Introduction
ACL tear is one of the most common sports-related injuries. With increasing life expectancy and physiological health, the participation in highly demanding activities in the middle-aged population is increasing.1 Therefore, the risk of ACL tears is becoming more frequent also in this age group.2
In young and active patients, ACL reconstruction has been regarded as a reliable procedure with excellent outcome for ACL tears.3 Traditionally, conservative treatments are mostly adopted in middle-aged and older patients.4 Studies reported that this procedure was associated with post-operative complications such as stiffness, residual pain and progression toward osteoarthritis (OA) with remarkable modifications of activity levels and lifestyles.4 So, actually more middle-aged patients have undergone ACL reconstruction to prevent decreased knee function and to maintain an active lifestyle.
A growing body of evidence has broadly changed the approach of the surgeons toward the management of the ACL tears in middle-aged patients.5–18 Several systematic reviews and meta-analysis19,20 have demonstrated that ACL reconstruction for patients older than 40 years could have comparable clinical outcomes as younger patients, including a greater return to sport activity. Moreover, although few studies have evaluated the outcomes of ACL reconstruction in patients with a cut-off of older than 50 years, a systematic review and a meta-analysis recently claimed that age was no longer a criterion contraindicating ACL reconstruction.21,22
The aim of the present meta-analysis was to update the literature on the safety of ACL reconstruction in patients aged 50 years and older. It has been hypothesized that patients older than 50 years would have comparable clinical and functional outcomes after ACLR than younger patients.
METHODS
The reporting in this systematic review follows the Preferred Reporting Items for Systematic Review and Meta-analyses (PRISMA) guidelines.23
Search strategy
A systematic review of the available literature published from date of inception to April 30, 2021 was performed using the keyword terms: “anterior cruciate ligament” “reconstruction” AND “middle-aged OR elderly OR over 50”. We used both MeSH terms and free text and utilized Boolean operators to combine them in searching. The following databases were accessed: Pubmed, Medline, Cochrane Reviews, Google Scholar.
Two authors (KC and SC) independently screened the titles and abstracts of the articles resulting from the searches. Potentially relevant studies were subsequently screened by full text reading. In case of disagreement, a consensus was reached by discussion, with the intervention of the third author (ASP). Reference lists of retrieved papers and review articles were hand-searched for additional relevant citations. Only peer-reviewed articles published in English were included in the systematic review.
Selection criteria
Studies included in the systematic review met the following inclusion criteria: (1) randomized controlled trials or comparative studies and (2) studies that compared the outcomes of patients older than 50 years and those younger than 50 years after ACL reconstruction. Studies were excluded if: (1) involved revision surgery without separate data, (2) animal or in vitro studies, (3) single-arm case series without a control group, and (4) studies with no usable data.
Data extraction
Two authors independently extracted data from the included studies using a standardized data collection form. The following information was included: first author, year of publication, study design (patient selection and concealment), details of the partecipants (number, age and sex), type of tendon graft, fixation device for the tendon graft, and outcomes data, which included functional scores, knee anteroposterior (AP) stability, and complications.
Quality assessment
We used the Methodological Index for Non-randomized Studies (MINORS) to assess the methodological quality of nonrandomized studies.24 The checklist includes 12 items, with the last 4 specific to comparative studies. Scoring was as follows: 0, not reported; 1, reported but poorly done and/or inadequate; and 2, reported, well done and adequate. The highest overall score was 16 for non-comparative studies and 24 for comparative studies. Each study was scored by two authors who reached consensus if disagreement occurred with the intervention of the third author (ASP).
Statistical Analysis
Statistical analysis was performed with Review Manager (Version 5.3, The Cochrane Collaboration). Risk ratio (RR) and odds ratio (OR) were used as summary statistics to perform statistical analysis of dichotomous variables, and the mean difference (MD) was used to analyse continuous variables. They were reported with 95% confidence intervals (95% CI), and P value of 0.05 was used as the level of statistical significance. Statistical heterogeneity between trials was evaluated by the chi-square and I-square (I2) test, with significance set at P<0.10. an I2 above 40% was considered to be significant. The random effect model was used in the presence of significant heterogeneity, while in the absence of significant heterogeneity, the fixed effect was preferred. A sensitivity analysis was conducted by excluding one study in each round and evaluating the influence of any single study on the primary meta-analysis estimate.
RESULTS
Study selection
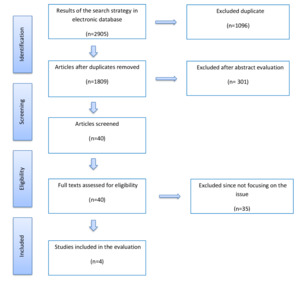
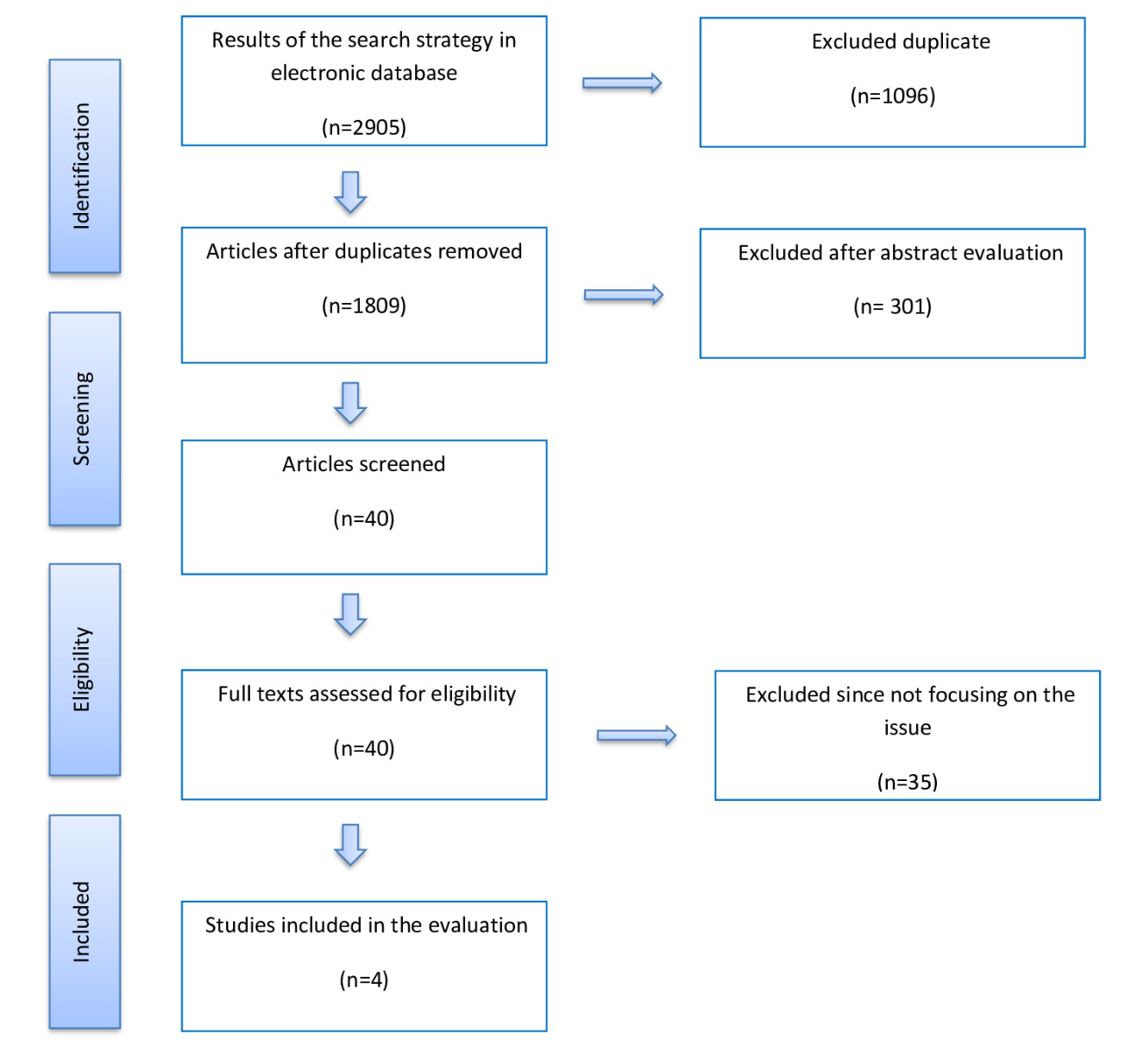
A total of 2905 studies were retrieved through electronic database searches and cross-references search. After removal of duplicates, 1809 studies were identified for title and abstract screening. Review of the titles and abstracts yielded 40 relevant studies for full text screening. From these, 35 studies were eliminated. Finally, we included 5 studies in the meta-analysis. Figure 1 shows the study flow-chart and searching results.
Study characteristics
Table 1 and 2 show the demographic characteristic of the cohorts reviewed and a summary of surgical details. A total of 357 patients with 50 years of age or older undergoing ACL reconstruction were identified from 5 studies, of which 188 were men and 204 were woman. The mean patient age was 54.7±1.3 years and mean follow-up was 31.8±21 months.
The cohort of patients younger than 50 consisted of 288 patients, of which 169 were men and 84 were woman. The mean patient age was 28.4±2.4 years and mean follow-up was 36.8±25.5 months. All studies presented retrospective design.
IKDC Score
Four studies reported IKDC score collected in a quantitative manner12–14,25 and only one study in a categorical manner (A, B, C, D).8 The post-operative scores improved from an average of 71.3 to 91.4 points in the over 50 group and from 73 to 96 points in the younger patient cohort. The pooled analysis revealed that the younger group had a significant higher IKDC score than the over 50 group at the end of follow-up (MD, -2.18 [95% CI -4.29 to -0.07]; P = 0.04; I2 = 41% for homogeneity) (Figure 2a; Table 3).
Lysholm Knee score
The post-operative scores improved from an average of 84.4 to 94.3 points in the over 50 group and from 85.8 to 96 points in the younger patient cohort. The pooled analysis revealed that these two groups had similar Lysholm scores at the end of follow-up (MD, -1.87 [95% CI -3.88 to 0.14]; P = 0.07; I2 = 0% for homogeneity) (Figure 2b; Table 3).
Return to Physical Activity
Of the 5 included studies, three evaluated the return to physical activity between over 50 and younger patients. The pooled analysis revealed no significant difference in Tegner scores at the end of follow-up (MD, -1.24 [95% CI -2.63 to 0.14]; P = 0.08; I2 = 90% for homogeneity) (Figure 2c; Table 3).
Anteroposterior (AP) laxity
Knee AP stability was measured by the mean side-to side difference at maximal manual traction with KT-1000 arthrometer (MEDmetric Corp., San Diego, CA, USA) or equivalent. Instability was defined as a mean side-to-side difference of greater than 5 mm. Only three of the included studies reported outcomes in knee AP stability. 5.2% of patients (5/96) in the over 50 cohort and 7.5% of patients (8/106) in the younger cohort had a side-to-side difference greater than 5 mm.
For this analysis, the calculation of risk ratio was based on the data regarding the number of patients with a side-to-side difference > 5 mm between two aged-groups. The pooled analysis revealed no difference between the two aged-groups (RR, 0.68 [95% CI, 0.23-2.01]; P = 0.49; I2 = 0% for homogeneity) (Figure 3a; Table 3).
Complications rates
Three studies reported post-operative complication rates. Of 281 over 50 patients, a total of 72 patients documented complications (25.6%): ACL graft failure, knee instability, loss of motion, anterior knee pain, arthrofibrosis. The pooled analysis showed that the over 50 group had a significant higher complication rate than the younger group at the end of follow-up (RR, 2.32 [95% CI, 1.45-3.71]; P = 0.0005; I2 = 33% for homogeneity) (Figure 3b).
Return to sport
Only two studies reported on return to sport activities of over 50 patients. Iorio et al25 indicated 100% returned to sport and 56% returned to preinjury level with a mean of 102 days in over 50 group compared to 93 days of younger group. While Panisset et al8 reported that return to initial sport was slightly earlier in over 50 group than younger cohort (266.8 versus 302.7 days).
DISCUSSION
The most important finding of the present meta-analysis was that comparable clinical and functional results were observed in patients over and under aged 50 years after ACL reconstruction. Conversely, over 50 cohort seem to have an increased risk for complication rate when compared with the younger cohort. This information is to be interpreted with caution, as findings are due by one large study8 that had a major weight (>70%) on the pooled results, hence making the conclusion based essentially on the results of this study and further investigations is needed. Nevertheless, we found that ACL reconstruction was a safe procedure for treating ACL tears in patients older than 50 years, especially those who would like to return to practice pivoting sports. These findings support our hypothesis that the age over 50 does not predict results in ACL reconstruction.
The result obtained were similar to those observed in the literature. A recent systematic review21 and following meta-analysis,22 reported similar results in terms of clinical and functional outcomes of the two cohorts. Both, are uncertain if there is a difference in terms of complications between the two groups. So, this aspect has not been clarified in this aged population, differently to the evidence regarding under and over 40 years of age that confirmed no difference in terms of complication rate between the two groups.15
Recently, there was a growing of studies that encourage the surgical approach in this population and these evidences could help surgeons with patient selection and adjusting expectations.5–14 At the same time, some surgeons are scared of the risk of a higher rate of complications, progression of OA and consequent poor results.
Pre-existing chondral and meniscal lesions are risk factors for complications, including arthrofibrosis and OA progression, and unfavorable outcomes following ACL reconstruction. These pre-existing conditions are a major concern in older patients. In addition, Dejour et al26 reported that female gender and medial meniscal lesions significantly compromised KOOS symptoms and pain, while lateral cartilage lesions significantly increased differential laxity. In our meta-analysis, 50% of the cohort of patients over 50 are female and three of the included studies reported preoperative cartilage status, associated ligamentous and/or meniscal injuries and relative treatment performed in concomitance to ACL reconstruction. This makes difficult the interpretation of the results in terms of rate of complications. In this scenario, the management of meniscal lesions represents a dilemma for the knee surgeons: whether to leave the meniscus untreated, or to suture or resect it. In this case, the first line choice is to repair. The rationale is that the meniscus must be preserved (repair or no-resection), if possible, as, in combination with ACLR, it protects the articular cartilage and the ACL graft, reducing residual laxity.27
In addition to this, a prolonged time from injury to surgery more than one year has been associated with an increased rate and severity of cartilage pathologies in patients with ACL tear, especially if they are older.27 In this meta-analysis, studies included analyse patients under and over 50 years of age both in chronic than acute setting. In the study by Kim et al12 underwent surgery within a mean of 20 months from injury, and those in the study by Osti et al13 underwent surgery no longer than 2 months from injury. One of the studies enrolled patients with both acute and chronic ACL injuries14 and another only acute ACL tear (mean of 23 weeks).8 Also this aspect has caused difficulties in the interpretation of findings, as well as the different post-operative follow-up. In this review, Cinque et al14 and Osti et al13 reported outcomes at more than 3 years revealing no significant OA progression after ACLR in patients older than 50 years. Kim et al12 e Panisset et al8 reported a follow up of a mean of 12 months and Iorio et al25 superior to 5 years.
Various types of tendon graft were used in the studies included: the BPTB (autograft and allograft), the double hamstring tendon autograft, and the quadrupled hamstring tendon autograft. BPTB and GST are widely used for ACL reconstruction and it can lead to satisfactory clinical outcomes.28 No evidence exists that one of the two grafts type is superior over the other, and the choice remains at the discretion of the surgeon.28 However, considering the reduced donor site morbidity and delayed return to pre-injury levels in the general population with hamstring tendon autograft or allograft, several authors have suggested BPTB in older and less active patients.28,29
This study is an up-to-date of the previous meta-analysis that compare the outcomes after ACLR between patients older than 50 and younger patients that included only comparative studies to avoid any further bias. Some limitations of this study should be mentioned. Particularly, the analysis of the literature showed some heterogeneity in terms of graft choice, tunnel technique and fixation method, interval to injury to surgery and the length of follow-up.
CONCLUSION
Comparable clinical and functional results were observed in patients over and under aged 50 years after ACL reconstruction. Compared to younger cohort, over 50 patients seem to have an increased risk for complication rate. Nevertheless, ACL reconstruction is a viable surgical option in patients aged 50 years and older, especially among patients who enjoy pivoting activities.

__lysholm_(b)__tegner_(c).tiff)
_and_complications_(b).tiff)
__lysholm_(b)__tegner_(c).tiff)
_and_complications_(b).tiff)