Introduction
Septic arthritis (SA) is defined as an infection of the joint space caused by bacteria or any other infectious microorganisms.1 Septic arthritis was responsible for 16.000 emergency department visits in the USA in 2012.2 t is easy to think septic arthritis as a purely pediatric disease; Kang et al reported an incidence of 1 in 100,000 in industrialized countries and a higher incidence in developing countries (1 in 20,000 in Africa and 1 in 5000 in Malawi).3 But conversely SA is a frequent pathology even in the adult patient. The yearly incidence of septic hip arthritis is estimated at about 4-10 per 100,000 patients worldwide.
Most common risk factors for adult patients include: advanced age, pre-existing joint disease, recent joint surgery or injection, skin or soft tissue infection, intravenous drug abuse, indwelling catheters, immunosuppression, and diabetes.4–8 In the majority of cases, septic arthritis originates from hematogenous seeding of the synovial membrane and it is usually monomicrobial.9 The synovial tissue is highly vascular and is more susceptible to seeding. Alternatively joint infections are originated by local infection with subsequent bacteriemia, or by direct inoculation by open trauma. Gram positive organisms are the most common causative agent for SA with Staphylococcus aureus (including methicillin-resistant S. aureus, MRSA) being the most common in that group with a percentage of 52%; Gram negative, such as Streptococcus pneumoniae, Pseudomonas spp. account for approximately 10-15%, or polymicrobial infections (e.g. anaerobic species, Eikenella, streptococci) occur in a smaller percentages of cases especially in intravenous drug users, polytrauma, elderly and patient with underlying immunodepression, gastrointestinal or genitourinary compromise.9 Bacteremia is more likely to localize in a joint with pre-existing arthritis (e.g. rheumatoid arthritis, osteoarthritis, gout, pseudogout, Charcot arthropathy), particularly if associated with synovitis.1,10,11 Nevertheless, the immunocompromised (diabetes, HIV, drug and alcohol abuse) have greater risk for septic hip arthritis, occasionally healthy young adult patients with no other risk factors for this disease have been described.12,13 Although the majority of SA cases does not have causative bacterial microorganism, this is thought to be from early administration of antibiotics before arthrocentesis can be performed. Diagnosis of these cases is often delayed and nonspecific in the early stages of the disease. While host type and polymicrobial infection are strong predictors of severe consequences. The inflammatory process of the SA can lead to devastating consequences including acute destruction of joint cartilage.14 The estimated mortality rate due to complication for native hip arthritis is about 11%, but increased in case of prosthetic joint infection and elderly patient with comorbidity.15 Prompt diagnosis and treatment are pivotal in management of the infection: hospital admission for assessment, intravenous antibiotic therapy, and surgical treatment as deemed necessary.1 The diagnosis of adult hip septic arthritis occurs by microbiological confirmation via culture. Conventionally, septic hip arthritis was treated with resection arthroplasty, as described by GR Girdlestone16: in the last decades, new therapeutic approaches been developed: Arthroscopy treatment, open surgical debridement, and two-stage strategies (first stage, resection arthroplasty and implant on an antibiotic spacer; second stage, THA implant). Two-Stage total hip arthroplasty is safe and effective choice for the treatment of native infectious arthritis of the hip.12,17–21 One-Stage and Two-Stage demonstrated excellent results in terms of implant survival, function and quality of live; these techniques represent gold standard in case of joint damage.22
The development of modern antibiotics radically improved the success rate of this procedure that results often more than 90% after the first stage and reaches 100% after the second stage implant.17,19,23
Literature about SA is limited to case reports or case series with heterogeneous treatment. Many of the previous study have grouped different septic arthritis location irrespective that there are key differences between specific joints.
We describe clinical features, diagnosis, and treatment of an unusual case of septic hip arthritis in an adult patient with a non-contributory medical history and without any apparent primary source for the infection. The aim of the manuscript is to raise awareness of this uncommon condition among clinicians and warn about potential complications of a delayed diagnosis.
Case Report
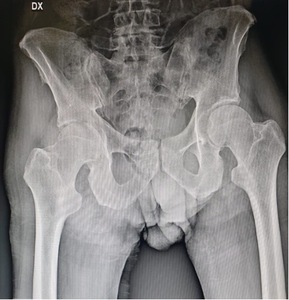
A 50-year-old male patient, working as a carpenter, presented to our attention with a one’s week history of acute right hip pain following a minor accidental hip hyperabduction injury. The patient presented with intense pain and was barely able to maintain upright posture. Past medical history was non-contributory, patient did not smoke and denied alcohol and recreational drug abuse. He had been taking pain medications and NSAIDs since the onset of the pain with no significant benefit. At this his current admission, physical examination showed soft tissue oedema around the right hip, no skin erythema, limited internal rotation of the hip joint or range of motion of the hip. Log-roll, Straight-leg-raise and Patrick test clinical test were positive. The most important clinical sign was the high grade of pain with an inability to bear weight without rest remission. There was no fever during the previous days and at the admission. Patient was admitted to our hospital where X-ray examination of the hip (Fig. 1) and laboratory tests were performed.
Given the negativity of both tests, an MRI of the lumbar spine and pelvis was performed: both examinations resulted negative. Patient was prescribed rest, analgesia, and periodic check-ups were scheduled. After 30 days the patient returned to our observation with unchanged symptoms but with the addition of a fever of 39° C lasting 48 hours, three days before the follow-up appointment. Repeat laboratory tests were significant respectively for a white blood cell count of 35.5 x 109/L, increased inflammatory markers with an erythrocyte sedimentation rate (ESR) of 97.0 mm/h and a C-reactive protein (CRP) of 47.8 mg/L.
A new x-ray examination of the right hip showed a marked joint line reduction (Fig. 2). A new MRI examination confirmed the presence of synovitis with joint effusion. (Fig. 2).
Hip joint aspiration was performed under local anesthesia by 3.5-inch trocar spinal needles with evidence of purulent material. The specimen was sent for microbiology testing, meanwhile the patient was started on a broad-spectrum antibiotic therapy consisting of intravenous Gentamycin and Rifampicin. Cultural tests showed the presence of a Methicillin-Resistant Staphylococcus aureus (MRSA). Based on cultural tests, antibiotic therapy was changed to Rifampicin and Daptomycin. Open hip arthrotomy with surgical debridement ad irrigation of the joint was planned to foster healing of the infection and preserve articular cartilage. However, at surgery articular cartilage of the femoral head was found to be completely damaged with subcondral bone exposure. Therefore, decision was made to proceed with hip excision arthroplasty surgery and spacer implantation (articulating spacer) cemented and loaded with antibiotics (Stryker NY) (Fig. 5). The surgery was performed under spinal anesthesia, in supine decubitus, through a “Direct Lateral” access route. The anatomical and surgical findings showed large destructive areas both of the femoral head and the acetabulum. After careful irrigation of the joint and surgical debridement, an articulating spacer was positioned with prosthetic components coated with cement and loaded with gentamycin. The surgery was followed by a rapid improvement of pain, patient restart independent ambulation within four days after surgery with aids for 2 weeks. The erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) inflammatory markers were respectively 32.0 mm/h and 7.0 mg/L as well as white blood cell count 12.7 x 109/L normalized within three weeks. At discharge, antibiotic therapy was prescribed for further 4 weeks along with follow-up check-up of the inflammatory markers to be performed at the end of the eighth week. We revealed progressive decrease of erythrocyte sedimentation rate (ESR) (27.0 mm/h) and C-reactive protein (CRP) (6.0 mg/L) inflammatory markers accompanied by lower white blood cell count of 9.5 x 109/L. Twelve weeks after index surgery, after obtaining a clinical ad laboratory values normalization, patient underwent the two-stage procedure with implantation a total non-cemented hip arthroplasty (ZIMMER BIOMET) (Fig. 6). Surgery was uneventful and patient was discharged home five days after surgery. At the time of the present writing, the patient completed the 1-year follow-up, complains of no pain and has resumed full work activity. No sign of recurrence was recorded.
Discussion
Adult septic hip arthritis is non-traumatic event, fortunately not frequent, that can affect any sex and age range.24 Often, it appears secondary to the haematogenic spread of bacteria from other locations, but cases have been described with no apparent primary source. The onset of the disease is dominated by pain and limping, erythema and local swelling, which are non-specific clinical signs.
Raised levels of inflammatory markers (i.d. ESR and CRP) can be noted during the early stages of the disease, whereas changes in the X-ray examination only become evident at a later stage.25,26 MRI examination performed at the onset of the clinical symptoms may show the presence of an intraarticular joint effusion. Suspected cases of bacterial arthritis should be evaluated promptly (CIT 1 SAHU). Initial work-up of suspected septic arthritis should include joint aspiration. Patients with symptoms of an inability to bear weight on the affected limb, fever above 38,6 C°, and elevated ESR and CRP are indicated for aspiration.
Obtaining a joint fluid sample is essential in order to achieve an early diagnosis with isolation of the responsible bacteria. The character of the synovial fluid aspirate may reveal turbid, purulent fluid with leukocyte count usually in excess of 50.000/mm3.
A suitable therapy, promptly established, can lead to a complete healing of the infection with no joint damage. On the contrary, a delayed diagnosis inevitably leads to inflammatory destruction of the joint with long term sequelae.27 About that seems that in native septic arthritis, in the absence of clinical sepsis immediate joint drainage does not appear to reduce the risk of sequelae compared with delayed drainage.28
Native septic arthritis of the hip represents an important challenge for the orthopedist, since this type of pathology can cause severe bone defects, an impairment of joint function with consequent worsening of patients’ quality of life. The two-stage technique is currently considered the treatment of choice in the management of patients with native active joint infection of the hip, as it guarantees high levels of eradication of the infection accompanied by a satisfactory medium-long term clinical and functional improvement.29 However in cases where the joint surface is highly damaged, an open debridement is recommended to prepare the joint for a future replacement or arthrodesis.30
The case reported in this manuscript shows two interesting and unusual aspects of this uncommon condition. First, our case shows that hip infectious arthritis can present without obvious systemic symptoms and negative laboratory findings. Second, despite close clinical follow-up, the infection can deteriorate rapidly and lead a complete destruction of the articular cartilage with joint function compromise. The staged antibiotic spacer is a well-known established method for chronic or late presenting SA and is also helpful treatment for patients who already had advanced degenerative changes before infection. Our patient was a perfect candidate for this surgical option due to the young age, general healthy status and the sudden worsening of the infection. The antibiotic spacer offers the advantage of consistent and higher antibiotic levels within the joint and usually will decrease the length of time that intravenous antibiotics are administered.1 These factors combined with the development of modern antibiotics increase the healing process and guarantee the immediate functional recovery and ambulatory status. Antibiotics should be continued until normalization of clinical and laboratory parameters (normally four to six weeks).27 Current case reports tend to perform the following indications: Open surgery with arthrotomy for patients with radiological sign of osteochondral involvement, extra-articular dissemination of infection or when the option for arthroscopic surgery is not available. Two-stage procedure with total hip arthroplasty is indicated when severe destruction of hip is already present and when joint preserving therapies are seldom successful.18
The results obtained in our case, in terms of implant safety, complications and functional results, are in line with what is present in the literature,31,32 although it has been reported that adults males tend to have an higher risk of complications.33
Acute onset hip joint pain can result from a variety of conditions, including trauma, transient synovitis, epiphysiolysis, Perthes disease, rheumatic arthritis, avascular necrosis, and metastatic lesions. Although varied, these conditions can share a similar clinical picture at the onset of symptoms. In an acute onset septic hip arthritis, the clinical picture is dominated by local and general signs (when present) including pain, limping and / or inability to weight bearing, fever, general malaise. Nevertheless, a high grade of clinical suspicion should be maintained when assessing patients with hip pain in order to rule out infection. When in doubt, obtaining a hip joint aspiration is paramount to exclude an infection.
Conclusion
Acute septic hip arthritis is an uncommon diagnosis that can lead to significant joint damage and long-term sequelae. This case report shows that clinical presentation can be non-specific, laboratory markers at the time of first presentation can be negative and at times there is no clue to direct the attention of the clinician towards a diagnosis of a septic arthritis. Nevertheless, the infection can progress rather quickly and lead to significant destruction of the joint. Once the joint is compromised, two-stage hip arthroplasty is a valid option to provide long term pain relief and restore mobility. We hope this case report will help raise awareness of this uncommon but dreadful complication and hip joint septic arthritis.
Author contributions
Fabio Zanchini and Valerio Cipolloni, Salvatore Lucchesi contributed equally to this work, generated the figures and wrote the manuscript (Conceptualization, Methodology, Software); Luigi Aurelio Nasto, Federico Fusini, Stefano Cacciapuoti, Piscopo Davide contributed to the writing of the manuscript (Data curation, Writing-original draft preparation); Enrico Pola, Raffaele Vitiello, Luigi Aurelio Nasto reviewed and approved the manuscript (Writing, Reviewing and Editing)
Conflict of interest
The authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript
Informed Consent
Written Informed consent has been given and retained by authors
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors