Introduction
Humeral diaphyseal fractures are estimated to be between 1% and 3% of all fractures occurring in adults.1 Their treatment once again confirms that uniformity of opinion in the trauma field is very questionable. In fact, no surgical method has yet established itself as the treatment of choice for the diaphyseal fracture of the humerus. It is true that in the past decades, non-operative treatment was the dominant one for this type of fracture. After all, richly vascularized, wrapped in a thick muscular coat, the humerus seems to be a district of the skeleton particularly suitable for orthopedic treatment as it is a biological area with not difficult osteogenesis even if not surgical treated. Supported by this, the authors who advocate the bloodless treatment of diaphyseal fractures of the humerus affirm that it is illogical as well as imprudent to surgically open the fracture, especially since the humerus, a non-load-bearing bone, forgives slight and modest shortenings and axial deviations without functional damage. If to these considerations we add the higher incidence of nonunion, an often-significant number of infections and the greater frequency of iatrogenic neurological damages resulting from surgical treatment, non-operative one is preferred by many. On the other hand, conservative treatment also presents non-negligible risks, such as delayed consolidation, malunion and the need for long immobilizations that cause significant shoulder and elbow joint stiffness. Consequently, surgical treatment is actual preferred in many cases. There are several surgical options: antegrade nailing, retrograde nailing and open reduction and internal fixation with plate and screws (ORIF), mini-invasive internal plate osteosynthesis (MIPO). Among these, antegrade nailing is certainly the most common treatment for diaphyseal fractures. The technical execution is simple, the operating time is reduced and it is not necessary to expose the fracture. It also allows the patient to move shoulder and elbow immediately after surgery, preventing stiffness. The other two methods are burdened by major disadvantages, such as the risk of iatrogenic fractures in the case of retrograde nailing and the huge bone exposure in the case of plate fixation, not to mention the risk of the radial nerve iatrogenic injury.2
The aim of the proposed study is to analyze the data in the literature in order to define the risks, advantages and disadvantages of the surgical treatment alternatives through a systematic review.
Methods
We conducted a systematic review of the literature according to the PRISMA guidelines,3 involving antegrade nailing, retrograde nailing and plate osteosynthesis for the surgical treatment of diaphyseal humeral fractures. The search engines used were: PubMed / Medline and Google Scholar. All prospective randomized or case-control retrospective studies published before November 2021 in English available as full text were included. Case-reports, pre-clinical studies, systematic reviews, descriptions of surgical techniques were excluded. The search included the following items:
“humeral shaft fracture” AND “intramedullary nailing”
“humeral shaft fracture” AND “open reduction” AND “internal fixation”
“humeral shaft fracture” AND “anterograde intramedullary nailing” OR “retrograde intramedullary nailing” OR “open reduction” AND “internal fixation”
The first selection of studies was performed on the basis of titles and abstracts. Studies that passed this selection were evaluated as “full-text”. The following data were extracted: authors, year of publication, type of study, number of patients, gender, fixation method, mean age (years), mean follow-up (months), postoperative complications, mean healing time (weeks), clinical evaluation scales used, operating times (minutes) and intra-operative blood loss (milliliters). The primary outcome considered was the fracture healing time by comparing the methods. The secondary outcomes were: the incidence of post-operative complications and the degree of patient satisfaction, further differences in terms of blood loss, surgical times, clinical scales and complications including infection. We also compared these parameters between reductions with plate performed with ORIF technique or with MIPO technique. The MIPO technique consists in the plate fixation without facture exposure. Data were collected on an Excel sheet (Microsoft) and a comparative statistical analysis was subsequently conducted with parametric or non-parametric tests depending on the variables analyzed. A p-value <0.5 was considered statistically significant.
Results
The search led to the identification of 506 studies, but only 30 fully met the established inclusion criteria. The in-depth analysis of the entire text of the manuscript led to the selection of only 10 studies valid for the systematic review.4–13 (Figure 1) The included studies were published between 2009 and 2020, involving a total of 562 patients, 391 males and 171 females. Of these, 270 underwent humeral nailing (of which 14 retrograde nailing), 208 ORIF and 94 MIPO. The average age of the patients included in the studies was 41.1 years (min: 37.3; max: 48). The mean follow-up of the studies was 16 months (min: 10; max: 24). (Appendix 1)
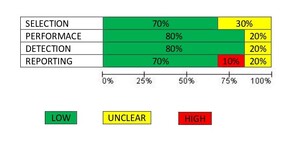
The quality assessment of the included studies was performed using QUADAS-2 and the results are presented in Figures 2-3.14
Intra-operative blood loss
5 papers report this data.7–9,11,13 In only one case the value related to MIPO is reported (147 mL) .11 The mean value of blood loss in the nailing group is 124.16 mL (min: 20; max: 206.8), while in the ORIF group is 261.91 mL (min: 150.23; max: 355.4). The difference found between the two comparison groups is statistically significant. (t: -2.391; p-value: 0.024), as intra-operative blood loss during ORIF is significantly higher.
Surgical times
The time requires for the surgical procedure is reported in 6 papers.7–11,13 Two are the data relating to the MIPO technique (mean: 113.36 minutes; min: 95; max: 131.71).15,16 The average value related to nailing is 89.63 minutes (min: 50.8; max: 126), while the average time related to ORIF is 109.32 minutes (min: 64.2; max: 150.58). Comparing parameters related to nailing and ORIF, a statistically significant difference is not obtained (t: -0.955; p-value: 0.182). In the same way, no significant differences are recorded by comparing nailing and MIPO (t: -0.873; p-value: 0.208) and ORIF and MIPO (t: -0.150; p-value: 0.443).
Healing time
This data is reported in 8 of 10 papers included in this review.4,5,7–9,11,13 Benegas et al., however, recorded a cumulative data (7.2 weeks), without distinguishing the fixation method used. Therefore, this value is not included in the analysis performed and reported below.5 The average healing time reported for nailing is 13.55 weeks (min: 6.7; max: 16.8), while the one related to the ORIF is 14.4 weeks (min: 10.6; max: 17) and to the MIPO is 15.8 weeks (min: 14.5; max: 17.1). Comparing the values between nailing and ORIF (t: -0.518; p-value: 0.307), between nailing and MIPO (t: -0.875; p-value: 0.205) and between ORIF and MIPO (t: -0.803; p-value: 0.226), no statistically significant differences are found.
Clinical evaluation
All studies included in this review report data from clinical scales at the latest follow-up.4–13 The DASH (Disability of Arm, Shoulder and Hand) scale is reported in 2 papers,4,13 the ASES (American Shoulder and Elbow Surgeons) Score in 5 ones,4,8,9,11,12 the UCLA (University of California at Los Angeles) Shoulder Score in 1 manuscript,5 the Constant Score in 1 paper,7 the MEP (Mayo Elbow Performance) Score in 1 paper10 and the Mayo Score in 1 paper.11 It is possible to compare the values obtained relative to nailing and ORIF only for the DASH scale and for the ASES scale, not recording statistically significant results (DASH: t 0.210; p-value: 0.427; ASES: t 0.558; p -value: 0.297). Therefore, there are no significant differences in the restoration of function following the two treatments under comparison.
Complications
Overall, data about failure, non-union, tools breakage, infections and interference with shoulder function are reported in all papers included in the review.4–13 Of 270 patients who underwent nailing, 74 developed complications (27.4 %). Complications were also observed in 21.2% (44 of 208 patients) of the patients who underwent ORIF and 13.8% (13 of 94 patients) who underwent MIPO. The Chi Square test allows to compare the incidence of complications between the three groups, obtaining that: the difference is statistically significant by comparing nailing with MIPO (Chi: 6.340; p-value: 0.012), while the difference is not significant between nailing and ORIF (Chi: 2.146; p-value: 0.143) and between ORIF and MIPO (Chi: 1.815; p-value: 0.178). In particular, infection were found in 5 of 270 (1.9%) patients who underwent nailing, 14 of 208 (6.7%) who underwent ORIF and 3 of 94 (3.2%) who underwent MIPO suffered from infection.4–13 The Chi Square test allows to compare the incidence of infection between nailing-ORIF and MIPO-ORIF, obtaining that: the difference is statistically significant by comparing nailing with ORIF (Chi: 7.331; p-value: 0.007), while the difference is not significant between nailing and MIPO (Chi: 0.587; p-value: 0.445).
Comparison ORIF-MIPO (Table 1)
An analysis was also conducted to compare the data relating to surgical time, intra-operative blood loss, healing time and complications (including infections) between patients undergoing ORIF4,7–9,12,13 and MIPO.5,6,10,11 Even in the presence of a substantial difference of cases enrolled in the two groups, no statistically significant differences are found.
Discussion
Humeral diaphyseal fractures can be managed in many modes depending on their characteristics. Even if described as the treatment of choice, rarely they are treated conservatively and more often the most popular treatments are nailing and plate osteosynthesis. Each of these methods has advantages and disadvantages. Surely nailing is less invasive on soft tissues and allows not to expose the fracture. On the other hand, the iatrogenic damage on the rotator cuff in case of anterograde nailing or the high risk of iatrogenic fractures in retrograde nailing can lead to serious complications for the patient.17 Moreover, not infrequently, the fracture can involve the distal third of the humerus requiring adjunctive open reduction and plating.15 On the contrary, ORIF allows an anatomical reduction of the fracture but involves the exposure of the fracture site, the excision of part of the periosteum and the risk of iatrogenic damage of the radial nerve. Moreover, it is more bleeding and it has a hypothetical higher risk of infection. The MIPO technique was born with the intention of overcoming some of these disadvantages, but it is often associated with suboptimal reductions and the risk of iatrogenic damage to nerve structures in a complex anatomical area such as the arm. The review of the literature that was conducted showed that there are no clear differences between these treatment methods. In particular, there were no differences in terms of functional outcomes as demonstrated by clinical scales and healing time. On the contrary, blood loss is certainly higher in the ORIF treatment, while the surgical times are superimposable as we might expect from the fact that the surgeon’s ability probably affects the result. In fact, there are surgeons more accustomed to nailing and others to ORIF, this means that the manual skills acquired in that method affect the execution times, reducing them. Similarly, performing MIPO compared to ORIF certainly safeguards soft tissues and the periosteum, but does not imply particularly short execution times, as reported by Benegas et al.5 Regarding complications, we recorded a statistically significant difference between nailing (27.4%) and MIPO (13.8%), while no significant differences were recorded between nailing and ORIF (21.2%). In our opinion, this data should be interpreted as follows: first, there is a considerable numerical difference between groups included, which obviously affects the results; furthermore, the nailing group includes retrograde nails, which are known to be burdened by major complications (iatrogenic fractures of the entry point) compared to anterograde ones, despite allowing optimal compression of the fracture site, as reported by Lian et al.11 This, along with the persistent rotator cuff pain that patients often complain in case of anterograde nailing, may have affected the outcome related to nailing. In 2016 Hohmann et al proposed a literature review based on 8 studies comparing nailing with ORIF and MIPO.16 They reported reduced surgical time for MIPO, a result not confirmed by our review. Complications are significantly lower for the MIPO group as also highlighted by our study, probably due to the interference on results of the rotator cuff pain related to nailing. In this regard, Ma et al. and Ouyang et al. reported similar data, underlining how nailing can significantly interfere with the functionality of the shoulder.18,19 In particular, Ma et al. investigated the influence of the two treatments on the range of motion of the shoulder after surgery: patients who undergoing ORIF reported better function of the shoulder.18 Similarly, Ma et al, Liu et al, Beeres et al reported no differences in healing time and clinical outcomes, as in our review.18,20,21 Liu et al. reported a greater tendency to healing delay in the ORIF group, probably related to the periosteal damage.20 Few studies in the literature report data relating to intra-operative blood loss, mentioned in the meta-analysis by Zhao et al. comparing nailing to the ORIF.22 They reported no difference in terms of surgical times and blood loss; the latter data is different from what we reported. In particular, we believe that the result is influenced by the fact that only 2 papers are analyzed by Zhao et al, while we report data from 6 papers (5 related to nailing and ORIF and 1 related to the MIPO technique).22 Therefore, we believe that it is particularly important to underline how a “closed” technique, such as nailing, leads to lower blood loss (about half) of than with alternative “open” methods, as we report in our review. At the same time, even if in a not statistically significant way, we found a reduced surgical time in case of nailing (about 20 minutes less). The most recent meta-analysis currently present in the literature is that of Beeres et al., which included 28 studies (18 observational and 10 randomized) for a total of 5431 patients undergoing nailing or ORIF.21 This review confirms much of the data that we have reported. This review does not report significant differences in the post-operative clinical scores, at the same time it reports a higher incidence of complications in the nailing group due to many cases of functional limitation of the shoulder which, in some cases, required revision surgery or early removal of the implanted nail. As in our case, Beeres also reported a decrease in surgical time in case of nailing. Furthermore, the evaluation of the data about infection extracted from the studies included in this review demonstrated that the risk of infection is statistically lower in case of nailing than ORIF (p: 0.007). This difference, on the other hand, was not found between MIPO and nailing as the exposure of soft tissues and bone is considerably less extensive (p: 0.445).
Conclusion
Humeral diaphyseal fractures require careful selection of the most suitable treatment method and careful pre-operative planning. While, on the one hand, small consolidation defects are easily forgiven from an aesthetic and functional point of view, on the other hand, there is the need to ensure the fracture healing in a short time, the least possible trauma on soft tissues and respect for vascular and nervous structures. This systematic review found that in the treatment of diaphyseal humeral fractures there are no differences between nailing, ORIF and MIPO in terms of healing, surgical time and restoration of function. Differences exists for blood loss and infection, which are significantly higher during ORIF, and in complications, which are lesser for MIPO.
Acknowledgements
Nothing to declare
Authors’ Contribution
MS and GL draw the study protocol; MS and CF and FF selected papers and wrote the manuscript; GL revised the manuscript critically.
Conflict of interest
Authors declare that they have no conflict of interest to disclosure.