1. INTRODUCTION
Total hip arthroplasty (THA) is utilized for a variety of diagnoses including osteoarthritis, rheumatoid arthritis, proximal femoral and acetabular fractures in the elderly, and fracture arthropathy. Historically, the posterior approach has been advocated. In recent years, there has been conversation around newer approaches.1–5 The term minimally invasive total hip arthroplasty6 has emerged as a blanket term for new surgical approaches and the use of smaller incisions. The direct anterior approach3 and the piriformis sparing approach4 have the potential to reduce pain scores, improve recovery, and improve hip disability and osteoarthritis outcome scores (HOOS) as compared to the posterior approach.3
Regardless of the pathology treated and the approach taken, THA is generally a successful procedure.7–11 A recent systematic review and meta-analysis demonstrated that THA has improved clinical scores, decreased mortality rate, and dislocation rate when compared to hemiarthroplasty in the treatment of femoral neck fractures in the elderly.9 A recent retrospective case series reported significantly improved pain, mobility, and quality of life in young patients with end-stage juvenile osteoarthritis that underwent THA after the failure of due conservative attempts.8 THA does exist as a salvage option for the failure of arthroscopic cam/pincer resection, failure of periacetabular osteotomies for adult hip dysplasia, and other causes of secondary arthropathy.7 Favorable outcomes after hip dislocations have also been shown demonstrating the versatility of the operation.10
Liposomal bupivacaine (LB) has shown great promise within various fields of surgery. To date, these include colorectal surgery,12 cardiothoracic surgery,13 and orthopedic surgery.14 Within orthopedic surgery, LB has demonstrated great potential as an adjuvant to traditional pain control measures in rotator cuff surgery,15–17 ACL reconstructions,18 and total knee arthroplasty.19 As a suspended, long-duration non-opioid anesthetic, LB has the potential to decrease dependencies on opioid use in the post-operative period following THA.15–19 The purpose of this scoping review is to summarize the current literature regarding the opioid epidemic as it pertains to THA and to highlight the role that LB may play in decreasing narcotic use after total hip arthroplasty.
2. MATERIAL AND METHODS
2.1. General
This was an IRB-exempt scoping review. The scoping review checklist available at the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews Checklist (RPSIMA-ScR) was followed strictly. The international prospective register of systematic reviews (PROSPERO) was contacted regarding our intention for this article and advised that scoping views do not require registration with PROSPERO.
2.2. Search Strategy
The literature search was performed using Medical Search Headings (MeSH) in Mendeley version 1.19.8. Articles published between January 1975 to December 2021 were Search fields were varied until no new articles were collected at which point the search was considered exhaustive.
2.3. Study Screening
All articles were screened by title and abstract. An initial decision to include a given article was made based on the relevance of the information within the abstract as determined by our inclusion/exclusion criteria (Table 1). This constructed a list of preliminarily included articles. These preliminarily included articles underwent classification as ‘Tier 1’, ‘Tier 2’, or ‘Tier 3’ articles. Tier 1 articles were defined as primary studies that directly pertained to the use of liposomal bupivacaine in total hip arthroplasty. Tier 2 articles were relevant articles that summarized the current state of pain control after total hip arthroplasty, the opioid epidemic as it pertains to hip arthroplasty, or the current standard of care regarding the use of other local anesthetics in total hip arthroplasty. Tier 3 articles were those that included relevant search terms but did not meet the above two criteria.
2.4. Study Selection
Articles from Tier 1 and Tier 2 then underwent a full-text screening process. This resulted in the elimination of many articles until 9 articles in Tier 1 and 21 articles in Tier 2. The results of the articles from Tier 2 are described qualitatively in Sections 3.1-3.4 and Section 3.6. The results of the Tier 1 articles are discussed in Section 3.5. Any question regarding the inclusion of an article was discussed by all authors until an agreement was reached. The bibliographies of these articles were also hand-searched to identify any missing articles.
3. RESULTS
3.1. Risk factors for poor pain control after total hip arthroplasty
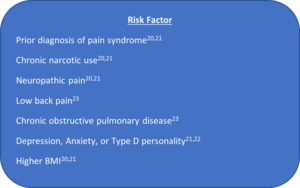
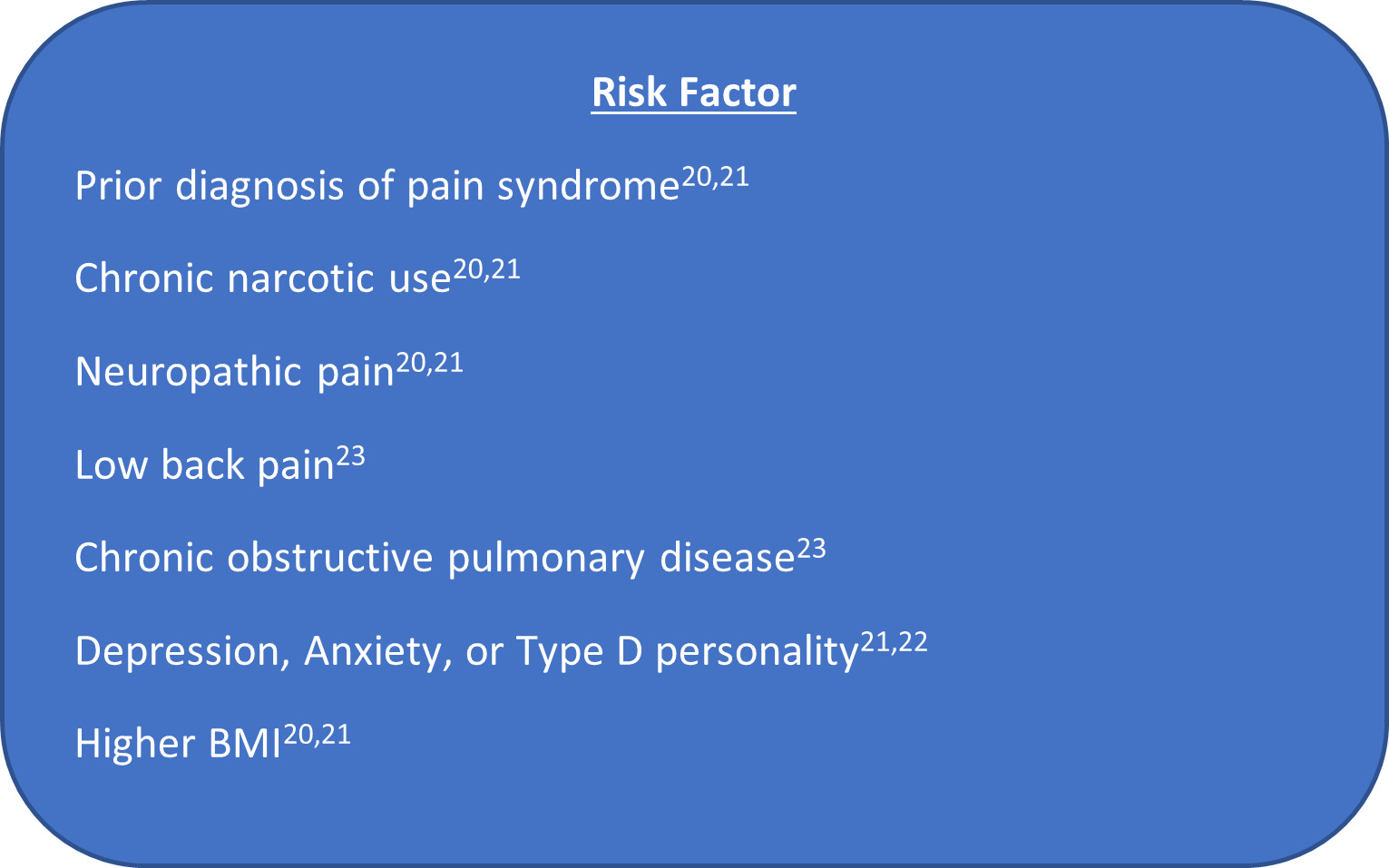
Multiple risk factors have been identified contributing to prolonged postoperative pain and prolonged pain medication use following total hip arthroplasty (Figure 1). These include the prior presence of a pain syndrome, chronic use of narcotics, and neuropathic pain.20,21 Pre-surgical pain intensity is the most significant clinical risk factor for developing moderate to severe persistent postsurgical pain.22 Specifically, the presence of low back pain and chronic pulmonary disease are risk factors for delayed pain relief following THA.23 One of the primary risk factors for neuropathic pain following THA is the presence of high preoperative pain.24
Depression has been named a risk factor for prolonged pain following THA by multiple studies.21,23,25 Other psychological risk factors for persistent postsurgical pain after THA include severe anxiety, chronic or negative emotional perception of the surgical disease, and Type D personality.21,22 Higher body mass index (BMI) and female gender are also risk factors for increased pain following THA.21,25
Resistance to liposomal bupivacaine as part of a multi-modal pain regimen can lead to failed pain management (pain score include ≥ 5) with risk factors including age < 64, history of pain management, smoking, and opioid use. Higher pain was also found in patients who received patient-controlled analgesia after surgery.26
3.2. Current state of the opioid epidemic
The United States currently consumes roughly four-fifths of the world’s total opioid supply.27 Currently, an estimated 92 million Americans are using opioids for pain relief.28 Opioid overdose deaths have increased by a factor of 6 as compared to the early 2000s. An estimated 130 citizens die daily from an opioid overdose.
An emphasis on pain control in postsurgical patients is partially at fault for the recent increase in opioid prescriptions over the past decade.29 Further, it is important to acknowledge that the recent increase in opioid prescriptions is not paralleled by an increase in the prescription for non-narcotic analgesics such as nonsteroidal anti-inflammatory drugs.28 Between 2000 and 2010, opioid prescriptions nearly doubled from 11.3% to 19.6%; however, nonopioid pain medication prescriptions only increased from 26% to 29%.28 Though this may represent a developing tendency to more aggressively treat pain, the proportionally larger increase in opioids is undeniable.
Further, the costs of opioids to American society cannot be overstated. The United States spends an estimated 50 billion dollars annually on the use of nontherapeutic opioids. The ongoing opioid epidemic plays a large role in the high costs of healthcare in the United States. However, worse, is the effect that prescription opioid use has had on drug addiction in the country.27,30
Multimodal analgesia has begun to appear in the literature as a highly promising strategy in anesthesia with the potential to reduce postoperative opioid use. Multimodal analgesia refers to the combination of anti-inflammatories, analgesics, and neuropathic agents and adjuncts to general anesthesia including regional anesthesia, local anesthetics, and better postoperative pain control without the use of narcotics. As mentioned in the last PROSPECT guidelines regarding THA, LIA has been recommended as a valid adjunct to nerve blocks.31 LB may improve the duration of analgesia given many new ultrasound guided pericapsular techniques.32,33 Though many articles find success with this approach, data suggests that multimodal analgesia has yet to be incorporated into the majority of orthopedic surgical practices.34 As the results of the present study demonstrate, liposomal bupivacaine may have the potential to decrease dependencies on opioid use after orthopedic surgery.
3.3. Opioid Overuse in Total Hip Arthroplasty – An Ongoing Epidemic
Several risk factors for opioid overuse after total hip arthroplasty. These are summarized in Figure 2. Risk factors for prolonged opioid medication use following THA include younger age (<65), back pain, fibromyalgia, chronic pain syndrome, drug potency > 10 morphine equivalents, and Opioid Risk Tool score (ORT) > 7, with the strongest risk factor being preoperative opioid use.35,36 Factors associated with greater opioid use in the first year following THA include chronic pulmonary disease, anxiety, and substance abuse. Additionally, factors associated with greater opioid use > 90 days post-THA were found to be female gender, peripheral vascular disease, higher BMI, and acquired immunodeficiency syndrome.36 A prospective study showed that depression was a risk factor for opioid overuse 2 years after primary THA.25
3.4. Standard periarticular analgesia in total hip arthroplasty
Before the recent conversation in the literature that shifted towards liposomal bupivacaine in total hip arthroplasty emerged, there were many promising studies regarding standard or non-liposomal bupivacaine in total hip arthroplasty. These are summarized in the current section. A randomized controlled trial examined the effect of intraarticular analgesia including postoperative pain at rest and during activity, analgesic consumption, complications, and range of motion within the first 48 hours following THA.37 The treatment group received an intraarticular injection containing a cocktail of morphine, bupivacaine, and compound betamethasone, while the control group received IV parecoxib only. The results of this study suggested that intraarticular analgesia injection significantly relieved early pain after total hip arthroplasty, as demonstrated by significantly lower rest pain scores on the visual analog scale in the treatment group compared to the control. Additionally, the treatment lessened analgesic consumption significantly, contributed to early rehabilitation of patients, and led to no visible adverse effects.37
Another randomized clinical trial investigated the effects of local and intraarticular analgesia techniques after hip arthroplasty in 80 patients. Ropivacaine, ketorolac, and epinephrine were used to infiltrate the local tissue around the hip joint intraoperatively and patients were then given a single-shot intraarticular injection 8 hours postoperatively.38 Results showed that the treatment group experienced significantly less narcotic consumption during the first 20 hours postoperatively (p = 0.004) compared to the control group (epidural analgesia infusion alone), which continued throughout the entire observation period. Furthermore, the treatment group experienced less pain both at rest and during mobilization (demonstrated by lower visual analog pain scores) starting at >20 hours and persisting through 96 hours postoperatively. The treatment group was also found to have an improved early walking ability relative to the control, which experienced a higher level of immobility due to leg block from the epidural analgesia (measured by the modified Bromage scale). The treatment group also had a shortened length of stay by 2 days (p < 0.001).38 Finally, the occurrence of side effects such as vomiting, urinary retention, constipation, and itching were lower in the treatment group, with the exception of nausea. Overall, this study found that local and intraarticular analgesic infiltration was associated with a significantly reduced consumption of narcotics, reduced occurrence of side effects, improved early walking ability, and shorter length of stay compared to the control group.38
Dobie et al. randomized 96 patients to either receive local periarticular analgesia (levobupivacaine with epinephrine) or a control (saline) solution. Their primary outcomes were differences in postoperative outcomes, including pain scores, opioid requirements, early mobilization, and length of hospital stay.39 They demonstrated no differences in postoperative pain scores, early mobilization 1 day after surgery, postoperative morphine consumption, level of assistance required to perform functional tasks, or length of hospital stay.39
Another randomized, double-blind placebo-controlled trial investigated the differences in pain scores up to 7 days postoperatively in patients undergoing bilateral THA who received a periarticular analgesic injection (PAI) in one hip and placebo injection in the other.40 They demonstrated that although the hips that received PAI did not have significantly less pain past the minimum clinically important significant difference as compared to the contralateral hip 24 hours after THA.
The most interesting of these trials explored intraoperative administration of high volume infiltrative periarticular analgesia followed by subsequent intraarticular analgesia (post-operatively). This randomized, double-blind placebo-controlled trial investigated the effects of high-volume infiltration analgesia with ropivacaine compared to control of saline in patients undergoing bilateral total hip arthroplasty. Patients received an intraoperative solution of high volume (170 mL) 0.2% ropivacaine with epinephrine (1:100,000) and saline placebo injection in the contralateral hip followed by postoperative intraarticular injections through an epidural catheter at 8 hours.41 Following surgery, patients were also given a multimodal analgesic regimen consisting of celecoxib, gabapentin, and paracetamol for breakthrough pain. Pain scores using the visual analog scale were calculated at various time points up to 48 hours postoperatively during flexion of the hip and at rest. The results of this trial showed no significant clinical difference in pain levels between hips, except for less pain at rest in the placebo injection site at 32 hours postop.41 This study not only confirms the prior literature that periarticular analgesia may not be as effective as intraarticular analgesia in decreasing pain after THA, but also that this effect may be such that it is only effective when done intraoperatively as post-operative scheduled intraarticular analgesia did not produce the same effect as that seen intraoperatively.39,40
3.5. Use of liposomal bupivacaine in total hip arthroplasty
The results of our literature search revealed nine articles that explored the use of regional liposomal bupivacaine in total hip arthroplasty. These are summarized in Table 2. Their discussion is presented below.
Asche et al. 201942 demonstrated great evidence regarding the use of liposomal bupivacaine in total hip arthroplasty. Through a retrospective cohort study of 7,232 patients from a public health database, the authors found that local, periarticular LB use in THA was associated with post-surgical opioid use, a decreased length of stay, and an increased likelihood of time to discharge, and decreased hospitalization cost. However, it is important to note that through the public health database used, the authors were unable to distinguish between LB use as local periarticular, local intraarticular, or the use of regional anesthesia.42 Currently, there is limited data in the literature to comment on whether or not LB use as a regional anesthetic has a role in total hip arthroplasty; future research is required on this topic.
It is important to consider the cost considerations of liposomal bupivacaine in orthopedic surgery. Beachler et al.43 echoed the results regarding the potential for liposomal bupivacaine to decrease postoperative opioid use in total hip arthroplasty. However, the study highlighted the significantly increased cost (Table 2, row 2). Thus, many advancements are likely necessary before liposomal bupivacaine can be integrated into standard protocols throughout the United States. As the industry around LB grows, this may become more feasible in the future.
Another important point to highlight when evaluating the literature in Table 1, is the variability in premedication of the patients. Domb et al. 201444 well describe their preoperative medication protocol which includes 1000 mg of acetaminophen, 400 mg of celecoxib, 75 mg of oral pregabalin, and 10 mg of oral celecoxib with extended-release oxycodone. It is important to consider the effects that premedication may have on interpreting the results of the cited studies.
A few of the included articles directly compare bupivacaine to standard bupivacaine through the level I studies.45–47 Johnson et al. 201745 demonstrate superiority when compared to post-operative pain control. This corroborates the results of the aforementioned studies; however, in their study, this did not extend to decreased postoperative narcotic use. Importantly, there LB group did contain standard bupivacaine in the administered injection, which may also make comparison difficult. Nonetheless, it is still an important, high-quality study that proposes the potential advantages of LB in THA.
3.6. Other Intraoperative Measures
Other intraoperative measures have been studied for use in conjunction with standard regional anesthesia via continuous epidural analgesia or peripheral nerve blocks. The alpha-2 adrenergic receptor agonist Dexmedetomidine (DEX), for example, can serve as a useful adjuvant during the intraoperative period upon intravenous infusion. This sympatholytic agent functions to blunt the surgical stress response to preserve hemodynamic stability while also reducing the patient’s oxygen requirements, minimizing the risk for intraoperative myocardial ischemia. Additionally, DEX works to potentiate the effects of other anesthetic agents thus reducing dosing requirements.48 In a study published in 2018, intraoperative sedation with DEX was associated with a lower incidence of post-operative dementia and cognitive decline compared to elderly patients sedated with supplementary propofol during hip arthroplasty.49
The efficacy of DEX as an adjuvant for intraarticular analgesia in total hip arthroplasty was further studied by Liu et al. This prospective randomized control study investigated the efficacy of fascia iliaca compartment block (FICB) in combination with DEX during postoperative and inflammation management for 119 elderly patients (≥ 60 years old) after total hip arthroplasty. The results showed that pre-operative DEX in combination with post-operative FICB enhances pain control while also lowering the serum levels of inflammatory factors as compared to groups receiving routine general anesthesia with an additional post-operative FICB. Sleep condition was also improved in the DEX + FICB group, and there were no obvious side effects of the therapy combination.50
Lumbar plexus blocks have also been studied as an alternative to traditional regional anesthesia in total hip arthroplasty. A case series of ultrasound-guided single bupivacaine injections to the quadratus lumborum was reviewed to assess effectiveness in postoperative pain control following THA. The review involves two patients who presented with difficult anesthesia management due to medical comorbidities. Following the quadratus lumborum block, neither patient required narcotics intraoperatively and both were able to participate in physical therapy with minimal discomfort.51
4. CONCLUSIONS
LB represents a useful local anesthetic adjunct for multimodal pain strategies in total hip arthroplasty with sufficient evidence to suggest that it may be useful in decreasing postoperative opioid use. This may represent a potential means by which the opioid overuse in total hip arthroplasty is combated; however, there is no literature to suggest whether preexisting demographic and medical risk factors can be compensated for with LB. LB may also be useful in improving hospital course, post-operative pain scores, time to ambulation, and patient satisfaction. Local infiltration analgesia “top-ups”, given through a wound catheter, exist as an option in the early postoperative period to reduce postoperative pain based on a surgeon’s clinical judgment. The high costs of LB represent a barrier to institutional acceptance of LB into standardized multimodal pain strategies. Further efforts should be aimed toward better understanding the current state of integration of LB into academic and private practice settings, industry movements to decrease the cost, and the role other adjunctive measures may have in reducing post-operative opioid use.
Author Roles
Study concept and design: N. V.; I. U.; O.V.; Acquisition of data: N. V.; I. U.; O.V.; Analysis and Interpretation of data: N. V.; R.S.; D.V.; N.C..; I.U.; O.V.; Drafting of the Manuscript: N. V.; R.S.; D.V.; N.C..; I.U.; O.V.; critical revision of the manuscript for important intellectual content: N. V.; R.S.; D.V.; N.C..; A.K.; I.U.; O.V.; Statistical Analysis: none; Administrative, technical, and material support N. V.; I. U.; O.V.; Study supervision: N. V.; I. U.; A.K.; O.V.
Disclosures Statement
We have no disclosures or potential conflicts of interest.
Further Information
We have no sources of funding to report for this manuscript.