Introduction
Over the last few years, increasing attention has been devoted to the assessment of hamstring graft preparation for ACL reconstruction. Clinical outcomes of reconstructive surgery have dramatically improved following an increased knowledge of anatomy and the biomechanics of native ACL.1–4 The most important advances in ACL reconstructive surgery passed from anatomic studies of the double-bundle concept to the anatomic position of the graft during reconstruction.5 In addition, graft fixation systems were implemented allowing an increased solid fixation and making the surgical reconstructive procedure easy and reproducible.6 However, controversies still exist concerning different topics such as tunnel placement and biological integration. The type of graft and the way of preparing it before implantation represents another crucial changing topic. Concerning graft, hamstring tendon (HT) and patellar tendon (PT) have shown good clinical results with no clear and strong evidence in favor of one or the other graft type.7 While PT graft preparation is standardized, for hamstring tendon graft different suturing techniques8 and methods of preparation such as the four-strand graft, tripled ST graft, ST quadruplication has been proposed in recent years, to create an adequate graft diameter reducing morbidity linked to gracilis tendon harvesting procedure.9
The present study aims to describe different options of hamstring graft preparing, listing and analyzing each configuration to help surgeons to choose the most suitable graft type for their patients.
Suturing the graft
During ACL reconstructive surgery the graft is usually sutured in a different fashion. Graft suturing could be performed at different levels of the graft, trying to leave it free from the suture at the level of the intra-articular portion. This is commonly performed by surgeons to avoid permanent synthetic material in the joint space. Suturing the graft’s free ends allows to handle the graft during the final tibial fixation, ensuring graft tensioning during final fixation by using an interference screw. Furthermore, it allows to tubularize the graft and to obtain the correct graft diameter, required for its tunnel transfer. In addition, suturing the free ends of the graft could be useful for the surgeon for tibial post-fixation. The graft could be prepared by extending the suture from the free end to the tibial graft portion thus increasing graft fixation strength because of the engagement of the threads of the interference screw with the suture. However, permanent viscoplastic elongation of the graft could be observed, due to slippage of the suture within the tendon tissue during loads. For this reason, graft suturing should be performed with a good amount of tension of the graft. It should be note that, although this effect has been described, no clinical real implications have been demonstrated. After graft configuration, the femoral portion of the graft could be left free or sutured preventing graft sliding on the femoral fixation device during pulling from the tibial side.10,11
Suturing techniques
To date, several suturing techniques have been described and used by surgeons for graft preparation.12,13 No. 2 braided non-absorbable FiberWire (Arthrex), UltraBraid (Smith & Nephew) and force fiber (Stryker) are usually used and passed through the tendon with different configurations using a curved needle. The most popular suture techniques are the Krackow stitch, the baseball stitch and the whipstitch. They consist in passing the suture with a different configuration through the tendon using a needle. Although these suture techniques are widely used, potential disadvantages have been reported such as possible graft damages and permanent viscoplastic elongation of the graft due to slippage of the suture within the tendon tissue during load.14,15 Furthermore, passing a suture through the tendon is relatively time-consuming and it could increase the duration of the surgery.13
For these reasons, different authors advocate the use of grasping suture techniques rather than locking suture techniques with the main advantage of a faster graft preparation and an increase in the suture-tendon interface surface area.15 The most common grasping suture technique is the modified finger-trap (MFT)suture technique. It consists to tie the suture over the graft with a criss-cross suture pattern, allowing the surgeon to constrict the graft when tension is applied to the sutures. In order to prevent slippage of the crosshatch suture from the end of the tendon graft during loading, an additional final rolling-hitch suture is applied.16 The main advantages of this suture technique are the increased suture-tendon interface surface area and a faster graft preparation. Furthermore, the MFT is potentially faster for graft preparation.8 Although the MFT-graft construct has previously been studied and compared with other suture techniques, to our knowledge no data is present regarding the merit of the MFT to reduce the overall surgical time of ligament reconstruction.17
Graft Configuration
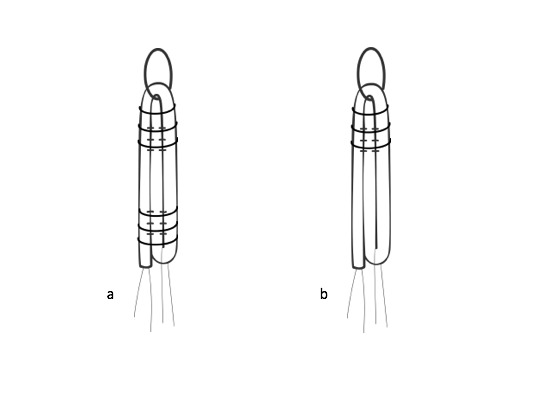
Four-Strand Graft Preparation
The four-strand graft (Figure 1 a, b) represents the most common technique used among surgeons. This configuration could be used when cortical fixation systems are used as well compression (absorbable screws), expansion and cancellous suspension systems. The free ends of each tendon are whipstitched with a high-strength nonabsorbable suture, trying to equalizing both the ends of the graft. At this point, tendons should be twisted in a reverse orientation so that the proximal end of the ST is adjacent to the distal end of the GR and vice versa.18 Then, the graft is loaded in a cortical suspensory device. If compression or cortical femoral fixation system is used, all tendon strands could be suture at the level of the femoral intra-tunnel graft portion.19 This could allow an increased screw tightness and a better load sharing between all four limbs of the graft at the time of tibial fixation. When femoral cross-pin fixation technique is used, suturing the looped-over part of the tendons could provide increase biomechanical graft fixation properties.16,20 Independently from the femoral fixation system used, absorbable screws or staples are generally used in the tibial side for the final fixation. Adequate graft length could allow a post-fixation with screw or washer in the tibial side.
Tripled Graft
The main advantage of the use of a tripled ST graft (Figure 2 a, b) construct is to avoid the use of the gracilis tendon, which could be preserved as secondary stabilizer reducing flexion strength loss and preserving rotatory stability of the knee. Further, gracilis tendon could be used as a further graft in case of multiligament reconstruction.21 A tendon length greater than 240 mm allow to obtain a graft length of at least 80 mm, allowing the use of an adjustable-length loop cortical button fixation in the femoral side and an interference screw in the tibial side. The tendon could be tripled following different fashions such as S or circle configuration. Tendon’s ends are whipstitched and the graft is divided into 3 equal parts. One-third of the tendon is loaded in the suspensory device, while the free-limb is reversed and sutured to the other strands. During this phase, the third free limb should be rigidly fixed to other limbs using a high-strength non-absorbable suture to created a resistant graft that resists elongation during loads. The suture should be also passed at the distal end of the graft. Concerning biomechanics, conflicting results are reported in literature, depending from a possible different contribute of the third limb to the tension of the final tripled graft.
Quadrupled Semitendinousus Graft Preparation
The semitendinousus tendon could be quadrupled to increase graft diameter and it can be used if gracilis tendon is required for other procedures such as multi-ligament reconstruction.20 The main indication of the use of quadrupled ST is represented by an all-inside reconstruction with half-tunnels placed in both femoral and tibial sides and a total semitendinousus length of at least 240 mm. In fact, this procedure requires a short graft with a length of about 60-70 mm. The graft could be prepared by passing the ST tendon through an adjustable tibial fixation device, suturing its 2 free ends together with a high-strength suture. Free ends are sutured and then passed through the loop of a femoral suspensory adjustable-length device, quadrupling the final graft. The femoral and tibial intra-tunnel portion of the graft is sutured in a circumferential fashion, locking all 4 strands and placing a knot into the center of the strands. A bigger suture diameter should be used during graft preparation to ensure safe graft stability and to avoid a cutting through the tendon that could occur during loads and post-operative rehabilitation.22 Different studies have evaluated the biomechanics behavior of the quadrupled ST, concerning different tibial fixation methods and to the sutures used to secure two free limbs to the remnant tendon. Recently Mayr et al.23 observed an increased quadrupled ST graft elongation during loads when a tibial adjustable-length loop cortical button fixation was used in place of an interference screw. Pailhé et al24 found that ST4 had a significantly higher failure load than the other grafts such as patellar tendon and four-strand GR and ST.
Five-Strand Graft Preparation
The main advantage of the use of a five-strand graft is an increased graft diameter (Figure 3). This could be helpful in a specific situation such as a four-strand graft (GR + ST) with an overall diameter less than 7-8 mm. If small-diameter hamstring tendons are harvested, creating a five-strand graft could increase the overall graft diameter of 1-1,5 mm, reducing the risk of postoperative graft failure.25 Another advantage is represented by an adequate total graft length that can allow a tibial fixation using an interference screw. Even these theoretical advantages are reported, no clear biomechanical effect has been demonstrated. Specifically, no advantages in terms of graft elongation were observed comparing four-strand and five-strand graft, even an increased stiffness of the five-strand graft was observed during cyclic load.26
During graft preparation, each tendon ends should be separately whipstitched with no. 2 non-absorbable sutures. At this point, the gracilis is duplicated around a cortical button femoral fixation system. Similarly, the ST is triplicated creating a five-strand graft looped around the suspensory device. The femoral portion of the graft should be sutured having the care to reach each limb to secure the third limb of the tripled ST and to better load sharing between all five limbs of the graft at the time of tibial fixation.
Six-Strand Graft Preparation
Using autograft tissue, GR and ST could be prepared together to obtain sufficient graft diameters (>8mm). The six-strand graft27 preparation technique allows for all strands of the graft to be suspended over a rigid cortical fixation system on both femur and tibia sides. The ST is folded twice to create a 4-strand graft that can be sized with the sizing tubes. If the graft diameter is <8mm, the GR could be added to the 4-strand ST graft. The GR tendon is passed through the cortical femoral fixation loop at the femoral end of the graft and tensioned over the 4-strand ST, creating a 6-strand construct. On both femoral and tibial sides of the graft, a high-strength non-absorbable suture is then placed 20 mm from the end of the graft, taking care to include the suture on each strand. The main advantage of this graft configuration is that it allows the creation of a graft of adequate diameter. However, a cortical fixation on the femur and tibia side is required. For this reason, a retro-construction of the tibial tunnel is required on both femur and tibia.
Contributions
The authors contribuited equally.
Conflict of interests
The authors declare no potential conflict of interest
Funding
The authors received no financial support for the research and /or authorship of this article