Introduction
Total joint replacements are one of the most common surgical procedures in America, and they are being performed at an increase rate. Hip and knee replacements are projected to increase by 71% and 85%, respectively, by 2030.1 As of 2010, there were over 1 million total hip and knee replacement procedures performed each year in the United States.2 In the United State from 1959 to 2016, life expectancy has increased from 69.9 to 78.9,3 one can assume that total joint replacements will only become more prevalent as the population of the United States continues to age. Predictions show that the number of total knee arthroplasty will increase 14% between 2012 and 2050.4 With new advances in the field, better optimization, rapid recovery protocols, and new technology, patients are recovering faster and expected to go home sooner.
Currently, most joint replacement surgeries are still performed as inpatient procedures, even though Medicare has taken them out of the in-patient only list, However, there are factors that may cause a shift in this paradigm. Firstly, outpatient total knee arthroplasty (TKA) reduces the cost, on average, by $8,527 and has been shown to be efficacious and safe, given that the patient meets appropriate inclusion criteria.4 When comparing outpatient THA vs inpatient THA, patients undergoing outpatient THA have reported better outcomes in several categories without any statistically significant detriments.5,6 Early studies show promising results in terms of outpatient joint replacement surgery. Therefore, it is no surprise that even before COVID a 2019 study predicted that half of all primary joint arthroplasties will be performed in an outpatient setting by 2026.7
Given the prevalence of the surgery and the trajectory in which it is going, the authors of this paper sought to analyze the current literature on outpatient total joint arthroplasties. The analysis will be in the form of a bibliometric review, focused on citation frequency. A citation analysis, which this is commonly termed, involves using the number of citations a publication has amassed to quantify its influence on the field. Though direct impact cannot be directly correlated with total number of citations, this analysis creates a baseline for how far TJA research has come and may elucidate any trends for future researcher and clinicians alike.
Methods
The database used to collect the data for this analysis was Clarivate Analytics Web of Science (WoS), a global publisher-independent citation database. A search query which optimized the number of results and quality of publications was used. This was accomplished via different iterations of Boolean search terms. The final search query selected and used to collect data was: “outpatient or ambulatory,” with a “Title” filter AND “total joint replacement” AND “total joint arthroplast*” with “Topic” filters. Specifically, the term “arthroplast*” was used to avoid unnecessary omission of articles with topics including a plural or past tense term. This search yielded 170 unique results, which required no additional filtering. The papers returned were then sorted by total number of citations and exported to Google Sheets for further analysis. An initial review of this search was deemed acceptable by two independent reviewers (JW and JL), with the understanding that some articles would need to be excluded on the grounds of being tangential or related to Outpatient Total Joint Replacement, but not being included as the primary topic of investigation.
67 papers, in total, were reviewed by two independent reviewers (JW and JL). 50 were deemed acceptable as their primary focus of investigation was Outpatient Total Joint Replacement. 17 papers ended up being excluded from our analysis, primarily pertaining to anesthesia care, post-operative physical therapy modalities, or inpatient total joint replacement.
The full-text publications of the top 50 included results were then reviewed to determine the Level of Evidence according to Oxford’s guideline. The guidelines for Level of Evidence were as follows:
1 = Systematic reviews of randomized trials, or systematic reviews of inception cohort studies.
2 = Systematic reviews of cohort studies, inception cohort studies, cross-sectional studies, randomized trials, or observational study with dramatic effect.
3 = Cohort studies (primarily retrospective), epidemiological/observational study
4 = Case-control studies, low impact cohort studies, animal trials
5 = Simulations, models, or mechanism-based reasoning
The publications were simultaneously reviewed for classification within the following categories: Clinical Outcomes, Classification, Clinical Guidelines, Economics, and Perceptions. These categories were selected by the authors as the most common topic observed in the top 50 publications.
Using the analysis tools included in the Clarivate Analytics Web of Science (WoS) database, additional data was obtained from the 50 included publications including: primary author, country of origin, number of citations overall, year of publication, and publishing journal. To mitigate inflation in citation quantity for older articles, the results were also sorted by number of citations per year since their publication.
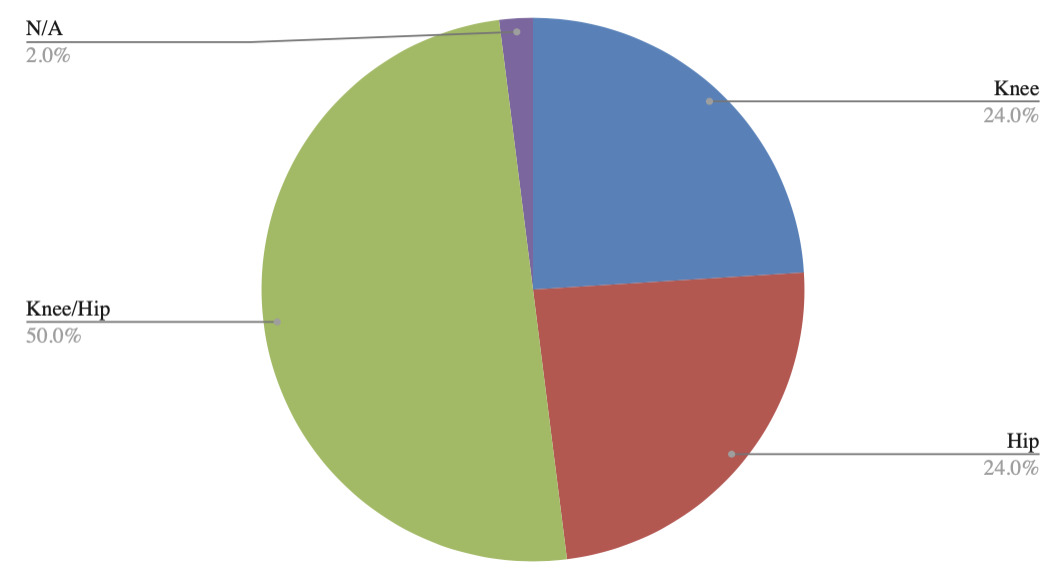
Lastly, the reviewers stratified the publications based on what joint was replaced in each of the papers. This was broken down into Hip, Knee, Hip and Knee, Shoulder, Ankle and Elbow. Shoulder, Ankle, and Elbow were excluded. Only Hip, Knee or papers that included both Hip and Knee were included in the study.
Results
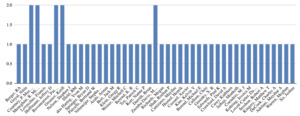
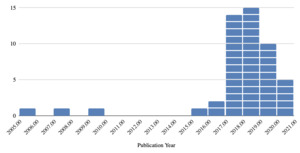
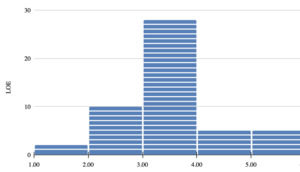
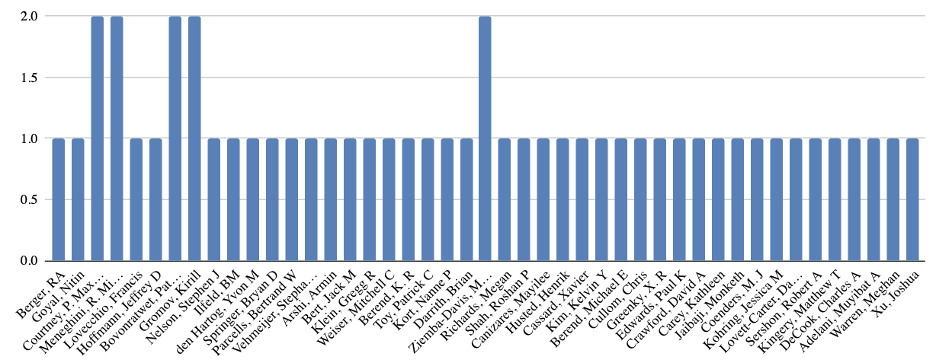
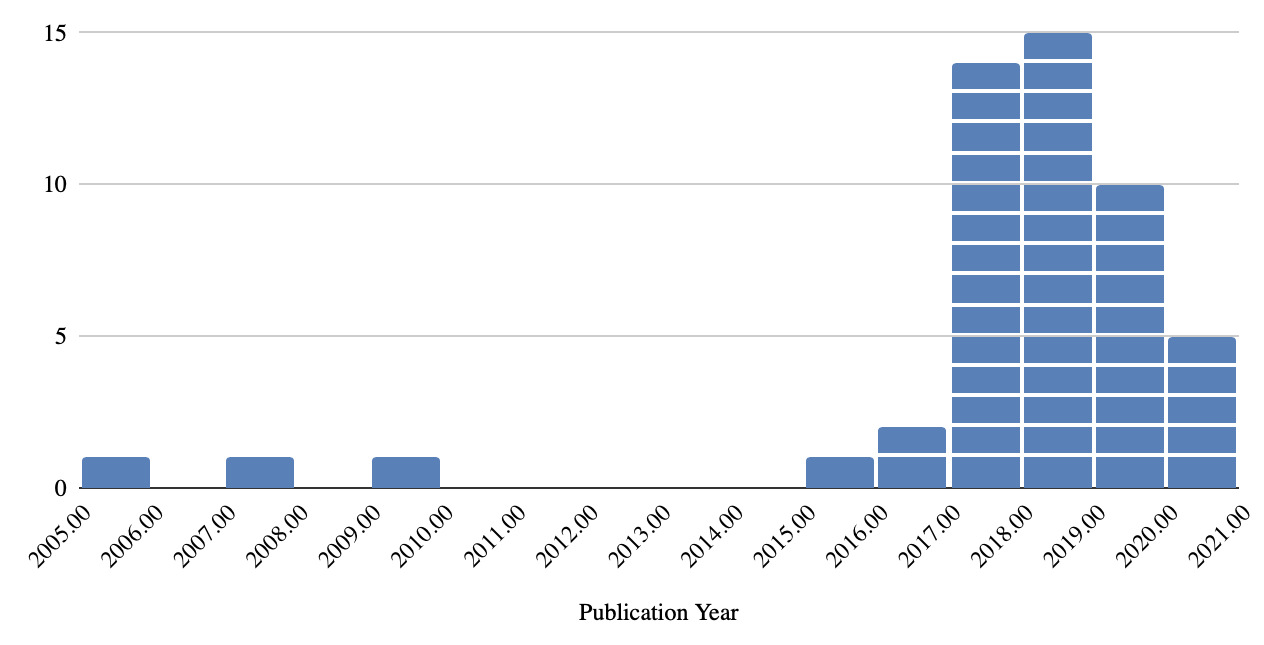
There were five authors who contributed two publications each (Bovonratwet, Courtney, Gromov, Meneghini and Ziemba-Davis) [Figure 1]. The most most popular year for publication was 2018 [Figure 2], which produced 15 publications (30%), followed by 2017, which produced an additional 14 publications (28%). There were zero publications in 2006 and 2008, as well as from 2010-2014 [Figure 2].
Six countries could be attributed to all 50 publications analyzed in this study [Figure 3]. The country that produced the most publications was the United States (n=40), the countries with the second most publications were Denmark (n=4) and The Netherlands (n=4). The remainder of the publications could be attributed to Canada, England, and France. The Indiana University System was the institution(s) with the most attributed publications (n=12), followed by Rush University (n=7) and the University of Copenhagen (n=4) [Table 1]. Eight other institutions were attributed with three publications.
The 50 publications analyzed for this study were cited a total of 1,774 times (including self citations). The average number of citations for the top 50 articles was 35.5 citations per publication. The raw numbers for total citations and citations per article may be skewed lower due to the recency of the publications, on average. The most cited article amassed 147 citations while the least cited article was cited 8 times. The most recently published article in the top 50 was published in 2020 and the oldest publication analyzed was published in 2005 [Table 2].
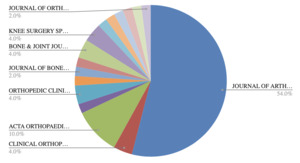
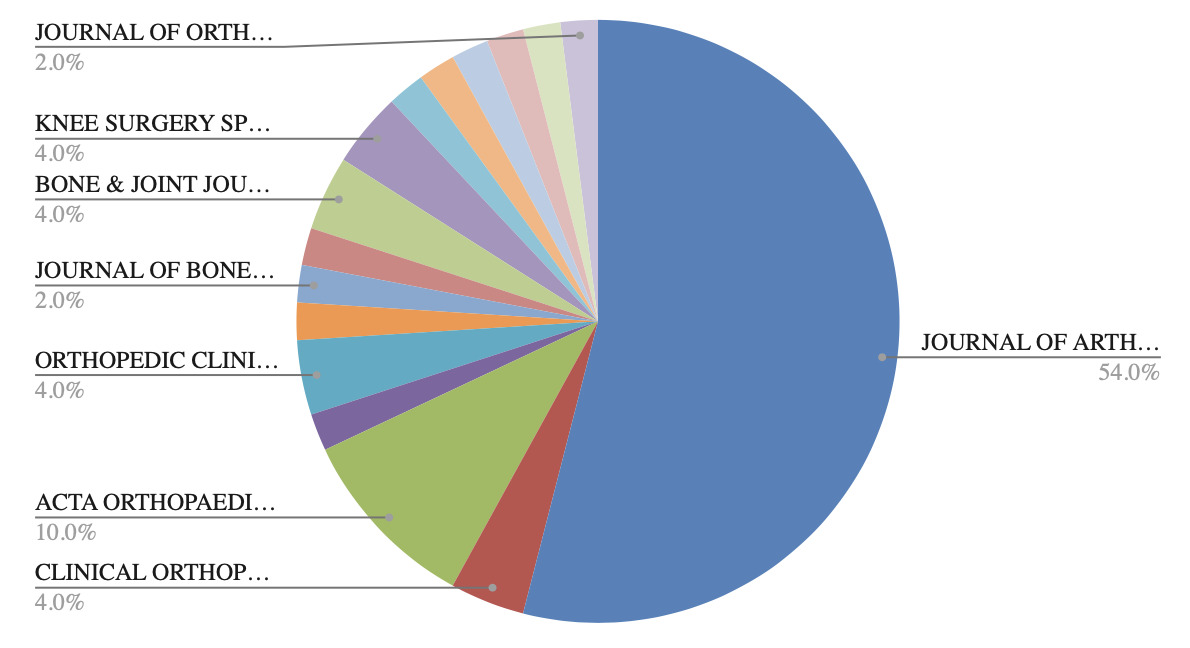
The journal that published the most articles in this study was Journal of Arthroplasty, publishing 27 articles (54%). This was followed by ACTA Orthopaedica with 5 publications (10%). In total, our study included papers from 16 different journals [Figure 4].
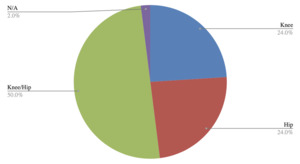
Both Total Hip Arthroplasty and Total Knee Arthroplasty were equally investigated in this study with 12 unique papers each. After excluding Total Shoulder Arthroplasty, Total Ankle Arthroplasty, and Total Elbow Arthroplasty, there was only one remaining publication that described Outpatient Total Joint Replacement in general, rather than with respect to specific joints. Although, most of the current literature remains focused on hip and knee. Additionally, our authors found that papers with titles describing “Joint Replacements” almost always referred to both hip and knee arthroplasty. Of note, 25 publications focused on both hip and knee replacement outpatient surgery. [Figure 5].
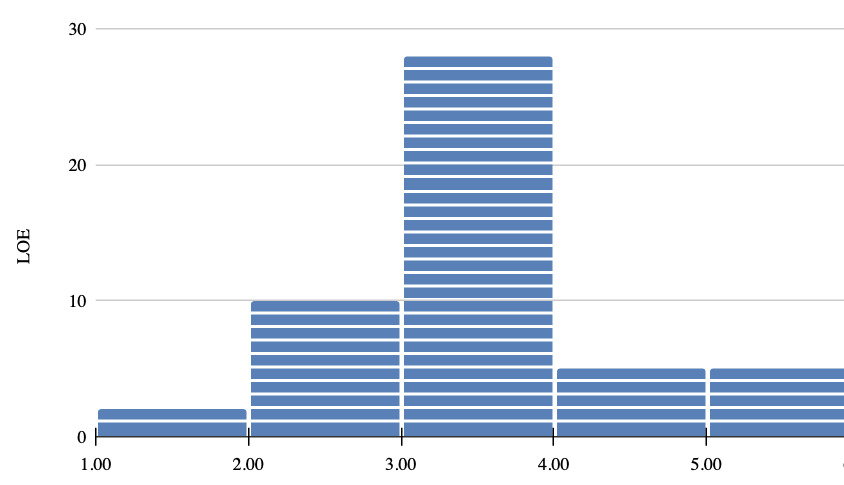
Of the 50 articles analyzed, most publications met criteria for Level III (n=28, 56%) in terms of Level of Evidence (LOE) [Figure 6]. Two publications were classified as a Level I publication. There were 10 Level II publications, four Level IV publications and four Level V publications, creating a rather “normal” statistical distribution of data [Figure 6]. There were not any publications in the study that were unable to be assigned an LOE. In terms of categorization of the publications, the most common article category was Clinical Outcomes (n=34). Clinical Guidelines was the second most common category with 12 publications. Unique categories pertaining to outpatient total joint replacement included Economics, contributing six publications, and Perceptions, contributing four publications [Figure 7]. Only two publications were not applicable to our classification system (Shah, Roshan P. et al and Warren, et al), which discussed the surgeon’s increased burden of care and a geographical analysis, respectively. Of note, some publications spanned two categories. Those which spanned two categories were included in the total count, once for each classification.
The three most cited articles in this study described Clinical Outcomes. The most cited article was “Outpatient total knee arthroplasty with a minimally invasive technique,” (2005) by Berger et al.. The study published outcomes from a specific minimally invasive TKA technique. “Otto Aufranc Award: A Multicenter, Randomized Study of Outpatient versus Inpatient Total Hip Arthroplasty,” (2017) by Goyal et al., was the second most cited article in the top 50. The authors of this study conducted a randomized trial to evaluate clinical outcomes of patients undergoing THA who are discharged on the same day as the surgery compared with those who are discharged after an overnight hospital stay. Furthermore, the 2017 article by Courtney et al., titled " Complications Following Outpatient Total Joint Arthroplasty: An Analysis of a National Database," was the third most cited article in this study. This study provided guidelines by determining the complications associated with outpatient total joint arthroplasty (TJA) and identifying high-risk patients they thought should be excluded from these protocols.
After ranking the articles in the top 50 based on the number of citations accrued per year since their publication, rather than total citations, the two publications by Goyal et al and Courtney et al, were both in the top three. However, the 2005 article by Berger et al., “Outpatient total knee arthroplasty with a minimally invasive technique,” was not in the top 10 based on citations per year, accruing 9.2 citations per year, likely due to it being slightly ahead of its time and being published 12 years before the peak of research on this topic. Every article in the top 10 ranked in order of citation per year was published in 2016 or later [Table 3].
Discussion
By performing a bibliometric review on “Outpatient Total Joint Replacements” this study aimed to identify the articles that have been most influential in this field of orthopaedic surgery. While total number of citations is not the only metric which determines the influence of a publication, it does provide a frame of reference for that article’s recognition in literature. To further substantiate the data acquired in this paper, different metrics were measured to gauge the characteristics and trends seen in the literature. Similar studies have been performed for topics such as total ankle arthroplasty, cervical myelopathy, and elbow surgery.8–10
Despite being a newer concept in joint replacement surgery, it has pick up a lot of traction over the decade, Outpatient Total Joint Arthroplasty has become a hot topic in orthopaedic journals. Possibly because the procedure has seen a significant increase in feasibility and popularity in the last ten years, even more so in the last five years, and the literature reflects this well. Given that Total Joint Arthroplasty is a well established and well tolerated procedure, the logical progression of transitioning lower-risk cases to the outpatient setting achieves a myriad of goals with respect to patient satisfaction and the overall burden on the healthcare system.
Another factor that may be playing into the rapidly growing popularity of outpatient total joints is the ever-evolving changes seen in physician reimbursement. A 2020 study by Lopez et al, demonstrated that despite an increase in TJA volume and utilization, there has been a steady decline in surgeon reimbursement accompanied with significant increases in hospital payments and charges.11 Part of the reason for the disproportionate increase in hospital charges compared to surgeon reimbursement is the cost of inpatient services which has increased 18.6% since 2012. Therefore, there is great appeal to conducting TJA’s in an ambulatory setting to curb the financial burden associated with inpatient services.
Additionally, the COVID-19 pandemic may have put forth an unforeseen pressure pushing TJA’s to the outpatient setting. The 2021 study by Chen et al, sought to explore the kind of impact that the COVID-19 pandemic had on different aspects of TJA’s via a comprehensive and scoping review of relevant publications. The authors of the study highlighted the importance of outpatient surgery, notably to minimize costs while improving the value of care.12
The outpatient total joint replacement research scene is primarily dominated by newer publications from 2016 onward, but a dichotomy of “newer” and “older” still exists, given that the most cited paper in the field is one of the oldest, from 2005. Our study elucidates this rather clearly. When the top 50 list was ranked in terms of total citations, eight out of the top 10 were from 2016 or later whereas the other two were from 2005 and 2007 respectively. When the top 50 list was ranked in terms of citations per year, all 10 articles were published in 2016 or later.
After analysis of each article’s classification in the top 50 most cited works, it is clear that Clinical Outcomes has been the most desired genre of outpatient total joint replacement research. This is likely due to the newer nature of the idea of outpatient total joint replacement and reflects the surgical community’s desire to prioritize patient safety when considering a change in practice patterns. Our data demonstrated that articles pertaining to Clinical Outcomes occupied 68% of the top 50. Additional unique categories included Economics and Perceptions, which have undoubtedly driven part of the transition of total joint replacement to the outpatient setting. Additionally, it stands to reason that a classification such as “Surgical Technique” might not be as heavily cited in this topic (only once), as there typically isn’t a major change in surgical technique, but a combination of protocols and patient optimization, depending on the setting of total joint replacement. As mentioned, certain publications received more than one category depending on overlapping themes.
The Level of Evidence (LOE) distribution for these articles was rather normal [Figure 6], with the obvious mode being Level III evidence, comprised mainly of retrospective studies. In comparison to other, similar, bibliometric reviews, this seems to be a trend in the literature. The authors understand that, pragmatically, retrospective studies are essential to the literature in order to get out quality data in a reasonable timeframe; especially in something so safe, effective, and rapidly popular as outpatient total joint replacement, but it call the attention that further prospective level I and II studies are needed for better understanding of it.
Unsurprisingly, hip and knee replacements continue to dominate the discussion, likely due to sheer volume and demand. However, it is worth noting that ankle, elbow and especially shoulder replacements were excluded from this study, but this is an excellent sign of progress in the outpatient total joint replacement space.
As with all research, there are inherent limitations to bibliometric reviews. The most obvious limitation in this study is the lower number of citations of these publications compared to other major topics in orthopaedics. However, due to the newer nature of the field, it is reasonable to expect further investigation requiring long-term increases in citation of many of these cornerstone papers. Another limitation is in the smaller pool of publications the authors were able to pick from, n=170. To ensure our results were specific to outpatient total joint replacement, and not tangential to the focus of the study, more narrowly focused search terms were used. To ensure crucial papers were not missed, many different iterations of the final search were used to rule out gross negligence. However, it is critical to understand that search terms, search engine and user error may all contribute to errors of omission with respect to this review.
Conclusion
This study provides a comprehensive and objective measure of the most cited articles on outpatient arthroplasty. Most of the literature on the topic were categorized as Clinical Science and Outcomes (50%), comprised level of evidence III (28%), were published in the Journal of Arthroplasty (54%) and came out of the United States (76%). Knowledge of these most influential articles allows for a foundation of understanding on a rapidly growing area of arthroplasty among clinicians.
Conflict of Interests
The authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article. There are no relevant disclosures. We have no conflicts of interest. The Manuscript submitted does not contain information about medical device(s)/drug(s). All authors significantly contributed to the document and have reviewed the final manuscript.