Introduction
Acromioclavicular septic arthritis is a rare and destructive process that may be difficult to diagnose. The causes of acute joint pain are vast. They include osteoarthritis, rheumatoid arthritis, other immune deposition diseases, gout, pseudogout, seronegative spondyloarthropathies, reactive arthritis, as well as bacterial and viral infections.1 Once there is suspicion of septic arthritis based on symptoms which may include fever, warmth, erythema and limited range of motion, the precise diagnosis of acromioclavicular septic arthritis is challenging due to its similarities with the much more common presentation of glenohumeral septic arthritis.2 In the emergency department, the initial diagnosis is largely clinical, typically later supported by diagnostics. Risk factors include but are not limited to immunocompromised states such as autoimmune conditions, diabetes, HIV, as well as recent surgery, instrumentation, endocarditis or other seeding type infections, prior joint disease, and intravenous drug use.3 The gold standard for diagnosis in native joints is arthrocentesis with a synovial fluid white blood cell count usually greater than 50,000 per mm3 and a lower threshold for those with prosthesis. Nearly 80% of nongonococcal infections identified the causative organism as staphylococcus aureus, however, group B streptococcus is most common in diabetic patients as in our case.3,4 Multiple imaging modalities including plain film radiography, computed tomography, magnetic resonance imaging, as well as ultrasound may be helpful, but offer their own unique limitations. Lab studies are supportive but not diagnostic and typically include a white blood cell count over 10k, as well as an elevated sedimentation rate. C-reactive protein is helpful in assessing the efficacy of therapy if trended appropriately.3 Treatment should be started empirically in the emergency department to cover both gram-positive and gram-negative organisms with vancomycin and ceftriaxone respectively. Special populations or considerations may require coverage for pseudomonas or gram-negative rods if there is the likelihood of these being the causative organism. Ideally, antibiotics should be tailored once fluid analysis and culture are completed. Misdiagnosis or delayed treatment has significant mortality and morbidity as cartilage damage can occur within eight hours of infection.3 Intravenous antibiotics, arthrocentesis, and often surgical exploration are typically curative.
Case Presentation
A 51-year-old undomiciled male with a past medical history of diabetes mellitus, schizophrenia, and substance abuse presented to the emergency department for evaluation of right shoulder pain. He noted the pain began suddenly three days prior to presentation and was associated with weakness and decreased range of motion secondary to pain. He denied any trauma or previous shoulder surgeries. He reported associated nausea and anorexia coupled with the onset of his symptoms but denies any other systemic symptoms.
Physical examination revealed erythema and edema localized to the right trapezius, posterior deltoid, and over the shoulder. The patient denied any recent skin tears, lacerations, or prior similar symptoms. He admitted to using cocaine and marijuana but denied any current intravenous drug use. Active range of motion to the right shoulder was significantly reduced as well as passive range of motion was limited but to a lesser degree. He had strong radial pulses, sensation intact, and preserved function of radial, ulnar and median nerves. The patient was tachycardic with a heart rate of 110 beats per minute and febrile at 38.3 degrees Celsius on arrival. The patient met sepsis criteria at this time given likely cellulitis as the source and possible septic arthritis. Vancomycin and ceftriaxone IV was ordered along with blood cultures and lactic acid. Sedimentation rate (ESR) and C-reactive Protein (CRP) were added due to concern for osteomyelitis. The patient had an elevated white blood cell count of 13.2k as well as elevated ESR and CRP. Lactic acid was within range at 1.6mmol/L. Plain film shoulder x-rays revealed no acute fracture and noted mild acromioclavicular arthropathy. The decision was made to obtain computed tomography (CT) imaging with the contrast of the shoulder to better characterize the cellulitis and to investigate if the infection had spread to deeper structures. CT revealed fat stranding consistent with cellulitis but no focal fluid collection or aggressive bone lesions. The patient was admitted for further MRI imaging, continued IV antibiotics, as well as orthopedic and infectious disease evaluation.
On the second day of admission, two sets of blood cultures were positive for streptococcus agalactiae group B. Patient was no longer febrile or tachycardic after emergency department treatment. MRI without contrast revealed extensive soft-tissue edema, and mild subdeltoid bursitis, however, no signs of osteomyelitis. Orthopedics consulted interventional radiology for possible arthrocentesis. This was deferred as there was no obvious fluid collection upon review of imaging. He underwent transthoracic echocardiography to evaluate for endocarditis which was negative for any significant findings or vegetations. The decision was made to continue antibiotics and serial exams. It was also noted that the patient was negative for HIV as well as gonorrhea and chlamydia infection.
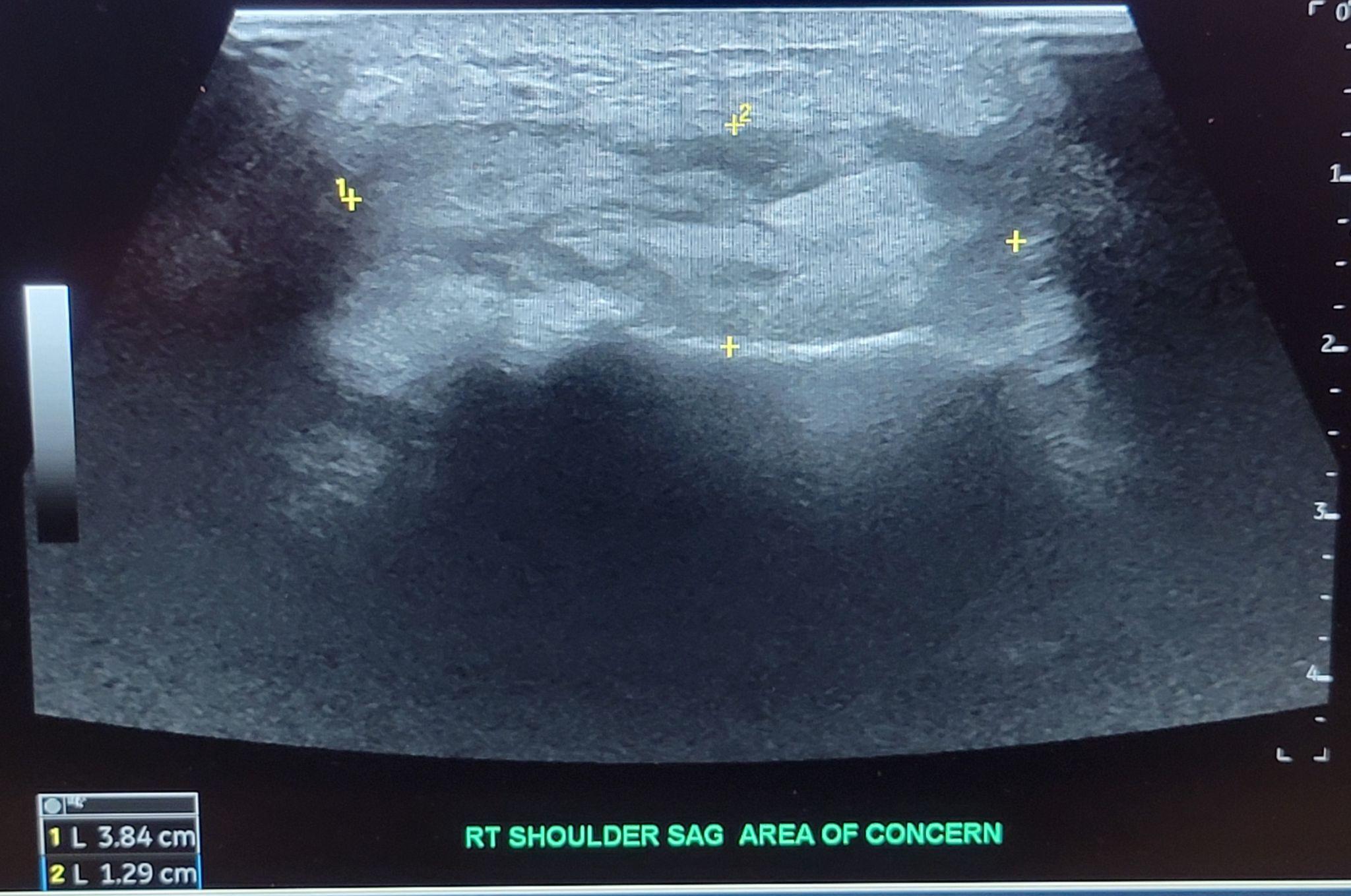
Infectious disease became a concern as the patient continued to have an upward trending white blood cell count and continued pain despite antibiotics on the fourth day. The recommendation for STAT MRI as well as orthopedic re-evaluation for possible surgical exploration was given. The next day, orthopedics did not wish to explore surgically as previous imaging did not reveal any signs of necrotizing disease or obvious fluid collection. The repeat MRI with contrast resulted after the initial orthopedic evaluation was concerning for septic arthritis as well as osteomyelitis of the acromion and distal clavicle [Figure 1]. Additional ultrasound imaging was ordered and confirmed a 1.3cm x 2cm area of fluid collection [Figure 2]. Interventional radiology was again consulted but was unable to perform arthrocentesis as there was no clear uncontaminated path due to overlying cellulitis. The decision was made for incision and drainage for the next morning [Figure 3].
The operative report noted purulent drainage from the fluid collection which was cultured and found to contain the same streptococcus agalactiae group B as the previous blood culture. During the exploration, a tract was noted from this fluid collection into the distal end of the clavicle and subsequent excision of this distal tip. The wound was closed loosely and a wound vacuum device was applied. The decision was made to continue IV antibiotics for a total of six weeks given the penetration of infection into the bone. The patient remained afebrile and was discharged home on the eleventh day of his hospital course.
The patient returned to the emergency department three days later due to social barriers to receiving IV antibiotics in the outpatient setting. The patient white blood cell count had increased from discharge, however, he remained afebrile and noted improved pain. Case management was made aware and the decision to remain admitted for IV antibiotics was determined to be the optimal option as the patient did not qualify for a skilled nursing facility, had social security as sole income, and did not have a definitive address for home health care as he was homeless. The patient was discharged home on the 34th day of this total hospital course with oral linezolid which was free of charge with his insurance and he continued to obtain outpatient orthopedic follow-up.
Discussion
As presented in this case, the diagnosis of septic arthritis and subsequent osteomyelitis is difficult for a multitude of reasons. Emergency physicians must consider not only large joint manifestations but also small joint synovial infections. The case also demonstrates the constant need for re-evaluation and persistence by all members of a multidisciplinary team to ensure accurate diagnosis and ultimately curative treatment. The initial presentation of cellulitis, fever, tachycardia and elevated biomarkers along with white blood cell count allowed for prompt initiation of empiric antibiotics and admission for further consultation with appropriate consultants. In the earlier stages of this condition, the indication for aggressive treatment and surgical exploration may not be as apparent. According to a 2020 literature review, less than 28 documented cases of acromioclavicular septic arthritis were found.5 It is also notable that imaging, serum examinations, and biomarkers are not specific and must be in conjunction with clinical suspicion based on physical exam findings. Carpenter et al6 noted that overlying cellulitis and recent surgery were the only findings in the history and physical exam that altered the probability of nongonococcal septic arthritis. The patient had extensive cellulitis overlying his trapezius and shoulder girdle along with positive blood cultures which were only known later to the inpatient team. It is reasonable to assume the infection was spread as is common via hematological spread in the absence of trauma or prior instrumentation of the joint. The cause for the cellulitis, however, was not typical given the location and lack of apparent breakdown of the skin or other vulnerable areas where this may have originated.
The patient was examined with a multitude of imaging modalities during his course. Initial x-ray radiographs along with CT imaging with contrast in the emergency department did not reveal any fluid collection or signs of osteomyelitis. The initial MRI was performed without contrast and also did not demonstrate a drainable fluid collection. Only after six days of admission and re-imaging of the shoulder with contrast-enhanced MRI was their evidence of septic arthritis which was even more accurately characterized by ultrasound. It cannot be known if a bedside ultrasound in the emergency department would have identified the fluid collection as it is unknown whether it had manifested at the time of examination given the negative results of both CT and MRI imaging, however, is an area that may warrant further exploration.7 Interventional radiology was consulted initially and was unable to perform the arthrocentesis as during their review there was not a drainable collection. Fortunately for our patient, the interventional radiologist was unable to find an uncontaminated path for arthrocentesis secondary to overlying cellulitis. The availability, improved accuracy, and safety of interventional radiology performing this procedure have made it a preferred approach, however, this may lead to delays in diagnostics and treatment.8 Without surgical exploration, the tract between the purulent fluid collection and clavicle would have likely not been identified and led to a prolonged, difficult course and possibly deadly outcome.
Septic arthritis with associated osteomyelitis requires an extended course of intravenous antibiotics along with close follow-up. As in the case presented, many patients may have barriers or other social determinants of healthcare that will need to be overcome in order to ensure a good outcome. Case management is a critical aspect of this type of presentation for these reasons. Due to his social situation combined with his psychiatric and other medical conditions, the appropriate disposition was further admission to ensure not only antibiotic administration but counseling and resources to better manage his diabetes as this is a risk factor for both his initial infection and possible subsequent similar infections. This case highlights the necessity of advocating for our patients and seeking out affordable and executable plans of treatment as a top priority.
Conclusion
Acromioclavicular septic arthritis is an unusual condition that requires consideration, careful history taking, and physical examination to ensure prompt diagnosis and treatment. Imaging and laboratory testing are helpful in aiding diagnosis but are not required for the initiation of empiric treatment. Alternate causes of shoulder pain should be considered and explored to precisely diagnose this and other concomitant conditions which may require additional treatment. Serial examinations along with trending of white blood cell count, biomarkers, and imaging may be necessary to determine eligibility for surgical exploration. Choosing appropriate imaging modalities may be challenging given their unique limitations. As with any rare diagnosis, it is critical to include the differential diagnoses in order to evaluate thoroughly. Case management, outpatient follow-up, and patient advocacy continue to be of the highest importance to decrease morbidity and mortality relating to treatment noncompliance and failure.
Disclaimer
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.



_and_post_procedure_(right).png)

_and_post_procedure_(right).png)