Introduction
Acute knee dislocation is a rare orthopedic injury with an incidence of <0.02% annually.1 Knee dislocations predominantly occur in a younger patient population, with a male-to-female ratio of 4:1.1 Although knee dislocations traditionally are thought to result from high-energy mechanisms (e.g. fall from a height, crush injury, motor vehicle collision [MVC], and pedestrian versus motor vehicle), they also can be caused by low-energy mechanisms (e.g. misstep during routine walking, martial arts kicks, and trampoline fall).2 A high index of suspicion combined with a careful neurovascular examination is imperative in every patient presenting to the emergency department (ED) with a knee injury. Since the popliteal neurovascular bundle is anchored at both the femur and the tibia, any type of dislocation or injury to the knee could compromise this structure.3,4 The authors discuss a case involving a vascular injury sustained from a mechanical fall at home causing compartment syndrome.
Case Presentation
An 18-year-old male with a past medical history significant for Down’s syndrome, morbid obesity, and dilated cardiomyopathy status septal myomectomy on 75mg metoprolol daily, presented to the ED via Emergency Medical Services (EMS) after a mechanical fall at home. The patient was walking outside when he tripped and landed with full weight on his right knee. (Figure 1) He was unable to brace himself. He denied a loss of consciousness but reported right knee pain and inability to ambulate. EMS noted a right lower extremity deformity and pedal pulses were present. Upon arrival to the ED, the patient was noted to have a mottled, cool limb with absent pedal pulses. (Figure 2) The patient was immediately upgraded to a Level 1 trauma alert and taken into the trauma bay. He was placed on a cardiac monitor and noted to have sinus tachycardia sustained in the 160s. On examination, he was diaphoretic but alert and oriented. He could not range the right knee, ankle, or toes. The popliteal fossa and posterior aspect of the right lower extremity was indurated and tender to palpation.
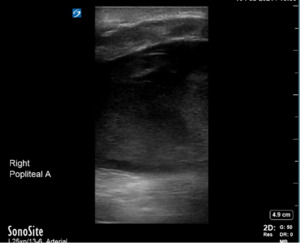
Bedside ultrasonography confirmed a large hematoma with heterogeneity in the popliteal fossa extending superiorly into the distal femur and inferiorly into the calf. While the femoral artery was found without anomalies on ultrasound, no popliteal artery could be found in the popliteal hematoma (Figures 3 and 4). This was concerning for active bleeding in the popliteal fossa from damage to the artery.
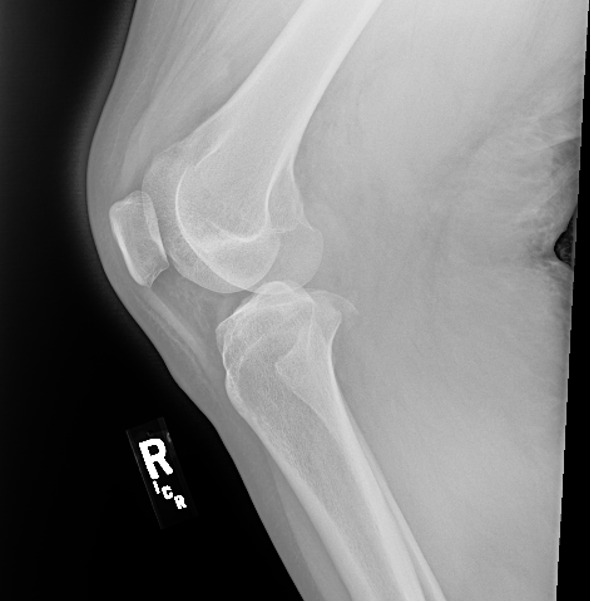
A quick portable knee x-ray demonstrated a right medial tibial plateau fracture with a displaced fragment measuring approximately 1.2 x 1.6 cm on the frontal view. (Figures 5 and 6) It was determined that the patient likely had dislocated his knee, resulting in significant vascular injury to the popliteal artery. Vascular surgery and orthopedics were consulted, and the patient was taken immediately to the operating room for revascularization and exploration.
In the operating room, the patient was found to have a right posterior knee dislocation, a right tibial plateau fracture, and a right proximal popliteal artery transaction resulting in a large hematoma. This hematoma, in turn, was contributing to compartment syndrome. The patient underwent a right proximal popliteal artery repair via end-to-end femoropopliteal bypass using a contralateral reverse saphenous vein graft harvested from the left thigh. He had an external fixator (ex-fix) placed by orthopedics and was taken to the Intensive Care Unit (ICU) for routine postoperative care and frequent neurovascular checks. (Figure 7) The patient was monitored in the hospital for several days and noted to be recovering well, including a return of range of motion to the right toes and ankle. Orthopedics elected not to pin the right medial tibial plateau fragment, given the patient was non-weight bearing for 3 months. He did require one unit of blood postoperatively. He was subsequently discharged on post-op day 10 to inpatient rehab with the ex-fix (definitive care) still in place as well as a right lower extremity multipodus boot to hold his foot in a neutral position following a successful hospital course. Fifteen weeks later, the ex-fix was evaluated for removal. However, the patient tested COVID-19 positive at that time, so removal was delayed until recovery.
Discussion
Down syndrome, also known as Trisomy 21, is a genetic condition that predisposes individuals to multiple orthopedic pathologies. These conditions include but are not limited to generalized ligamentous laxity, hypotonia, short stature, instability or subluxation of the atlantoaxial joint, delayed motor milestones, femoral head epiphysiodesis, dislocation or subluxation of the hips, patellofemoral instability, dislocation or subluxation of the patella, scoliosis, spondylolisthesis, pes planus, hallux valgus, metatarsus primus varus, and SCFE.5,6 Specifically, patellofemoral instability (PFI), the most common knee abnormality,7 predisposes patients with Down Syndrome to knee injuries. Those with PFI are more likely to have valgus deformities, medial tibial plateau depression, and lateral translation of the tibia,(6) all of which can predispose to knee dislocations such as in our patient.
Furthermore, young individuals with Down Syndrome often have hypotonia and delays in motor development, especially of the lower extremities, resulting in impaired physical health, walking, balance, and activities of daily living.8 Oftentimes these individuals need physical therapy to improve their motor strength.8,9 Unfortunately, our patient was not undergoing physical therapy but also had never had difficulty walking before. This muscle weakness also predisposes patients with Down Syndrome to obesity.
There is increasing evidence suggesting that morbid obesity (BMI > 40) also predisposes to and increases the risk for knee dislocation.10 Specifically, this population had an increased risk of dislocation from low-velocity mechanisms, such as those seen with activities of daily living: stepping off a curb, stepping off a stair, stepping down from a truck, or a ground-level fall.11 Average BMI in this case series was 48, and our patient’s BMI was 41.9, making this risk applicable to our patient. Subsequently, all of these factors likely contributed to our patient sustaining a significant knee dislocation and vascular injury following an uncomplicated mechanical ground-level fall.
Popliteal artery transaction is a condition that can lead to limb ischemia, necrosis, and amputation. Delay in presentation and/or delay in revascularization can increase the likelihood of subsequent permanent disability and/or amputation.3 Despite the closed reduction of a proximal tibial fracture or a knee dislocation, vascular occlusion may persist. Frequently, the joint does spontaneously reduce, and it can be difficult to differentiate between swelling from the tendon disruption and subsequent hemarthrosis versus from a vascular injury. Rates of popliteal artery injury in knee dislocations can reach 32%.3,12 Rapid diagnosis and intervention can decrease the period of limb ischemia distally, which in turn decreases the need for palliative amputation. The overall rate of civilian amputations secondary to a popliteal artery injury approaches 30%, and in popliteal injuries unaddressed for 8 hours or more, the amputation rate is 85%.3
Popliteal artery injury may be diagnosed using doppler ultrasound, however, the gold standard is angiography. Nevertheless, given the time-sensitive nature of arterial injury (i.e. transection, dissection, impingement, or shearing), ultrasound has been increasingly used as an adjunct to physical examination.3 Any delay in treatment can be catastrophic and may lead to serious complications such as permanent sensory and motor deficits, contractures, infection, and ultimately limb amputation. If clinical signs and symptoms of compartment syndrome are present such as pain with passive movement, paresthesias, pallor, paralysis, poikilothermia, and/or pulselessness, a fasciotomy should be performed immediately, as exsanguination can lead to compartment syndrome such as in our case.12 Preventive fasciotomy may be considered in cases where limb ischemia is greater than 5 hours and there is a delay in treatment in order to avoid a reperfusion injury.
Conclusion
This case illustrates known complications associated with knee dislocations: vascular injury and compartment syndrome as well as the high suspicion needed in certain patient populations. It highlights the importance of rapid diagnosis, a complete physical exam, and the need to involve consultants in a timely fashion. Every clinician should maintain a high index of suspicion for vascular injury following trauma to the knee, regardless of the mechanism.