.
CRP evaluation
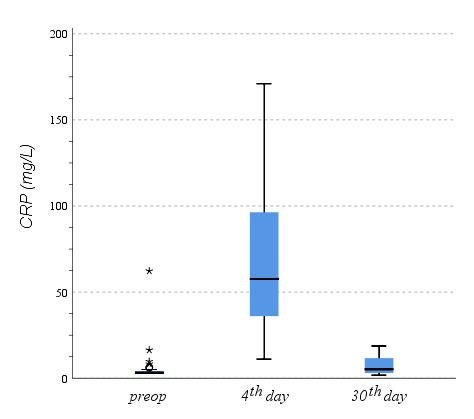
Figure 1 shows differences in pre- and postoperative CRP values. Preoperatively, the CRP median value was 3.2 mg/L (IQR, 3.2-4.2); 4 and 30 days after surgery, it measured 57.6 mg/L (IQR, 36.1-96.4) and 5.3 mg/L (IQR, 3.0-11.8), respectively. At the non-parametric Friedman test, there was a statistically significant difference in the distribution of CRP levels among values reported at the three evaluations (i.e., preoperatively, 4, and 30 days after surgery) for χ2(2)=66.7 and p<0.001. Dunn tests with Bonferroni correction were carried out, and there were significant differences between the CRP values preoperatively and 4 days after surgery (p<0.001) and between CPR levels 4 and 30 days after surgery (p<0.001). No differences were found between preoperative CPR values and those recorded 30 days postoperatively (p=0.181).
Correlation and regression analysis
As showed in Table 2, higher preoperative CRP values were associated to heart disease and chronic renal failure (r=0.329, p=0.036, and r=0.437, p=0.004, respectively), and trends toward statistical significance were found between higher preoperative CRP values and DM and hypertension (r=0.274, p=0.083, and r=0.300, p=0.057, respectively). Four days after surgery, higher CRP values were associated to older patients (r=0.311, p=0.048) and showed a trend toward significance in patients with chronic renal failure (r=0.264, p=0.096). No correlations were found between baseline characteristics of patients and the CRP values or the CRP values over the reference range, 30 days postoperatively.
Discussion
The most important findings in the present study are that there was a significant increase between preoperative CRP values and those recorded 4 days after surgery. Moreover, CRP levels significantly decreased between 4 and 30 days after surgery. No differences were found between median CRP values preoperatively and 30 days after surgery. Higher preoperative CRP values were associated to heart disease and chronic renal failure. Four days after surgery, higher CRP values were associated to older patients and showed a trend toward significance in patients with chronic renal failure.
PJI is still one of the most challenging and devastating complication after TKA,21 and it represents the most common cause of failure in TKA, representing 20.4% of all knee revisions.22 The economic burden of treating this complication is staggering, costing over $75,000 per patient, as well as prolonged inpatient stays and higher morbidity and mortality. CRP and ESR rates are first-line tests in suspected PJI, because of their convenience and short waiting times. They are strongly recommended in the 2010 guidelines of the American Association of Orthopaedic Surgeons (AAOS).23,24 Elevated ESR and/or CRP levels were included as a diagnostic criterion in the 2011 definition of PJI by the MSIS,25 and the 2013 guidelines of the Infectious Diseases Society of America (IDSA).26
The diagnosis of PJI in the early postoperative period is challenging especially when the clinical presentation is nonspecific. One of the major issues is that the values for inflammatory serum markers such as CRP may be elevated for a long period as a result of surgical trauma, rendering these tests less valuable for the diagnosis of early PJI. High early postoperative CRP levels can be hard to interpret shortly in the days and weeks immediately after arthroplasty, because CRP can be elevated for as long as 3 months even in the absence of infection.27 We reported that the median value of CRP levels was within the normal ranges preoperatively, and that there were no differences between CRP values before the operation and 30 days after surgery. Kim et al.28 constructed ROC curves to determine the optimal cutoff values for laboratory parameters such as synovial white blood cell (WBC) count, percentage of polymorphonuclear (PMN) cells, ESR, and CRP levels for diagnosing early postoperative infection after TKA. Each parameter was studied to determine its sensitivity, specificity, and positive and negative predictive values (PPV and NPV) in diagnosing acute PJI. The authors reported that there were 2 optimal cutoff values for CRP levels. Interestingly, the CRP level >34.9 mg/L had the best sensitivity (100%) and specificity (90.3%), whereas the CRP level >74.5 mg/L had the best PPV (100%) and NPV (99.2%). Notably, the patient that developed an early PJI and who was therefore excluded from the current study, showed a CRP value of 265 mg/L two weeks after surgery.
CRP levels are influenced by age, sex, smoking, and BMI in the general population and in people with certain comorbidities such as rheumatoid arthritis and chronic renal failure. Thus, interpreting elevated CRP levels in the first 30 days after primary TKA requires an understanding of how this variable is influenced by patient characteristics. Current recommendations for the use of CRP in diagnosing PJI may not consider the influence of preoperative patient characteristics on CRP levels. We demonstrated that higher preoperative CRP values were associated to heart disease and chronic renal failure. We next found that four days after surgery, higher CRP values were associated to older patients and showed a trend toward significance in patients with chronic renal failure. Given the association between elevated CRP levels and patient characteristics found in this study, physicians should be cautious about interpreting post-operative elevated CRP levels in older patients and in patients suffering from chronic renal failure in the first 30 days after primary TKA and take preoperative values into account to avoid false positive PJI diagnoses.
Several limitations can be found in the present study. The most important limitation is the small sample size. However, a power analysis conducted prior to the main analyses showed that this sample had sufficient power to conduct our tests. A larger sample size would be needed in order to detect correlations or predictors for CRP values over the reference range at 30 days postoperatively at the correlation and logistic regression analysis. However, these were secondary outcomes. Finally, we have only evaluated one serum inflammatory marker and we have not considered other serum parameters such as IL-6 and ESR that could be equally useful.
Conclusions
Thirty days after primary non-infected TKA, CRP levels are comparable to preoperative values. Use of standalone CRP value as an indicator of postoperative joint infection should be used with caution in the diagnosis of early PJI since it is not an absolute value, but the relative trend should be considered. Older age and comorbidities should be carefully evaluated using postoperative CRP as diagnostic marker for the early detection of infection.