Introduction
Background: Humeral avulsion of the glenohumeral ligament (HAGL) lesions are a class of shoulder injury contributing to pain and instability in typically young and active patients. A HAGL lesion can affect any of the segments of the glenohumeral ligament: superior (SGHL), medial (MGHL), and inferior (IGHL) – comprised of the anterior inferior (AIGHL) and posterior inferior (PIGHL). Injury to the AIGHL is found in up to 93% of HAGL cases, with injuries to the PIGHL also causing clinical instability and pain at a lower rate.1 Most HAGL lesions are caused by a traumatic event like a dislocation or subluxation, and present with instability, pain, weakness, poor function.1 The incidence of HAGL lesions has been reported between 7.5% and 9.3% in patients presenting with glenohumeral instability, though underdiagnoses is possible due to a variable profile of symptoms and common concomitant shoulder injuries.1 Longo et. al2 established that operative management of HAGL lesions leads to superior outcomes and decreases recurrent instability compared to non-operative management highlighting the need for accurate identification and treatment.
Study Objectives: Two systematic reviews on HAGL lesions were published in 20162 and 2017.3 Longo et al. (2016)2 determined that surgical management (either open or arthroscopic) is more effective than non-operative measures at preventing recurrent instability. Bozzo et al. (2017)3 reviewed the indications for surgical treatments and detailed patient demographics, common associated pathology, and outcomes. An updated systematic review is needed given the evolution of surgical techniques in recent years1,4 and the increasing age of the data analyzed in the previous systematic reviews—which contained data up to June 2016. This systematic review aims to further elucidate the clinical outcomes of HAGL lesions, and to generate data that will inform physicians’ diagnosis and clinical decision-making regarding HAGL lesions.
Methods
Literature and Database search
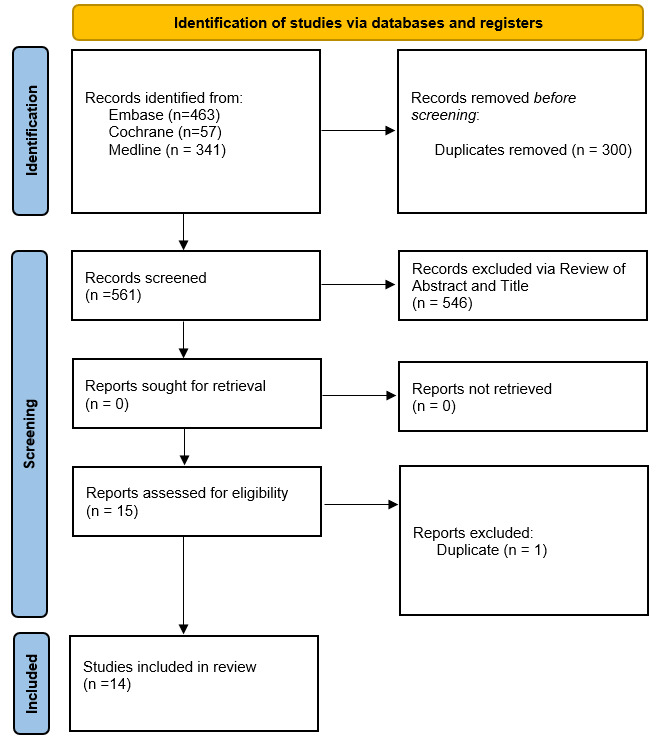
The review began with a search of the following databases for studies describing HAGL lesions since the publication of previous systematic reviews: Medline, Cochrane, and EMBASE. A systematic search of peer-reviewed, published literature was then conducted in consultation with a research librarian in Medline (Ovid), Embase (Ovid), and Cochrane from inception of the database to April 14, 2022. The search consisted of a combination of keywords and controlled vocabulary for the following concepts: HAGL, humerus, instability, lesion, dislocation, and humeral avulsion glenohumeral ligament. The full details of the search strategy for Medline, Embase, and Cochrane can be seen in Appendices 1, 2, and 3 respectively. All references were imported into Endnote reference management software (Clarivate, https://endnote.com/) and duplicate references were removed, as shown in figure 1. The remaining references were exported and uploaded to Rayyan (https://www.rayyan.ai/) for screening.
Eligibility Criteria and Study Selection
The first review of studies screened abstracts and titles as shown in figure 1. Two blind reviewers (CN, CR) included studies in English that chiefly investigated operative or non-operative HAGL interventions and their indications and clinical outcomes. Case reports, case series, retrospective cohort studies, and randomized controlled trials published no earlier than June 2016 were included. Studies were excluded if they did not directly investigate management of HAGL lesions. Likewise, reviews, cadaveric studies, non-human studies, and non-English studies were excluded. Studies then underwent a second full text review based on the same criteria to exclude any additional studies as needed. Any conflicts between reviewers were resolved through third-party consultations with a senior author (JS).
Methodological Quality Assessment / Risk of Bias
Methodological quality of included studies was assessed using the JBI protocol checklist (https://jbi.global/critical-appraisal-tools) for cohort studies, case series, and case reports, respectively. Each criterion consists of unique vetting questions that evaluate the validity of methods, appropriateness of analysis, and quality of presentation for their given study type.
Data Extraction
For each included study, two authors (CN, CR) independently extracted data into a spreadsheet formatted to highlight key data points. A second review of the extracted data sheets was then performed by the opposite reviewer, with any discrepancies between reviewers being resolved through third-party consultation with a senior author (JS). Data points for extraction from each study included the following: study type, level of evidence, number of patients, sex, mean age, mechanism of injury, indication for treatment, treatment, follow up duration, post-operative complications, associated injuries, and outcome parameters: clinical outcome scores, clinical evaluations, and return to activity.
Statistical Analysis
Meta-analysis was not performed. Categorical variables will be summated and presented as counts or proportions, and continuous variables will be presented as means. Outcomes of interest will be displayed via tables highlighting individual studies and their findings. Findings from data synthesis will be illustrated by tables and figures generated by the research team.
Results
Literature Search
Our initial search of the three databases yielded a combined total of 561 papers after duplicates were removed. After screening, 14 studies were found that met the review criteria for inclusion. The flowchart in Figure 1 displays the results of each step of the screening process with number of studies and reasons for each decision made. Our results are reported in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) reporting standards (PRISMA).5
Methodological Assessment and Risk of Bias
Two blind reviewers (CN, CR) analyzed studies according to JBI Clinical appraisal tools for each study type. Eight case reports6–13 had a mean score of 7.88 out of 8. five case series14–18 had a mean score of 9.8 out of 10, and the sole retrospective cohort study19 was scored 11 out of 11. Both reviewers scored each study the same, with no discrepancies. These scores suggested that all 14 studies had adequate methodology to be included in the review without unnecessary risk of bias.
Data Extraction and Analysis
This study reviews 13 studies with level IV evidence that were either case reports6–13 or case series,14–18 and one retrospective cohort study with level III evidence.19
Demographics
A total of 119 patients were identified with 82 males (68.9%) and 37 females (31.3%) with a mean age of 24.08 years in 13 studies with reported means. Follow up intervals ranged from two weeks to two years. Of the 51 injury mechanisms reported, 12 (23.5%) resulted from sports, 21 (41.2%) from fitness training, and the remaining 19 (37.3%) from unspecified trauma.
Indications for Treatment
The most common indications for surgical treatment were instability (n=97, 81.5%) , pain (n=40, 33.6%), and recurrent instability (n=11, 9.2%). Weakness and failed conservative treatment were also noted as indicators for surgical treatment. There were 51 cases (42.9%) that reported use of imaging to either confirm clinical suspicion of or identify HAGL lesions. Imaging modalities included preoperative magnetic resonance arthrogram (MRA) with contrast, multidetector computerized tomography (MDCT) and magnetic resonance imaging (MRI). As illustrated in Table 2, the remaining 68 cases (57.1%) did not include imaging modalities in reporting their clinical indications.
Associated Injuries
There was a total of 85 associated injuries across the 119 patients (Table 1). However, given that there can be multiple associated injuries per patient, and that some studies were not explicit in providing ratios of prevalence for associated injuries, this study was unable to generate an exact percentage of patients who presented with associated injuries. However, the reported associated injuries listed from most common to least common are as follows: 29 non-descript labral tears (34.5%), 19 Bankart lesions (22.4%), 16 rotator cuff tears (18.8%), 11 Hill-Sachs lesions (12.3%), 8 SLAP lesions (9.4%), and two cases of Axillary nerve palsy (2.4%).
Management and Complications
Surgical data and complications are shown in Table 2. 117 patients were managed with surgery performed in either an arthroscopic or open manner. There were 60 open and 57 arthroscopic repairs reported. Of the 117 procedures, 11 complications (9.4%) were reported which included: 3 recurrent dislocations (2.6%), 4 counts of post-operative apprehension (3.4%), and 4 revision surgeries (3.4%). Indications for revision surgery included long head of bicep tenodesis (n=2), loose anchor screw from poor insertion technique (n=1), and subscapularis retear (n=1).17,19 Among the 11 reported complications 5 (45.5%) followed open procedures, and 6 (54.5%) followed arthroscopic procedures.14,17,19 One case reported non-operative management of a HAGL lesions due to a surgical contraindication of Axillary nerve palsy.7,10
Outcomes and Return-to-Activity
Clinical outcome scores were reported in 7 of 14 papers with a variety of assessment tools used (Table 2). Rowe score was the most used metric, found in 4 studies.14,16,17,19 In two studies with reported means,14,19 21 patients had a mean postoperative Rowe score of 86.7. Likewise, the two remaining studies16,17 reported a 35.5-point postoperative improvement, and median score of 85 in 23 and 15 patients, respectively. A visual analog pain scale (VAS Pain, 10 point scale) was utilized in 3 studies7,17,19; 2 studies reported a mean postoperative pain rating of 1.6 in 16 patients,7,19 while the third reported a mean improvement of 6.6 points in 23 patients.17 The Western Ontario Shoulder Stability Index (WOSI), Oxford Shoulder Instability Score (OSIS), Constant-Murley score, and Simple Shoulder Value (SSV) were reported in two studies each (Table 2). The following metrics were each reported in only 1 study: Quick Disabilities of the Arm, Shoulder, and Hand (Q-DASH), Shoulder and Elbow Surgeons Shoulder Score (ASES), Single Assessment Numeric Evaluation (SANE), and Simple Shoulder Test (SST).
Return to activity data was available for 8 studies with 88 of 91 (97%) patients returning to some level of activity and 57 of 70 (81%) patients returning to a similar level of activity to preinjury (Table 2). Of the three studies investigating military populations,10,11,15 29 out of 29 (100%) patients returned to military duty post-injury, including one patient that returned to Special Forces units after nonoperative treatment.
Other clinical outcomes, including range-of-motion (ROM), strength, and instability tests, were available in 9 studies (Table 2). Post-treatment ROM values of various movements were reported in 3 studies totaling 16 patients; two of these reported good ROM in all movements except significant postoperative decrease in external rotation ROM compared to the contralateral shoulder,12,14,16 while the third case report reported good postoperative ROM at 9 months follow-up as the patient was cleared to resume playing football.12 Likewise, three additional cases6,9,10 reported post-treatment ROM as either satisfactory or improved in each of the three cases. A comprehensive account of any other clinical outcome evaluations can be found in Table 2.
Discussion
These findings highlight that majority of HAGL lesions occur alongside associated injuries to the shoulder with 119 cases having 85 different associated injuries. Likewise, high rates of non-descript labral tears, Bankart lesions and rotator cuff lesions corroborate the findings of two prior systematic reviews2,3 and confirm that HAGL lesions often do not occur in isolation. This review found that the most common associated injuries were non-descript labral tears (n=29), Bankart lesions (n=19), rotator cuff tears (n=16), and lastly Hill-Sachs lesions (n=11). When comparing these current findings to the two previous systematic reviews, similar incidence of total associated injuries was found between all studies. However, no specific associated injury occurred as ‘most common’ across all studies. This study reports non-descript labral tears as most common, Longo et. al.2 reported Hill-Sachs lesions, and Bozzo et al. (2017)3 reported Bankart Lesions. Associated injuries may influence clinical outcomes as shown in a study evaluating HAGL repaired with concomitant rotator cuff lesions showing increased operative times and lower patient reported outcome scores.16 As HAGL lesions often occur alongside other injuries that may be more prevalent and easily detected, it is logical to consider the potential for undetected HAGL lesions that likewise contribute to patients’ symptoms. To mitigate this risk Longo et al.2 established the imaging modalities, imaging findings, and intraoperative pearls that are best used for diagnosing HAGL lesions. These findings endorse the utilization of proper diagnostic protocols, and corroborate the position of Bozzo et. al3 in encouraging a high clinical suspicion of HAGL lesions in the presence of these associated injuries, to ensure that they are detected and treated.
The results of this review suggest satisfactory clinical outcomes following HAGL repair corroborating the findings of the two previous systematic reviews.2,3 High rates of return to activity (97%) and improved functional outcome measures were reported, similar to the good clinical outcomes reported by Longo et. al (2016)2 and Bozzo et. al (2017).3 Longo et al.2 found improved functional outcome scores and zero instances of postsurgical complications, and Bozzo et al.3 reported significantly improved outcome scores, and only 2 of 79 patients who were unable to return to similar levels of sport. Despite these similar findings however, this current study reports a postoperative complications rate of 9.4% including patients who experienced recurrent dislocations, apprehension, or revision surgeries, compared to zero reports of postoperative complications in either of the previous systematic reviews. Furthermore, this study’s data showed that only 81% of patients were reported as returning to a similar level of preinjury activity, which is noticeably lower than the 97% reported by Bozzo et al (2017).3 These discrepancies may be explained by differences in surgical skill level, case by case variation of the degree of injury to shoulder, or sample bias.
It is worth noting two accounts of nonoperative management of HAGL lesions exist in literature since June 2016. One case showed mild improvement of an isolated HAGL lesion, while the other reports a ‘serendipitous’ recovery in the environment of a traumatic injury involving axillary nerve palsy where surgery was not an option.7,10 Regardless, HAGL lesions remain to be treated best by using surgical interventions over nonoperative management as established by Longo et al. (2016).2
Strengths: This study’s search was broad in its scope and a thorough review of included studies provided an up-to-date and comprehensive clinical picture of HAGL lesions. Building on the work of two previous systematic reviews,2,3 this systematic review updates relevant data with analysis of studies covering 119 total lesions from a variety of patient populations including athletes, military, and non-athletes. Evaluations of the clinical presentations of HAGL lesions, non-operative and operative managements, and outcome measures further serve to strengthen the breadth of this study. Likewise, this review serves as a timely clinical companion to the Krueger et. al’s recently published review on HAGL diagnosis and management.20 These two studies serve to increase the current awareness and strengthen the body of knowledge regarding HAGL lesions.
Limitations: This study is limited by the level of evidence of included studies (13 Level IV studies, one Level III). The depth of analysis was limited by both what these studies reported as outcomes and how outcomes were reported. Some studies were not explicit enough to obtain certain statistics and counts, like the exact number of isolated HAGL lesions versus HAGL lesions occurring with associated injury. Furthermore, reported outcomes were often too heterogenous to summate or average in order to generate overarching findings. Additionally, 8 of the 14 included studies were case studies and therefore, the 6 remaining studies accounted for most of the derived results. Lastly, some of the reported counts are not necessarily indicative of the true population distributions due to varying inclusion and exclusion methods utilized across the different papers. For example, the open versus arthroscopic surgery counts were skewed by on study that only included open procedures. Similarly, a small number of physicians performed each of the surgeries and thus physician preference likely introduced additional bias.
Conclusions
HAGL lesions are a common source of instability and frequently present with concomitant injuries of the shoulder. Untreated, they can lead to recurrent instability. This updated systematic review shows that HAGL lesions appear to respond well to surgery with low complication rates. Physicians should have a high index of suspicion for HAGL lesions as surgical repair provides good outcomes with low rates of recurrent dislocation. Increased clinical detection has potential for reduction in the incidence and prevalence of persistent instability and pain in patients with multiple shoulder injuries.
Author Contributions
Chase Nelson – prospective literature review, submitted IRB, reviewed papers, performed analysis, built table, performed risk of bias, wrote bulk of paper, formatted paper, wrote reference list.
Charles Reiter – reviewed papers, performed analysis, built table, performed risk of bias, wrote various results sections, edited drafts.
John Cyrus – performed database searches to gather papers, helped write methods section.
James Satalich – oversaw protocol, guided reviewers’ efforts, edited and revised drafts.
Robert O’Connell – oversaw paper structure, analyzed and critiqued drafts, provided edits.
Alexander Vap – principal investigator, identified research question, signed off on paper prior to submission.
Disclosures
The authors have no disclosures, conflicts of interest, or funding to report.